Oral Pathology
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Pronounce, define, and spell the Key Terms.
• Explain why oral pathology is important for the dental assistant.
• Explain why categories of diagnostic information are necessary.
• Describe the warning symptoms of oral cancer.
• Describe the types of oral lesions.
• Name five lesions that are associated with HIV/AIDS.
• Describe the appearance of lesions associated with the use of smokeless tobacco.
• Describe three conditions associated with the tongue.
• Identify two oral conditions related to nutritional factors.
• Recognize developmental disorders of the dentition.
• List and define three anomalies that affect the number of teeth.
• List and define five anomalies related to the shape of the teeth.
• Define, describe, and identify the developmental anomalies discussed in this chapter.
• Describe the oral conditions of a patient with bulimia.
• Describe the classic signs of inflammation.
Electronic Resources
![]() Additional information related to content in Chapter 17 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 17 can be found on the companion Evolve Web site.
Key Terms
Abscess (AB-ses) Localized area of pus originating from an infection.
Acute inflammation Minimal and short-lasting injury to tissue.
Biopsy (BYE-op-see) Removal of tissue from living patients for diagnostic examination.
Candidiasis (kan-di-DYE-i-sis) Superficial infection caused by a yeastlike fungus.
Carcinoma (kahr-si-NOE-muh) Malignant tumor in epithelial tissue.
Cellulitis (sel-yoo-LYE-tis) Inflammation of cellular or connective tissue.
Chronic inflammation Continuous injury or irritation to tissue.
Congenital (kun-JEN-i-tul) disorders Disorders that are present at birth.
Cyst (sist) Closed cell or pouch with a definite wall.
Ecchymosis (ek-i-MOE-sis) Technical term for bruising.
Erosion Wearing away of tissue.
Glossitis (glos-EYE-tis) Inflammation of the tongue.
Granuloma (gran-yoo-LOE-muh) A granular tumor or growth.
Hematoma (hee-muh-TOE-muh) Swelling or mass of blood collected in one area or organ.
Inflammation Protective response of the tissues to irritation or injury.
Lesion (LEE-zhun) An area of pathology.
Leukemia (loo-KEE-mee-uh) A progressive disease in which the bone marrow produces an increased number of immature or abnormal white cells.
Leukoplakia (loo-koe-PLAY-kee-ah) Formation of white spots or patches on the oral mucosa.
Lichen (LI-kun) planus Benign, chronic disease that affects the skin and oral mucosa.
Lymphadenopathy (lim-fad-uh-NOP-uh-thee) Disease or swelling of the lymph nodes.
Lymphoma (lim-FOE-muh) Malignant disorder of the lymphoid tissue.
Metastasize (muh-TAS-tuh-size) To spread (disease) from one part of the body to another.
Methamphetamine Potent central nervous system stimulant.
Meth mouth Informal name for the rampant tooth decay caused by heavy methamphetamine use.
Pathology (pa-THOL-uh-jee) The study of disease.
Petechiae (pe-TEE-kee-uh) Small, pinpoint red spots on the skin or mucous membrane.
Sarcoma (sahr-KOE-muh) Malignant tumor in connective tissue such as muscle or bone.
Tori (TOR-eye, TOR-ee) Abnormal growths of bone in a specific area.
Xerostomia (zeer-oe-STOE-mee-uh) Dryness of the mouth caused by reduction of saliva.
Oral pathology is the study of diseases in the oral cavity. Only a dentist or a physician may diagnose pathologic (disease) conditions, but it is important for the dental assistant to be able to recognize the differences between normal and abnormal conditions that appear in the mouth. For example, while taking radiographs or impressions, the dental assistant might notice a lesion in the patient’s mouth that appears abnormal. Then, the dental assistant would inform the dentist so that a diagnosis could be made.
Many systemic diseases, as well as infectious diseases, have oral manifestations (signs and symptoms). The dental assistant should understand how oral abnormalities affect the patient’s general health and planned dental treatment.
Before you can recognize abnormal conditions in the mouth, you must have a solid understanding of the appearance of normal oral conditions. You might want to review the appearance of normal oral tissues in Chapter 10.
As a dental assistant, you should understand the terms used to describe pathologic conditions and should record preliminary identification and descriptions of lesions. You should use these terms in the clinical setting so that they become part of your everyday professional vocabulary. You then can communicate effectively with other professionals.
In addition to pathologic conditions, this chapter presents conditions that are variations of normal but are not considered pathologic.
Making a Diagnosis
Making an accurate diagnosis is much like putting a puzzle together—many pieces are necessary. To make an accurate diagnosis, the dentist must rely on a variety of types of information. Remember, one piece of information alone usually is not enough to make a diagnosis. Eight sources of information can be used to make a final diagnosis. These include historical, clinical, radiographic, microscopic, laboratory, therapeutic, surgical, and differential findings. Imagine each of these findings as a piece of a puzzle that leads to diagnosis.
Historical Diagnosis
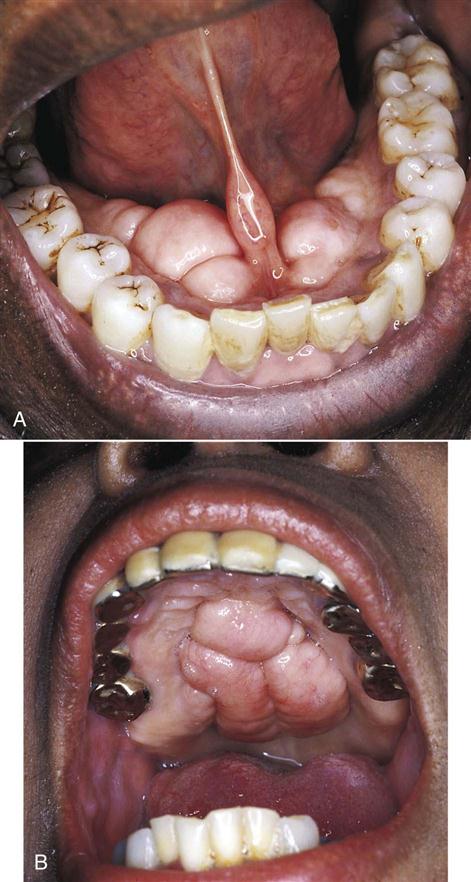
Personal history, family history, medical and dental histories, and history of the lesion are often useful in making a diagnosis. Family histories are important because of genetic disorders such as dentinogenesis imperfecta (Fig. 17-1). Melanin pigmentation of the gingiva is common in dark-skinned individuals (Fig. 17-2). Medical histories can provide information about medication the patient may be taking that could have an effect on the oral tissues.
Clinical Diagnosis
A clinical diagnosis is based on the clinical appearance of the lesion, including the color, size, shape, and location. Examples of conditions diagnosed on the basis of clinical appearance are fissured tongue (Fig. 17-3), maxillary and mandibular tori and torus palatinus (Fig. 17-4), and median rhomboid glossitis (Fig. 17-5).
Radiographic Diagnosis
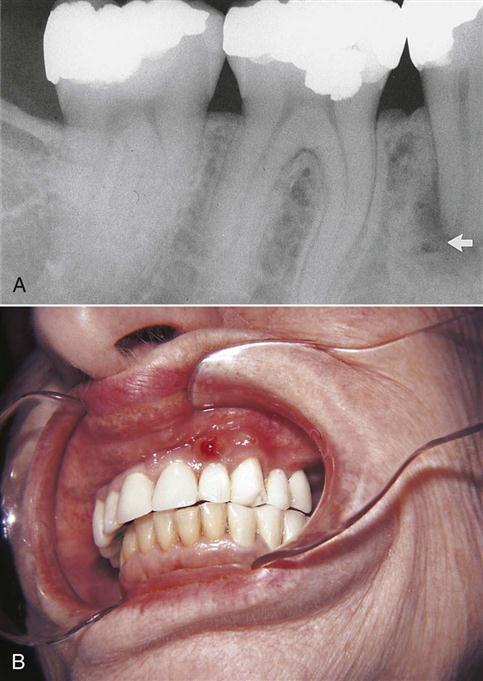
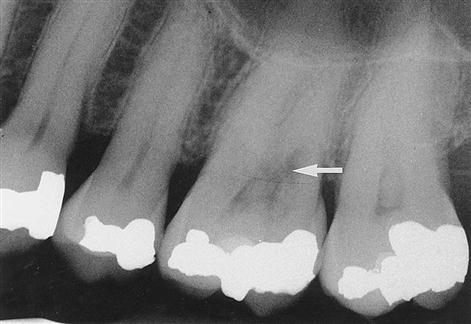
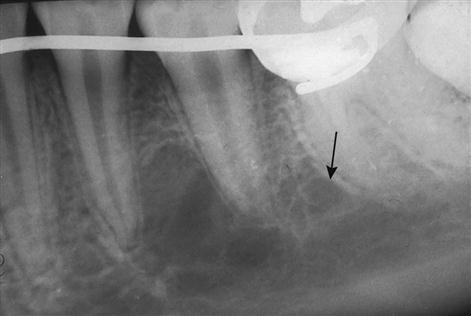
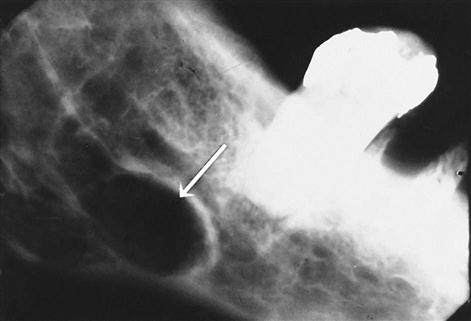
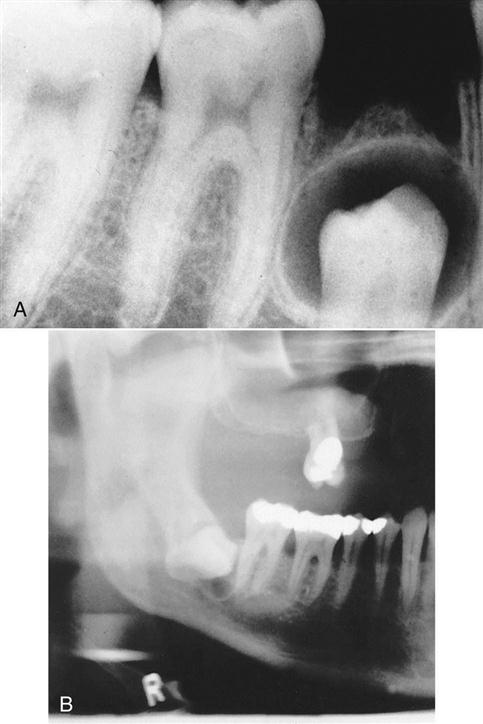
Radiographs are excellent in providing information about periapical pathology (Fig. 17-6), internal resorption (Fig. 17-7), and impacted teeth (Fig. 17-8).
Microscopic Diagnosis
When a suspicious lesion is present, tissue is removed from the lesion and is sent to a pathology laboratory, where it is evaluated microscopically (called biopsy). This procedure is very often used to make the definitive (final) diagnosis. For example, a white lesion cannot be diagnosed on the basis of clinical appearance alone. A biopsy must be performed to determine whether or not the lesion is malignant (Fig. 17-9).
Laboratory Diagnosis
Blood chemistries and other laboratory tests, including urinalysis, can provide information that leads to a diagnosis. Cultures done in the laboratory can be used to diagnose types of oral infection.
Therapeutic Diagnosis
Therapeutic diagnosis is made by providing a treatment (therapy) and seeing how the condition responds. For example, angular cheilitis (Fig. 17-10) may be caused by lack of the B-complex vitamins, or it could simply be a fungal infection. If angular cheilitis improves after the patient is given an antifungal cream, the vitamin deficiency theory can be ruled out.
Surgical Diagnosis
A diagnosis is made on the basis of findings from a surgical procedure. For example, on a radiograph, a traumatic bone cyst (Fig. 17-11) looks like a static bone cyst (Fig. 17-12). However, one condition would require treatment, whereas the other would not. Surgically opening the area and inspecting it would reveal whether the radiolucency on the radiograph was indeed a condition that required further treatment.
Differential Diagnosis
When two or more possible causes of a condition are identified, a differential diagnosis must be made. The dentist will determine which tests or procedures should be done to rule out the incorrect cause and make a final diagnosis.
Acute/Chronic Inflammation
Inflammation is the body’s protective response to irritation or injury. The inflammatory response is determined by the extent and duration of the injury. Inflammation can be acute or chronic. For example, acute inflammation occurs if injury to the tissue is minimal and short-lasting and the tissue begins to repair quickly. Chronic inflammation occurs when injury or irritation to the tissue continues. Inflammation of a specific tissue is described by the suffix –itis added to the name of the tissue (e.g., gingivitis, periodontitis, pulpitis). Refer to Chapter 14 for a discussion of gingival and periodontal inflammatory diseases.
Oral Lesions
Lesion is a broad term for abnormal tissues in the oral cavity. A lesion can be a wound, a sore, or any other tissue damage caused by injury or disease. It is important for the clinician to identify the type of lesion to make a diagnosis. Lesions of the oral mucosa are classified as to whether they extend below or extend above the mucosal surface, and whether they lie flat or even with the mucosal surface.
Lesions Extending Below Mucosal Surface
An ulcer is a break in the mucosa that looks like a punched-out area, similar to a crater. An ulcer may be as small as 2 mm or as large as several centimeters.
An erosion of the soft tissue is a shallow injury in the mucosa caused by mechanical trauma, such as chewing. (Trauma means wound or injury.) The margins may be ragged and red and quite painful.
An abscess is a collection of pus in a specific area. Abscesses are commonly found at the apex of a tooth (periapical abscess). An abscess may be caused by bacteria in a badly decayed tooth or by bacteria resulting from a severe periodontal infection (see Chapter 14).
A cyst is a fluid or semisolid, fluid-filled sac. The material within the cyst is not always infectious. In dentistry, a cyst may form around the crown of an unerupted tooth (Fig. 17-13).
Lesions Extending Above Mucosal Surface
Blisters, also known as vesicles, are filled with a watery fluid. (They look like the blisters that appear on feet as a result of poorly fitting shoes.) They are rarely seen in the oral cavity because they tend to rupture, leaving ulcers with ragged edges.
A pustule looks like a blister, but it contains pus. A hematoma is also similar to a blister, but it contains blood.
A plaque is any patch or flat area that is slightly raised from the surface. (Note: This is not the same as dental plaque, which is discussed in Chapter 13.)
Lesions Even With Mucosal Surface
These lesions lie flat or even with the surface of the oral mucosa and are well-defined areas of discoloration. An ecchymosis, which is the medical term for bruising, is an example of this type of lesion.
Raised or Flat Lesions
Nodules, which may appear below the surface or may be slightly elevated, are small, round, solid lesions. When palpated, a nodule feels like a pea beneath the surface.
Granuloma is a term with many meanings. In dentistry, it is often used to describe a type of nodule that contains granulation tissue. (The suffix –oma means tumor or neoplasm.) A granuloma may appear on the gingival surface as a swollen mass. It also may be located within the bone as a periapical granuloma at the apex of a nonvital tooth.
Tumors are also known as neoplasms. A tumor is any mass of tissue that grows beyond the normal size and serves no useful purpose. A tumor may be benign (not life threatening) or malignant (life threatening).
Diseases of the Oral Soft Tissues
Leukoplakia
Leukoplakia is a general term that means “white patch.” It may occur anywhere in the mouth. Very little pain is associated with leukoplakia unless ulceration and secondary infection are also present.
The lesions vary in appearance and texture from a fine, white transparency to a heavy, thick, warty plaque. To be classified as leukoplakia, the lesion should be firmly attached to the underlying tissue, and rubbing or scraping with an instrument should not remove it.
The cause of leukoplakia is unknown, but the presence of this disease is often linked to chronic irritation or trauma. Such injury may result from the use of smokeless tobacco, poorly fitting dentures, or cheek biting (Fig. 17-14).
Leukoplakia often appears before a malignant lesion develops, so early diagnosis and treatment are important.
Lichen Planus
Lichen planus is a benign, chronic disease that affects the skin and oral mucosa. Many factors have been implicated in lichen planus, but the cause remains unknown.
On the oral mucosa, the patchy white lesions exhibit a characteristic pattern of circles and interconnecting lines called Wickham’s striae (Fig. 17-15). A second type of lichen planus can cause erosive lesions on the gingiva. This type of lesion tends to worsen with emotional stress.
Candidiasis
Candidiasis is a superficial infection caused by the yeastlike fungus Candida albicans. It is the most common oral fungal infection, but it does not usually occur in the healthy general population.
Candidiasis can result from antibiotic therapy, diabetes, xerostomia (dry mouth), and weakened immunologic reactions. It also may be the initial clinical manifestation for patients with acquired immunodeficiency syndrome (AIDS; see later discussion in this chapter).
Candidiasis is accompanied by discomfort or pain, halitosis (unpleasant breath odor), and dysgeusia (distorted sense of taste). Diaper rash, vaginitis, and thrush are other common types of candidiasis.
Pseudomembranous Candidiasis
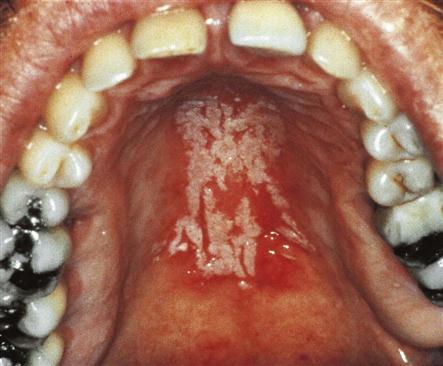
In pseudomembranous candidiasis, also known as thrush, creamy white plaques (resembling cottage cheese or curdled milk) form in the mouth (Fig. 17-16). The patient frequently describes a burning sensation, an unpleasant taste, or the feeling of “blisters forming in the mouth.” These “blisters” generally prove to be the pseudomembranous plaques. (Pseudomembranous is a term that describes a false membrane or tissue.)
The plaques can be scraped off, and they rarely bleed when they are removed. When bleeding does occur, the patient likely has an additional mucosal problem. When this condition is seen in babies, it is called infantile candidiasis.
Hyperplastic Candidiasis
Hyperplastic candidiasis appears />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses