Chapter 17
Clinical epidemiology
Introduction
A case scenario
- How sure can you be of the diagnosis?
- What caused the pulp necrosis?
- Is periapical inflammation a common finding?
- What factors are associated with an increased risk?
- What is the probability that the suggested treatment will cure the disease?
- Will my general health be compromised if the tooth is not treated?
- How long can a root filled tooth be retained?
To answer these questions and predict what will happen in this specific case you have to rely on various sources of information: basically on the dental scientific literature, but also on your own experiences and information and advice of colleagues. In this chapter you will find an overview of relevant data found in the scientific literature.
Clinical epidemiology
From a conceptual point of view endodontic treatment might be regarded as a set of procedures used to either prevent or treat apical periodontitis (AP) (58). Thus, the treatment of a case with pulpitis is considered to be successful if the treatment prevents AP from developing. Accordingly, the treatment of a case with an infected necrotic pulp and periapical inflammation is considered successful if, after a healing period there are no clinical or radiographic signs of AP.
With this conceptual model in mind it becomes important to study the prevalence, incidence and healing of AP in various populations, and to identify factors that influence these parameters. Such studies enable us to make predictions about individual patients. The science based on studies of groups of patients to ensure that the predictions are valid is called clinical epidemiology (26). Clinical epidemiology seeks to answer important clinical questions using methods developed by epidemiologists (Core concept 17.1).
Epidemiological methods
Epidemiology is the study of factors affecting the health and illness of populations and is of fundamental importance when interventions are to be made in the interest of public health and preventive medicine. It is considered a basic methodology of public health research and is highly regarded in evidence-based medicine for identifying risk factors for disease. Furthermore, epidemiology is essential to establish optimal treatment approaches in clinical practice. Epidemiological studies are generally based on samples of populations. Populations are large numbers of people in a defined setting (e.g. Denmark or the county of Västra Götaland in Sweden) or with a certain trait or characteristic (e.g. AP or root filled teeth). For practical reasons it is usually impossible to examine every individual in the population, therefore a sample or a subset of the population is selected. In the selection of the material and registration of data the investigator has to control for bias. Bias is defined as ”a process at any stage of inference tending to produce results that depart systematically from the true values” (52). Bias in relation to selection of patients is called selection bias and bias in relation to collection and registration of data is called information bias.
| Population: | Large group of people in a defined setting |
| Sample: | Subset of a population |
| Bias: | A process at any stage of inference tending to |
| produce results that depart systematically from | |
| the true values (selection, measurement, | |
| confounding) | |
| Exposure: | Any agent or factor that is thought to cause |
| disease | |
| Outcome: | The measure of disease occurrence |
| Prevalence: | The total number of present cases at a given |
| point of time | |
| Incidence: | The number of new cases that appear over a |
| given period of time | |
| Risk: | The probability of some untoward event (the |
| outcome) | |
| Risk factors: | Characteristics that are associated with an |
| increased risk of becoming diseased | |
| Prognosis: | Prediction of the future course of disease |
| Prognostic factors: | Conditions that are associated with a given |
| outcome of the disease | |
| Odds: | Ratio between two probabilities |
| Odds ratio: | Ratio of disease when exposed relative to ratio |
| of disease when unexposed | |
| Relative risk: | Risk of disease when exposed relative to risk of |
| disease when unexposed |
Another problem that may appear in epidemiological research is confounding. A confounding variable is associated with both the probable cause and the outcome, but is not included in the chain of cause and effect. For example it is known that smoking may cause larynx cancer, and it is known that smoking is frequent among individuals with heavy consumption of alcohol. If we want to estimate the effect of alcohol on larynx cancer, of course we then have to adjust for the confounding variable “smoking”.
Epidemiologists use different types of study designs with varying levels of evidence. In dentistry the most frequently used are case series, which also represent the lowest level of evidence, followed by cross-sectional studies, case–control studies, cohort studies and eventually experimental studies (randomized controlled trials) which represent the highest level of evidence.
In a case series study a number of cases are collected in an ad hoc manner and the experience of a group of patients with a similar diagnosis or treatment is described. The sample is not necessarily drawn from a well-defined population. For example, teeth treated for pulpectomy in a certain clinic are followed over a period of time (often 2–4 years). At the end of the period the number of ” successful” treatments (no symptoms or signs of AP) and number of ”failures” (signs of AP) are registered. This type of study is rather common in endodontology. The classic study published by Strindberg (75) is a good example of a case series. Case series are mostly used to generate hypotheses that can be explored in other study models, since generalization is seldom justified.
In cross-sectional studies the prevalence (person-level) and frequency (tooth-level) of AP may be estimated, and risk indicators associated with the presence of AP may be identified. In this study design a sample of a well-defined population is examined at a specific moment in time. To assess the magnitude of a problem in a population, all individuals may be examined one by one, or a representative sample of the total population may be drawn. Often the latter is chosen because it is the most cost-efficient method to retrieve an estimate of the disease prevalence. The possibility of generalizing from the results therefore depends on how representative the study population is. During the last 20 years several cross-sectional studies addressing endodontic status in various countries have been performed (for an overview see Ref. 30). Sometimes cross-sectional studies are repeated, like the examinations of 35-year-olds living in Oslo, Norway. The investigation was originally carried out in 1973 and then repeated in 1984, 1993 and 2003 (73). Obviously each sample consists of different individuals and such a study design allows researchers to monitor population trends.
In a case–control study cases are selected according to outcome and within a well-defined population. Controls are individuals who could have been cases if they had developed the disease. Thus they should be selected from the same population as the cases, during the same time period and independent of exposure status. Case–control studies are an efficient way of retrieving estimates on the risk of different exposures, but are vulnerable to information bias since participants must remember past exposures. This study design has infrequently been used in endodontic research.
In a cohort study or longitudinal study, a well-defined group of people sharing a common experience or condition is followed over time. The group may include both healthy and diseased individuals. Since it is the same individuals who are examined repeatedly, a cohort study could be used to estimate both incidence and healing rate of a disease. Furthermore, risk factors can be identified and quantified (22, 30, 42, 43, 59).
Randomized controlled trials (RCTs) are studies in which subjects are assigned on a random basis to participate in one group receiving one treatment or another group receiving another treatment. The study design ensures that known and unknown confounding factors are evenly distributed between treatment groups by random allocation of subjects. RCTs are considered the most reliable form of scientific evidence in health care, because they eliminate spurious causality and bias.
In the following we will try to find answers to the clinically important questions mentioned earlier. The approach is inspired by Fletcher and Fletcher (26).
Diagnosis
Question: How sure can you be of the diagnosis of AP?
Since AP is infrequently associated with clinical symptoms, most epidemiological studies are based on data obtained from radiographic images. As in all diagnostic systems the accuracy is not perfect and the unavoidable presence of false-positive and/or false-negative diagnoses must be carefully considered and a strategy chosen (see Chapter 14). In radiographically based surveys the presence or absence of AP is often related to the occurrence of carious lesions, the quality of the coronal restoration and various technical aspects of the root filling. However, the two-dimensional nature of conventionally obtained radiographic images may not reveal minor occlusal, buccal or oral carious lesions, and approximal caries may be detectable only when a certain degree of demineralization has occurred (32, 63). There are similar limitations when the quality of restorations is evaluated in the radiograph. On the other hand, approximal defects may be more readily detected radiographically than clinically.
When the technical quality of root fillings is classified, the seal against the canal wall and the distance from the end of the root filling to the radiographic apex of the tooth are usually assessed and measured. Several studies have pointed out the difficulties in defining and maintaining radiographic criteria for the quality of seal resulting in substantial intra- and interobserver variation. Forsberg (27) found that when the distance between the root filling and the apex was measured the paralleling technique was superior to the bisecting-angle method.
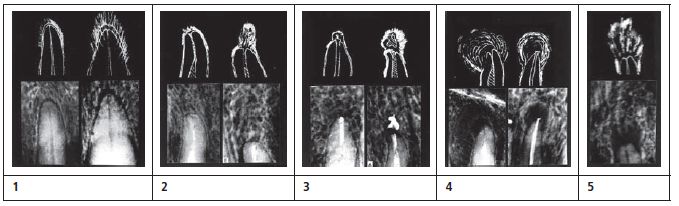
Many epidemiological investigations just report on the presence or not of AP (or more exactly, the presence or not of periapical radiolucencies). Strindberg (75) based a very influential system for evaluating the outcome of endodontic therapy on this idea. Ørstavik et al. (57) did a more detailed interpretation of the radiographic image and proposed a five-step score (from a healthy periapical bone to severe AP), the ”periapical index” (PAI). The PAI is based on original studies by Brynolf (11) in which she compared histology and radiography of periapical biopsy specimens (Key literature 17.1) Whatever system is used for radiographic diagnosis of AP there are obvious problems with the accuracy and a substantial body of studies has been concerned with observer variation, calibration and observer strategy. The theoretical background to observer variation and how such problems could be handled are discussed in more detail in Chapter 14.
The short answer: No diagnostic method is perfect and the risk of false-positive and false-negative diagnoses cannot be completely eliminated. However, in the clinical situation various diagnostic tests are combined and if radiographic signs of AP are found in combination with, for example, a negative pulp vitality test, the accuracy of the diagnosis is very good.
Cause
Question: What caused the pulp necrosis?
Pulp necrosis is most frequently preceded by pulpal inflammation and caries generally is regarded as the main etiological reason for pulpal injury and endodontic treatment (see Chapter 2). This notion was supported by data from a study by Bjørndal et al. (8), who sent a questionnaire to 600 randomly selected Danish general dental practitioners. The practitioners were asked to recall the reason for doing their last root filling. Caries in teeth with vital pulps were given as the reason for performing root canal treatment in 55% of the cases. Kirkevang et al. (43) performed a cohort study including 473 individuals with 12 443 teeth and found that teeth with primary caries had an increased risk of developing AP during a 5-year period (odds ratio = 2.9).
If the pulp resists a caries attack and survives there are several potential threats in the subsequent restoration of the crown. The use of rotary cutting instruments, leakage of bacterial elements along the margins of restorations and toxic effects of medicaments and materials used to restore cavities and cement crown and inlays may provoke pulpal inflammation and initiate processes that will lead to necrosis (see Chapter 2). Bergenholtz and Nyman (5) studied the effect prosthetic interventions might have on the pulp. They compared 255 abutment teeth and 417 non-abutment teeth in 52 patients treated for advanced periodontal disease. All pulps were initially diagnosed as vital and the observation period varied from 4 to 13 years (mean = 8.7 years). Pulpal necrosis (including periapical lesions) developed more frequently in abutment teeth than in non-abutment teeth (15% vs 3%). This finding was supported by a Danish cohort study where the presence of a filling as well as a crown increased the risk of developing AP, odds ratios being 2.8 and 7.9, respectively (43). Thus, pulp necrosis may be the result of repeated injuries that affect the pulp unfavorably.
- “Success” when (a) the contours, width and structure of the periodontal margin were normal, and (b) the periodontal contours were widened mainly around the excess filling.
- “Failure” when there was (a) a decrease in the periradicular rarefaction, (b) unchanged periradicular rarefaction, and (c) an appearance of new rarefaction or an increase in the initial.
- “Uncertain” when (a) there were ambiguous or technically unsatisfactory control radiographs which could not for some reason be repeated, or (b) the tooth was extracted prior to the 3-year follow-up owing to unsuccessful treatment of another root of the tooth.
The short answer: Necrosis often is the result of several accumulated injuries to the pulp. Even the most meticulous practitioner must expect some treated teeth to become necrotic.
Prevalence, frequency and incidence
Question: Is periapical inflammation a common finding?
Epidemiological studies on samples drawn from various populations demonstrate that AP is very common in adults. In the body of published data the prevalence of AP varies between 22 and 80% of the investigated individuals (Fig. 17.1), and the frequency of AP at tooth level is reported to be between 1 and 14% (Fig. 17.2).
Root fillings are frequently performed in Western countries and cross-sectional studies find 25–75% of individuals in various populations to have at least one root-filled tooth (30). Bjørndal and Reit (9) observed, despite the decreased caries prevalence, an increased number of endodontic treatments performed in Denmark between 1977 and 20/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


