16
Patient evaluation: dental implants in periodontally compromised patients
Treated Periodontitis Subjects
Implant Outcomes
Patients with a history of periodontitis demonstrate a greater risk for peri-implantitis (OR 3.1–4.7) and a lower implant survival rate (ISR) than non-periodontal patients (Ong et al., 2008; Cochran et al., 2009). Nevertheless, over a period of 3–16 years, the ISR remains high, i.e. greater than 90%, when the patients are periodontally well maintained (Heitz-Mayfield & Huynh-Ba, 2009).
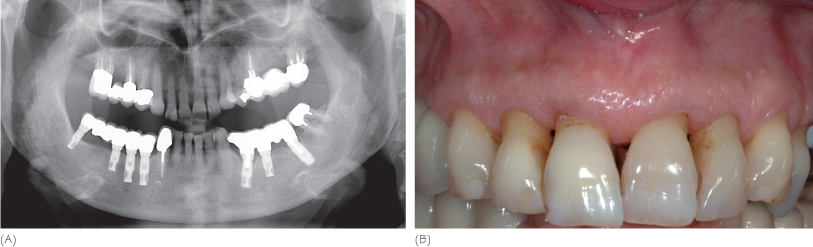
Thus, a history of treated periodontitis does not contraindicate implant therapy (Fig. 16.1). However, the patient must be informed of an increasing risk of implant failure and peri-implantitis (see Appendix E). The completed prosthesis and its supporting components (teeth and implants) must be carefully monitored with a maintenance program that includes systematic and continuous monitoring of the periodontal and peri-implant tissue conditions.
Figure 16.1 Dental implant therapy in a well maintained periodontitis patient. (A) Panoramic radiography, 7 years after implant placement. (B) Clinical view at the time of the radiography.
Risk Factors
Smoking is a risk factor for periodontitis and peri-implantitis. Patients who combine cigarette smoking and a history of periodontitis should be considered at risk for implant failure, even if further research is required to properly assess the combination of these factors. Implant placement procedures do not affect the ISR (one-stage versus two-stage). The ISR does not change when immediate implant insertion and immediate loading procedures are applied. The characteristics of the implant surface seem to influence the ISR. Lower ISRs are observed for very rough surfaces.
Dental Implant Therapy
In cases of severe periodontitis, subsequent alveolar bone resorption poses a significant challenge to achieving esthetic and functional restorations. Implant placement in periodontitis patients often results in long, unesthetic teeth (Fig.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


