Preimplant Prosthodontics
Overall Evaluation, Specific Criteria, and Pretreatment Prostheses
Carl E. Misch, Francine Misch-Dietsh
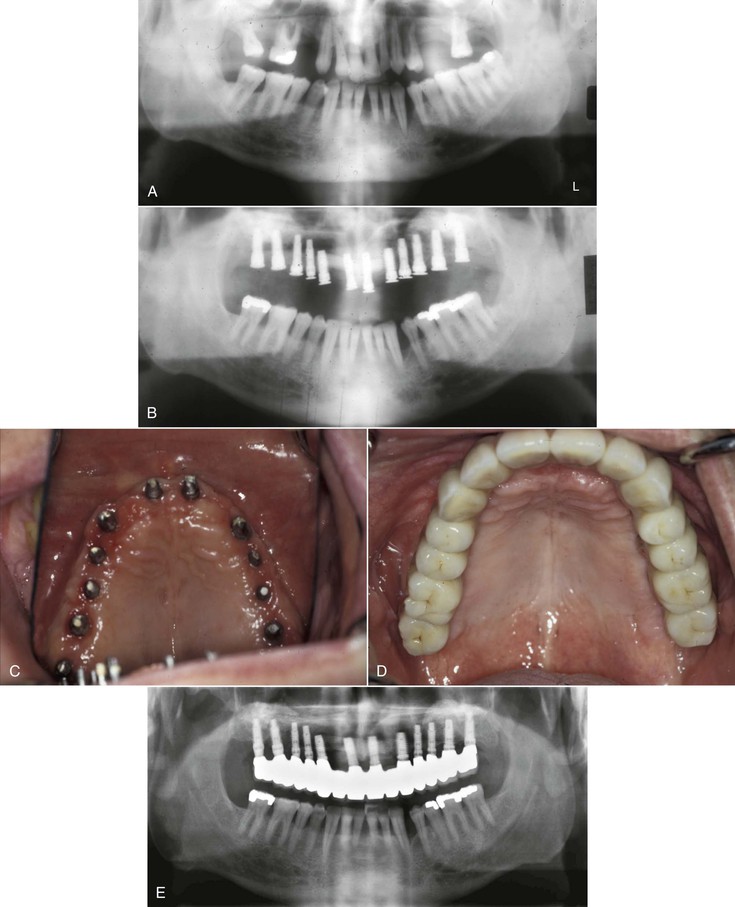
Implants serve as a foundation for the prosthetic support of missing teeth. However, in a partially edentulous patient, the existing teeth may often require restorations or other types of treatment. Hopeless teeth should be extracted and teeth with advanced periodontal or endodontic conditions treated before determining the final implant restoration and the implant position and number (Figure 16-1). Too often, a detailed treatment plan (complete with study models and computed tomography [CT] scans) is attempted before the extraction of hopeless teeth. After the extractions, more (or less) bone grafting and implant treatment is a usual consequence. As such, the time and effort to prepare the treatment plan are wasted. In addition, it causes confusion for the patient and often results in the delay of critical decisions for predictable treatment.
Extraction of Teeth with a Poor Prognosis
Maintaining natural teeth in health, function, and esthetics is a primary goal of all dentists. In the past, the maintenance of natural teeth was paramount because tooth replacement techniques were costly and not as predictable as repairing natural teeth. However, today dental implants are very predictable when available bone volume and density are present in the edentulous site. As such, under some conditions, the advanced repair procedures of a natural tooth, such as retreatment of endodontic failures or furcation treatment, may have a lower success rate than an implant to replace the tooth. Therefore, on occasion, when the natural tooth is significantly compromised, the extraction and replacement with an implant is the treatment of choice. In addition, multiple advanced procedures on the same tooth may be more expensive (and less predictable) than extraction of the tooth and replacement with an implant.
A tooth may be considered for extraction because of prosthetic, endodontic, periodontal, or surgical considerations. On rare occasions, extraction is considered rather than orthodontics to restore the teeth in a more esthetic or functional position.
Prosthetic Considerations
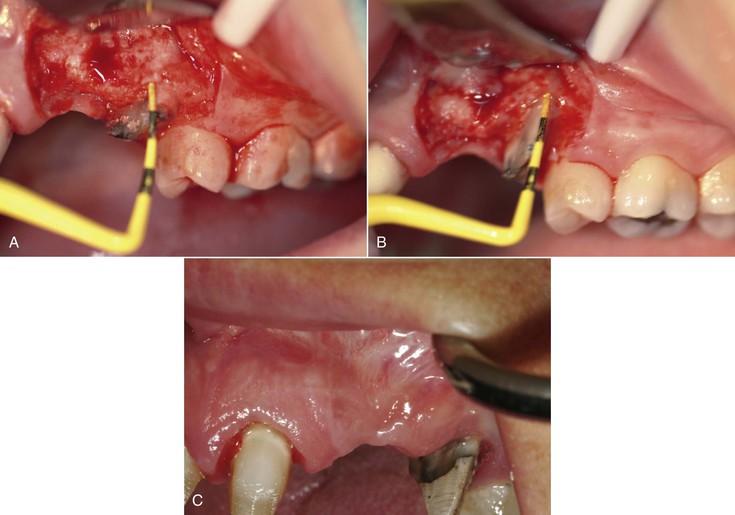
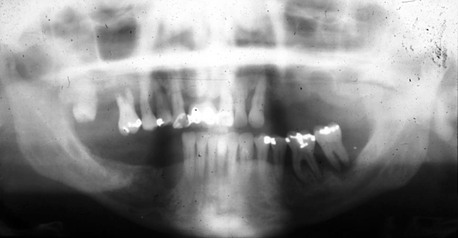
Caries on a natural tooth is most often able to be removed and the tooth restored. However, on occasion, the tooth is unrestorable after the decay is removed. A prosthetic axiom is to have at least 1.5 to 2 mm of tooth structure for a crown with a cervical ferule effect. In addition, adequate retention and resistance from the tooth preparation should exist.1–2 As a result of the caries, additional treatment as endodontic therapy, post and core, and functional crown lengthening may be required (Figure 16-2). Thus, procedures to save the tooth are costly and on occasion less predictable than an implant. In addition, the end result may not be esthetically pleasing. For example, when a central incisor requires considerable functional crown lengthening, the gingival margin may be compromised and have a poor esthetic result.
A patient with a history of high decay rate, a high caries index, and recurrent caries under crowns requiring endodontics with a post and core before restoration and may be better served with an extraction and implant insertion (Figure 16-3). The repeated recurrent decay can be eliminated, at least for that tooth, with an implant. In addition, when caries extends within the root canal, the outer structural walls of the natural root may be too thin for a predictable post or restoration. As a result, extraction and implant insertion has a better prognosis.
When the dentate arch opposing an edentulous posterior region exfoliates or extrudes beyond the occlusal plane many millimeters, the tooth may require several procedures to restore the correct occlusal plane. Endodontics and functional crown lengthening beyond the furca of the roots may be necessary. After these procedures, the lateral wall thickness of the root may be minimal for the post and core. A structural failure is most likely under these conditions. An extraction and implant may be appropriate, especially in cases of moderate to severe parafunction. Another option for extruded or exfoliated teeth may be orthodontic intrusion, often with an implant as a transitional anchorage device (TAD). This is more often the treatment of choice when orthodontic therapy is required to improve the position of the rest of the teeth in both arches.
Endodontic Considerations
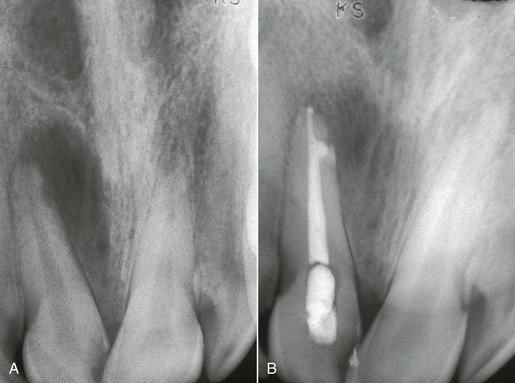
Endodontic conditions may cause the dentist to consider tooth extraction rather than traditional treatment. For example, when the root canal cannot be accessed because of abnormal root anatomy or previous restoration, an extraction and implant insertion may be considered rather than an apicoectomy (Figure 16-4). On occasion, the endodontic procedure in the posterior mandible requires an apicoectomy and has a moderate to high risk of paresthesia. An implant after extraction may be less invasive and have less risk of paresthesia.
A tooth with a “split root” syndrome may have root canal therapy, with pain still present during function, and may be treated with extraction and implant insertion. If the endodontic procedure appears satisfactory but pain persists during function, retreatment of the tooth is often not predictable. Rather than waiting for an observable symptom, the subjective finding of pain during function may be enough cause to extract the tooth. An extraction and implant insertion is usually a definitive treatment that eliminates more predictably pain during function than endodontic retreatment of the tooth.
A meta-analysis of endodontic success concludes the success rate of endodontic therapy is 90% at 8 years. However, it must be noted that the rates of success for endodontics are different than the “success” rates reported with implants.3,4 Success rates reported with dental implants are most often survival rates.5 If the implant is in the mouth, it is considered a “success” regardless of the quality of health. However, success in many endodontic studies is often related to resolution of all peirapical pathology. Hence, when tooth survival after endodontic therapy is considered, endodontic treatment is similar to implant therapy. As such, traditional endodontics is the treatment of choice for most teeth that are able to be restored.
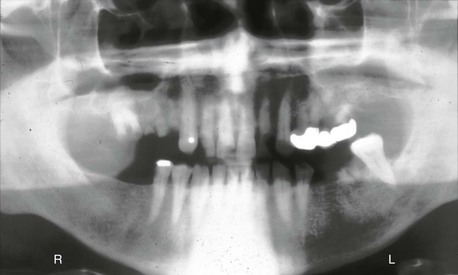
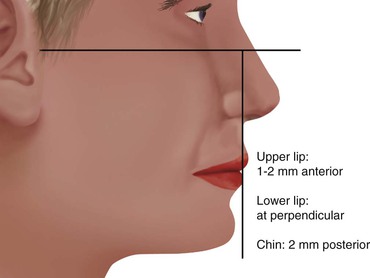
Whereas a vital tooth has endodontic success rates above 93%, a nonvital tooth has an 89% rate.6,7 A large periapical lesion (larger than 5 mm) compromises the success rate of traditional endodontics. A nonvital tooth with large periapical pathology has a success rate of 78%. As a result of a lower “success” rate, endodontic therapy should still be performed, but the tooth should be evaluated over several months before post, core, and crown treatment (Figure 16-5).
If endodontic retreatment is necessary, consideration for extraction may be more justified. A retreatment of an endodontic tooth (that appears radiographically to be within normal limits) with a periapical lesion has a reported “success” rate of 65%. As a result, the additional retreatment cost may lead to consideration for extraction and implant replacement. Therefore, for devital teeth with more than 5-mm apical radiolucencies that do not resolve after initial endodontic treatment and periapical lesions remain or reappear with clinical consequences, an extraction should be considered. This may be even more justified when an apicoectomy is the treatment of choice to treat the failure.8
Periodontal Considerations
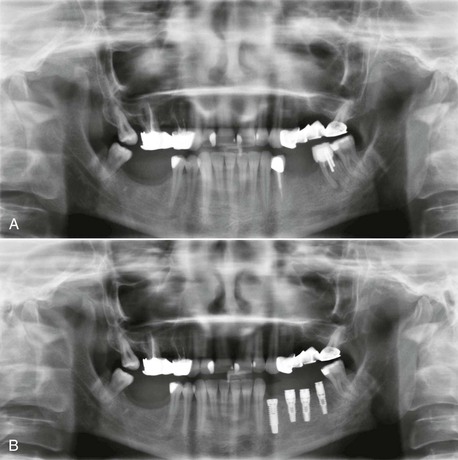
The existing teeth in a partially edentulous patient should be evaluated for periodontal disease. Advanced periodontal disease may be addressed with extraction of questionable abutments more frequently than in the past, provided the resulting edentulous area offers sufficient bone for predictable endosteal implant placement and a predictable prognosis9 (Figure 16-6).
Herodontics are discouraged when the prognosis is poor or failure of treatment may result in inadequate bone for implant placement. This is especially noted when the existing available bone around the tooth roots is compromised in height, especially in the posterior mandible. Unsuccessful periodontal treatment and continual bone loss may render the remaining bone inadequate for placement of implants after extraction of the teeth. Bone grafting to improve available bone height in the posterior mandible is more unpredictable than any other region of the jaws. As a result, when 10 mm of bone is all that remains from the mandibular canal to the remaining bone around the periodontally involved teeth, consideration is given to the predictable aspects of periodontal therapy. When in doubt, the teeth should often be extracted (Figure 16-7).
The etiology of furcation involvements includes bacteria as well as plaque in the furca with extension of inflammation in the region with loss of interradicular bone. This leads to a progressive and site-specific loss of attachment in most individuals. A first molar furcation entrance cannot be accessed with traditional periodontal hand instruments almost 60% of the time.10 In addition, pulpal pathoses with accessory canals in the furca may cause a combination of endodontic and periodontal problems. Vertical root fracture after endodontic therapy may also occur with greater incidence. Hence, patients with moderate periodontal disease that includes the molars are at greater risk of the continuation of the disease.
Furcation treatment of molars may include root amputation. The lowest success rate for root resection was found on mandibular distal root resections (75%).11,12 Even when successful, the remaining root indicates endodontics, core and crown of the remaining root, and the prosthetic replacement of the distal root with an implant or fixed partial denture (FPD) (Figure 16-8). An extraction, socket graft, and implant is more predictable to treat this condition. An implant may also replace the whole tooth with a lower cost. As a consequence, mandibular molar root resection should be replaced by extraction and implant therapy.
A distal furca in a maxillary molar is the most common furca involvement because it is directly below the interproximal contact and has difficult access for hygiene.13,14 A maxillary molar that has lost bone to the furcation has lost almost 30% of the root surface area of support. However, when a distal buccal root is resected in the maxilla, often the crown may be restored to fill the mesiodistal space, and an additional procedure is not required. Hence, a distal–palatal furca treated with a root resection is often indicated in the maxilla rather than extraction and an implant.
When a maxillary molar has more than one furca condition or short roots, a root resection, or even a considerable functional crown lengthening may compromise the remaining support or result in another furcation involvement. The endodontics, post and core, and functional crown lengthening may not be as predictable as extraction and implant insertion. In addition, the cost of this conventional treatment may be twice the cost of an implant.
On occasion, successful periodontal therapy is accompanied with a poor esthetic result. It may be more prudent to extract the unesthetic teeth even though the periodontal therapy was “successful.” Under these conditions, implant prosthesis may restore the dentition with a more esthetic restoration (Figure 16-9).
Traditional methods to save a tooth have increased in cost over the years. The cost of questionable periodontal treatment may result in the patient’s inability to afford the subsequent more predictable implant therapy. Multirooted endodontic therapy now approaches the cost of an implant surgery. When functional crown lengthening and endodontic posttreatment are also required, the fees are usually greater than those for extraction and implant insertion. Therefore, part of the equation of whether to extract or treat a tooth may also relate to the cost of the service provided. The natural molar tooth that requires endodontics, root amputation, post and core placement, and nevertheless a compromised root with a poor root surface area may be cost prohibitive for the service provided. In these cases, an implant in the site after tooth extraction is often less expensive and more predictable in the long term.
It should be noted that the recent trend to extract teeth with a good prognosis (with or without the need for endodontic or periodontal treatment) is discouraged.15 Implants are not yet 100% predictable, and implants should not be substituted for natural teeth presenting a good or even a fair prognosis.
0-, 5-, or 10-Year Rule
The dentist evaluates the natural teeth for their quality of health with widely used prosthetic, periodontal, and endodontic indexes. After this is accomplished, the dentist may obtain an estimate of longevity and decide whether to extract or to treat and maintain the tooth following a 0-, 5-, or 10-year rule.16 Box 16-1 summarizes the decision-making protocol involving a natural tooth. If the natural tooth has a favorable prognosis for more than 10 years, it is included in the treatment plan. The decision to use it or not as an abutment if it is adjacent to an edentulous space requires additional information, but few reasons support removal of the tooth to restore the partially edentulous patient.
If the natural tooth prognosis (after periodontal, endodontic, or restorative therapy when necessary) is in the 5- to 10-year range, the tooth should be maintained. If the tooth is adjacent to a missing tooth site, an independent implant-supported prosthesis is indicated. If the edentulous region does not provide sufficient implant support for an independent restoration, then placement of as many implants as possible around the tooth, with treatment alternatives that will permit removal of the tooth without sacrificing the restoration is indicated. For example, a coping may be placed on the tooth with a 5- to 10-year prognosis, and the tooth may act as “living pontic” in the final restoration, splinted to the adjacent implants on each side. Whether the tooth is missing or present does not modify the prosthesis. In this way, the prosthesis may be removed in the future, and the tooth may be extracted (if indicated). In this way, the prosthesis essentially is maintained without compromise.17
When teeth with copings are joined to implants, the copings on the teeth should be designed with a different path of insertion than the FPDs, and the coping should be cemented with permanent cement. The fixed implant prosthesis usually is cemented with a weaker (soft access) or temporary cement. Thus, the FPD path of removal differs from that of the natural tooth coping and, along with the weaker cement, allows the prosthesis to be removed while the coping remains permanently cemented on the tooth. The preparation of copings on natural teeth often requires additional removal of tooth structure to prevent overcontoured restorations and as a consequence may mandate endodontic therapy.19
When the estimate of survival of the natural tooth is in the 0- to 5-year survival (even after treatment), strong consideration is given to extraction of the tooth and implant replacement. As a consequence, the definitive treatment plan is delayed until after the extraction(s). For example, CT scans, mounted study casts, treatment prostheses, bone grafts (other than socket grafts), and so on are delayed until after the extraction sites initially heal because some intraoral conditions may be modified during this process. This treatment scenario may also often be faster and less costly over a 5- to 10-year period compared with maintaining a questionable tooth, especially when it is adjacent to an edentulous site.
Clinical Examples
If hygiene is poor in patients with a grade II or III furca involvement in molars, the tooth most often is considered in the 0- to 5-year category and is considered for extraction. This is especially considered when other teeth in the same quadrant are missing or hopeless or only 8 to 10 mm of bone remains between the crest of bone and the opposing landmark.12,13,18
Molars with grade I furcation involvement often are placed in the 5- to 10-year prognosis category. However, it should be noted that maxillary molars are at higher risk of furca complications, and even grade I furcations are lost 33% of the time within 5 years without treatment.14 Mandibular molars have a 20% failure at this same reference time. Therefore, even when grade 1 furcas are diagnosed, aggressive treatment and good oral hygiene are necessary, especially if the tooth needs extensive restoration.
Patients with a potential structural failure after restoration (as a result of caries or trauma) and who require endodontics, functional crown lengthening, posts and cores are considered in the 0- to 5-year category. When the caries index is high, especially with poor hygiene, and multiple restorations have failed, extraction of those teeth may be indicated.
When the patient has an endodontic lesion of greater than 5 mm on a previously treated endodontic tooth (which appears within an acceptable technique), the tooth is considered for extraction. A tooth that has pain during function, despite radiographically successful endodontic therapy, may have a split root and is considered to be in the 0- to 5-year category.
The dentist should evaluate teeth especially next to an edentulous site. A natural tooth distant from the future implant restoration site is less likely to affect the implant reconstruction and alter the treatment sequences in this site. However, failure of a natural tooth adjacent to an implant site may cause failure of the adjacent implant and almost always (whether failure occurs or not) causes the restoration to be delayed and compromised. Therefore, if the practitioner is not sure whether the tooth is in the 0- to 5-year or 5- to 10-year category, the tooth adjacent to the future implant site more often should be considered to have the poorer prognosis.
Overall Evaluation
The evaluation of the remaining teeth should precede the definitive treatment plan to replace missing teeth. The existing conditions of the stomatognathic system outside the range of normal should be evaluated and treated when necessary. This treatment may be performed before or in conjunction with implant therapy. As such, preimplant prosthodontic considerations are a vital phase of the overall treatment.
The existing teeth and arch relationships do not need to be perfect before implant surgery. However, because implant dentistry always concerns the replacement of teeth, at least a diagnosis and treatment plan should occur before implant placement. The goal is to identify and restore the prosthetic parameters of the remaining teeth within normal limits. The correct tooth positions should be first determined, so even if the total treatment time is extended over several years, at least each segment will aim toward a consistent goal. Too often the restoring dentist assumes the patient wants the cheapest or fastest treatment related to each treatment or to remain within the dental insurance limits of reimbursement. As a consequence, the mouth is restored one or two teeth at a time, fitting the restoration into the patient’s present occlusal condition, which usually worsens over time and never improves on its own. As a result, after the patient has been in the same practice for several decades, the overall dentition is in poorer condition than when the patient started. Although it is easier to restore an entire mouth to the correct occlusal relationships at one time, it is also possible to obtain a similar result one tooth at a time as long as each step proceeds along the predetermined course of the overall treatment.
The preimplant prosthodontic evaluation of the patient’s overall condition closely resembles traditional dentistry. When a restoring dentist first evaluates the prosthetic needs of a patient, an orderly process is required regardless of the current state of the dentition. In other words, regardless of whether the patient has all of his or her teeth or is missing all of the teeth, after the dentist accepts the responsibility of long-term professional guidance and treatment as necessary, a consistent approach to care is beneficial.
There are five initial elements of the existing teeth that should be assessed in sequence and treated when indicated. These elements are the maxillary anterior tooth position, existing occlusal vertical dimension (OVD), mandibular incisor edge position, maxillary occlusal plane, and mandibular occlusal plane16 (Box 16-2). These elements are evaluated in a partially edentulous patient during the initial clinical examination and may also be assessed on mounted diagnostic casts (which may also serve for diagnostic wax-up procedures).
Maxillary Anterior Tooth Position
The position of the existing maxillary anterior teeth is first assessed. Most often these natural teeth are adequate in location and incisal edge position. However, if their position is undesirable for any reason, orthodontics or restoration may be indicated. At this point, the evaluation is not for the cosmetic aspects of tooth color or shape, but tooth position is scrutinized. If the maxillary incisor edge is modified in either the horizontal or vertical plane, all other four elements of the stomatognathic system may also need to be changed.
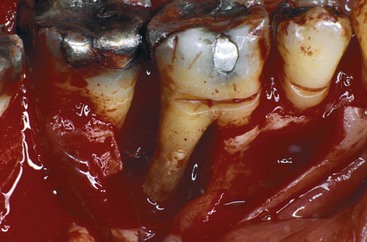
The labial position of the maxillary anterior teeth is first determined with the lip in repose. This is primarily evaluated by overall support of the maxillary lip and its relationship to the balance of the face, especially in relation to the nose and presence or absence of a philtrum in the midline.19–21 A perpendicular line from the Frankfort plane (plane passing through the lowest point in the floor of the left orbit and the highest point of each external auditory meatus of the skull) that touches the lower lip should most often find the maxillary lip 1 to 2 mm in front of this line and the chin 1 to 2 mm behind this line (at the correct OVD) (Figure 16-10).
When the teeth are positioned more labially, the vertical position of the lip is elevated. Likewise, a more palatal position of the maxillary anterior teeth results in a more inferior or extended position of the lip. If the labial or horizontal position of the lip is going to be altered, orthodontic therapy is the treatment of choice in a dentate premaxilla. On occasion, a prosthetic or surgical approach may be indicated with or without orthodontic treatment.
An alternative to increasing the length of the anterior teeth so more teeth are visible with the lip in repose may be to increase the thickness of the premaxillary alveolar ridge. This extra alveolar ridge thickness brings out the lip and raises the vermilion border. As a result, the teeth are not longer, but the border of the lip is higher. In addition, if the added width to the ridge is with autologous bone, replacing teeth with implants rather than pontics further helps to maintain the situation. The fuller maxillary lip may also look younger because vertical age lines may also be reduced.
In a completely edentulous patient, the labial flange of the patient’s existing denture may be removed and the lip position evaluated before the completed treatment plan for a fixed restoration. When the lip needs the support of the labial flange for esthetics yet a fixed restoration is planned, onlay grafts with hydroxyapatite (HA), connective tissue, autograft, or allograft may be indicated to increase labial tissue thickness for proper lip support.
The next step in the evaluation process (when the labial position is acceptable) is the vertical position of the maxillary anterior teeth related to the lip in repose.22 The maxillary canine is the key for this position.23 Misch has suggested the canine tip be located ± 1 mm with the lip in repose regardless of the age or sex of the patient (Figure 16-11). A horizontal line drawn from one canine tip to the other should be level to the horizon. The central incisors are 1 to 2 mm longer than the horizontal plane to the canines.
The position of the maxillary central incisor, in relation to the maxillary lip and the age of the patient (a range of 8 mm) is much more variable than the position of the canine (a range of 3 mm).23 The lip bow in the center of the upper lip rises several millimeters on some women and is barely obvious on others. The higher the lip bow, the more central incisor surface is seen on the patient regardless of age. Men rarely exhibit an exaggerated lip bow and therefore have a more consistent incisor edge to lip position. The canine position is closer to the corner of the lip and is not affected by the lip bow effect in the midline. As such, it is a more consistent position and usually corresponds to the length of the resting lip position from 30 to 60 years of age in both men and women.
No other region of the mouth should be restored until this position is corrected because it negatively influences the proper position of every other segment (e.g., OVD, mandibular anterior tooth position, and posterior planes of occlusion). If the patient is wearing a maxillary complete denture, the maxillary anterior tooth position is often incorrect. As a result of resorption of the premaxilla, the denture shifts apically and posteriorly following the bone loss pattern.
Arch relationships are often affected by resorption patterns in edentulous ridges. The anterior and posterior edentulous maxilla resorbs toward the palate after tooth loss.24 The width of the alveolar ridge decreases 40% within a few years, primarily at the expense of the labial plate. Consequently, implants are often placed lingual to the original incisal tooth position. The final restoration is then overcontoured facially to restore the incisal two thirds in the ideal tooth position for esthetics. This results in a cantilevered force on the implant body. The maxilla is affected more often than the mandible because the incisal edge position in the esthetic zones cannot be modified and is dictated by esthetics, speech, lip position, and occlusion. Anterior cantilevered crowns from maxillary anterior implants often require additional implants splinted together and an increase in the anteroposterior (A-P) distance between the most distal to most anterior implant positions to compensate for the increased lateral loads and moment forces to the premaxillary implants, especially during mandibular excursions.
The maxillary anterior horizontal and vertical tooth positions are evaluated before any other segment of the arches, including the OVD. If the maxillary anterior teeth are significantly malpositioned, the clinician should obtain further diagnostic studies, such as a cephalometric radiograph, to determine the relationship of the maxilla to the cranial base. The patient may have unfavorable skeletal relationships (vertical maxillary excess or deficiency). If the position of the natural maxillary anterior teeth is undesirable for any reason, orthodontics, orthognathic surgery, or restoration may be indicated. After the position of the maxillary anterior teeth is acceptable, the next prosthetic step is either the evaluation of the OVD or maxillary occlusal plane.
Existing Occlusal Vertical Dimension
To determine the anterior position of the mandible and the crown height space (CHS) of the maxilla, mandible, or both, the overall issue of OVD must be addressed. The patient’s existing OVD should be evaluated early in an implant prosthetic treatment plan because any modification will significantly modify the overall treatment. Not only will a change in OVD require at least one full arch to be reconstructed, but it will also affect the CHS and therefore the potential number, size, position, and angulation requirements of the implants.
The OVD is defined as the distance between two points (one in the maxilla and the other directly below in the mandible) when the occluding members are in contact.25 This dimension requires clinical evaluation of the patient and cannot be evaluated solely on the diagnostic casts.
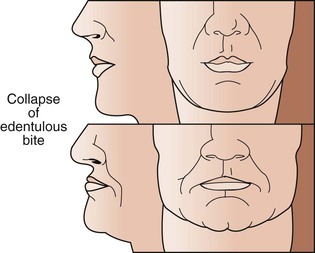
The determination of the OVD is not a precise process because a range of dimensions is possible without clinical symptoms.26,27 At one time, it was believed OVD was very specific and remained stable throughout a patient’s life. However, this position is not necessarily stable when the teeth are present or after the teeth are lost. Long-term studies have shown that this is not a constant dimension and often decreases over time without clinical consequence in dentate, partially edentulous, and completely edentulous patients. A completely edentulous patient often wears the same denture for more than 10 years, during which time the OVD is reduced 10 mm or more without symptoms or even patient awareness.
The OVD may be altered without the symptoms of pain or dysfunction, especially when the condylar disc assembly is healthy. However, this is not to say that altering the OVD has no consequence. Rather, a change in OVD affects the esthetics of the chin to face position and the CHS. As such, it may affect the biomechanics of the support system of a prosthesis. Any change in the OVD will modify the horizontal dimensional relationship of the maxilla to the mandible. Therefore, a change in OVD will modify the anterior guidance, range of function, and facial esthetics.28
The most important effect of OVD on tooth (implant) loading may be the effect on the biomechanics of anterior guidance. The more closed the OVD, the farther forward the mandible rotates and the more skeletal class III the chin appears (Figure 16-12). A bruxing patient who had a skeletal class I tooth position may develop an end-to-end incisal position along with a closed OVD (Figure 16-13). Because this type of patient has lost incisal guidance, the continued bruxism will more rapidly wear the anterior and posterior teeth. Hence, restoring OVD and incisal guidance is paramount to any oral reconstruction.
In a skeletal class II, division 2 patient, the more closed the OVD, the steeper the anterior guidance and the greater the vertical overbite of the anterior teeth. When the OVD is opened, there may be no anterior contact in occlusion. Hence, orthodontics or repositioning the lower anterior teeth may be necessary to restore incisal guidance. Anterior guidance is necessary to maintain incisal guidance during mandibular excursions to decrease the risk of posterior interferences.
The conditions of an increased vertical overbite will increase the forces to the anterior teeth (or implants). Hence, the OVD should be increased in a skeletal class II division II patient. Increasing the OVD has the opposite effect on the incisal guidance. In general, for a dentate patient, it may be more precarious to close an OVD than to open it because the resulting anterior rotation of the mandible will position mandibular incisor teeth facially in a closer relationship to the maxillary teeth in centric occlusion.
In completely edentulous patients restored with fixed implant prosthodontics, a change in OVD in either direction affects biomechanics. Opening the OVD and decreasing the incisal guidance with a resulting bilaterally balanced occlusion may increase forces placed on posterior implants during mandibular excursion. Closing the OVD may increase the forces to anterior implants during any excursion. On occasion, a change in the OVD may also affect the sibilant sounds by altering the horizontal position of the mandible.
The OVD is almost never naturally too large and, unless some manufactured interference has been created, it is within clinical guidelines or collapsed. Therefore, the restoring dentist most often should determine whether the OVD needs to be increased. In other words, the existing OVD in a patient without symptoms of the temporomandibular joint (TMJ) is a position to start the evaluation, not one that necessarily must be maintained.
According to Kois and Phillips, three situations primarily mandate the modification of the OVD: (1) esthetics, (2) function, and (3) structural needs of the dentition.28 Esthetics is related to OVD for incisal edge positions, facial balance, and position of the chin and the occlusal plane. Function is related to the canine positions, incisal guidance, and angle of load to teeth or implants. Structural requirements are related to dimensions of teeth for restoration while maintaining a biological width, or the CHS, which may modify biomechanical force.
Methods to Evaluate Occlusal Vertical Dimension
In traditional prosthodontics, a range of techniques has been described to establish the OVD. Whereas objective methods use facial dimension measurements, subjective methods rely on esthetics, resting arch position, and closest speaking space. There is no consensus on the ideal method to obtain the OVD. Therefore, this dimension is part art form and part science. And yet it is critical enough that a final treatment plan should not be rendered until a determination has been made relative to this dimension.
The subjective methods to determine OVD include the use of resting interocclusal distance and speech-based techniques using sibilant sounds.29,30 Niswonger proposed the use of the interocclusal distance (“freeway space”), which assumes that the patient relaxes the mandible into the same constant physiologic rest position.27 The practitioner then subtracts 3 mm from the measurement to determine the OVD. Two observations conflict with this approach. First, the amount of freeway space is highly variable in the same patient, depending on factors such as head posture, emotional state, presence or absence of teeth, parafunction, and time of recording (greater in the morning). Second, interocclusal distance at rest varies 3 to 10 mm from one patient to another. As a result, the distance to subtract from the freeway space is unknown for a specific patient. Therefore, the physiologic rest position should not be the primary method to evaluate OVD. However, it should be evaluated after the OVD is established to ensure a freeway space exists when the mandible is at rest.
Silverman stated that approximately 1 mm should exist between the teeth when making an S sound.31 Pound further developed this concept for the establishment of centric and vertical jaw relationship records for complete dentures.32,33 Although this concept is acceptable, it does not correlate to the original OVD of the patient. Denture patients often wear the same prosthesis for more than 14 years and during this time lose 10 mm or more of their original OVD. Yet all of these patients are able to say “Mississippi” with their existing prosthesis. If speech were related to the original OVD, these patients would not be able to pronounce the S sound because their teeth would be more than 11 mm apart. But to say the letter “S” with the correct sound, the teeth must be approximately 1 mm apart. Therefore, the speaking space should not be used as the only method to establish OVD. After the OVD has been determined, the speaking space should be observed, and the teeth should not touch during sibilant sounds. On occasion, a short adjustment period of a few weeks may be required to establish this criterion. Therefore, on occasion, a transitional prosthesis should be used to evaluate this position in case it must be modified before the final restoration.
Kois and Phillips have noted that the subjective method of esthetics to establish an OVD is the most difficult to teach inexperienced dental students and therefore is least likely to be initially addressed when teaching the concepts of determining OVD.28 However, experienced clinicians often value this method more than any other to assess OVD.
After the position of the maxillary incisor edge is determined, the OVD influences esthetics of the face in general. Facial dimensions are objective (because they are measured) and directly related to the ideal facial esthetics of an individual. They can be easily assessed regardless of the clinician’s experience.34–42 This objective evaluation is usually the method of choice to initially evaluate the existing OVD or establish a different OVD during prosthetic reconstruction. In addition, it may be performed without the need of additional diagnostic tests.
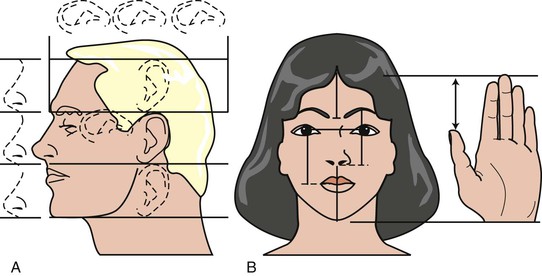
Facial measurements can be traced back to antiquity, when sculptors and mathematicians followed the golden ratio for body and facial proportions as described by Plato and Pythagoras. The golden ratio relates to the length and widths of objects in nature as 1 to 0.618. It was observed that biologic features follow this ratio. Architectural proportions often follow the golden ratio because it is considered the most esthetically appealing to the human eye.35–37 Leonardo da Vinci later contributed several observations and drawings on facial proportions, which he called divine proportions.39 He observed the distance between the chin and the bottom of the nose (i.e., OVD) was a similar dimension as (1) the hairline to the eyebrows, (2) the height of the ear, and (3) the eyebrows to the bottom of the nose—and each of these dimensions equaled one third of the face.
Many professionals, including plastic surgeons, oral surgeons, artists, orthodontists, and morticians, use facial measurements to determine OVD. Misch reviewed the literature and found that many different sources reveal many correlations of features that correspond to the OVD40,41:
1. The horizontal distance between the pupils
2. The horizontal distance from the outer canthus of one eye to the inner canthus of the other eye
3. Twice the horizontal length of one eye
5. The horizontal distance from the outer canthus of the eye to the ear
7. The vertical distance from the external corner of the eye (outer canthus) to the corner of the mouth
8. The vertical height of the eyebrow to the ala of the nose
10. The vertical distance from the hairline to the eyebrow line
11. The vertical height of the ear
12. The distance between the tip of the thumb and the tip of the index finger when the hand lays flat with the fingers next to each other (Figure 16-14).
All of these measurements do not correspond exactly to each other, but they usually do not vary by more than a few millimeters (with the exception of the vertical height of the ear) when facial features appear in balance. An average of several of these measurements may be used to assess the existing OVD. In a clinical study by Misch, the OVD was often slightly larger than the facial measurements listed (more in men than women) but was rarely a smaller dimension.41 The subjective criteria of pleasing esthetics may then be considered after the facial dimensions are within balance to each other.
Esthetics are influenced by OVD because of the relationship to the maxillomandibular positions. The smaller the OVD, the more skeletal class III the jaw relationship becomes; the greater the OVD, the more skeletal class II the relationship becomes. The maxillary anterior tooth position is determined first and is most important for the esthetic criteria of the reconstruction. Alteration of the OVD for esthetics rarely includes the maxillary tooth position. For example, the OVD position may be influenced by the need to soften the chin for a patient with a large mental protuberance by increasing the OVD.
Radiographic methods to determine an objective OVD are also documented in the literature. Tracings on a cephalometric radiograph are suggested when gross jaw excess or deficiency is noted. Such conditions may stem from vertical maxillary excess; vertical maxillary deficiency; vertical mandibular excess (long chin); vertical mandibular deficiency (short chin); or apertognathia or skeletal class II, division 2 (deep bite) situations. Orthodontic treatment planning of a dentate patient often includes a lateral cephalogram and may be used to evaluate OVD (glabella–subnasale, subnasale–menton). The same measurements may be performed on an edentulous patient.43,44
After the OVD satisfies the esthetic requirement of the prosthetic reconstruction, it may still be slightly refined. For example, the OVD may be modified to improve the direction of force on the anterior implants. In addition, on occasion, anterior mandibular implants are too facial to the incisal edge position, and increasing the OVD makes them much easier to restore. Therefore, because the OVD is not an exact measurement, the ability to alter this dimension within limits may often be beneficial.
Combination Syndrome
The evaluation of the pretreatment OVD is also very important for a patient wearing a complete maxillary denture opposing a partially edentulous mandible, especially in the case of edentulous posterior segments that are not compensated by a removable partial denture (Kennedy-Applegate class I). Under these conditions, a combination (Kelly) syndrome may be present and is especially noteworthy if the OVD is within normal limits.45 The clinical symptoms include (1) maxillary incisors of the denture positioned up and rotated back from ideal, (2) lower natural anterior teeth overerupted and beyond the mandibular occlusal plane, (3) maxillary horizontal occlusal plane tilted apically in the anterior and occlusally in the posterior regions, (4) enlarged tuberosities encroaching on the mandibular interarch space, (5) maxillary palatal hyperplasia, and (6) highly mobile tissue in the premaxilla. In addition, because the mandibular posterior teeth have been missing for many years to develop these clinical conditions of this syndrome, there is a lack of posterior bone in the mandible to place endosteal implants (Figure 16-15).
The proper maxillary incisal edge position and OVD are especially critical for these patients because of the incidence of mandibular incisor extrusion beyond the maxillary occlusal plane. The extrusion is usually accompanied by the alveolar process. To position the maxillary incisors properly, the mandibular anterior teeth must be repositioned at the proper incisal plane. Orthodontic intrusion (often with implants that are TADs) or enamel p/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses