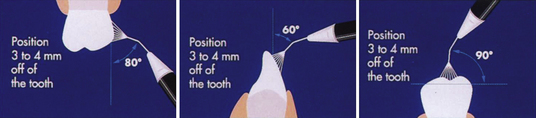
Figure 27-18 Recommended angulations of Prophy-Jet nozzle to tooth surface.
(Adapted from DENTSPLY Preventive Care Division, York, Pennsylvania.)
Chapter 27 Management of Extrinsic and Intrinsic Stains
Procedure 27-1 RUBBER-CUP POLISHING
Photographs courtesy Dr. Margaret Walsh, University of California-San Francisco.
| EQUIPMENT | |
| Polishing paste, esthetic restoration polishing paste, and low-abrasive toothpaste | |
| Prophylaxis angle and toothbrush | |
| Dental floss or tape | |
| Floss threader (if needed) | |
| Rubber cups and pointed bristle brushes | |
| Low-speed handpiece | |
| Gauze squares | |
| Mouth mirror, air-water syringe | |
| Disclosing solution | |
| Preprocedural antimicrobial mouth rinse | |
| Saliva ejector or high-volume evacuation (HVE) tip | |
| Safety glasses for client | |
| Personal protective equipment (PPE) | |
| STEPS | RATIONALES |
| PREPARATION AND POSITIONING | |
| 1. Evaluate client’s health and pharmacologic history to determine need for antibiotic premedication. | Ensures protection from health risks. |
| 2. Identify tooth surfaces indicated and contraindicated for polishing. Always polish esthetic restorations first, then polish teeth. | Prevents unnecessary removal of tooth structure; maintains esthetic dental material by using specially designed nonabrasive polishing parts; ensures protection from health risks. |
| 3. Educate client about selective polishing procedure. | Facilitates client acceptance. |
| 4. Select polishing abrasive based on type of stain and oral restorations and assemble basic setup (Figure 27-1). | Prevents unnecessary removal of tooth structure. |
| 5. Wear appropriate PPE and provide protective eyewear for client. | Prevents cross-contamination; protects client’s eyes from spatter. |
| 6. Provide client with a preprocedural antimicrobial rinse polishing. | Reduces aerosol microorganisms; minimizes occurrence of bacteremia in at-risk clients. |
| 7. Have client tilt head up and turn slightly away when polishing maxillary and mandibular right buccal surfaces of posterior teeth (left buccal if left-handed practitioner) and maxillary and mandibular left lingual surfaces of posterior teeth (right lingual if left-handed practitioner). | Enhances access and visibility; prevents occupational injury. |
| GRASP | |
| 8. Use modified pen grasp (Figure 27-2). | Facilitates movement of handpiece. |
| 9. Rest handpiece in V of hand. | Transfers handpiece weight from fingers to hand to decrease fatigue. |
| 10. Have all fingers in contact as a unit. | Facilitates wrist-forearm motion. |
| FULCRUM | |
| 11. Establish intraoral fulcrum close to working area. | Enhances control of handpiece. |
| 12. Fulcrum on ring finger. | Facilitates pivoting for wrist-forearm motion. |
| 13. Use moderate fulcrum pressure. | Enhances stabilization. |
| ADAPTATION | |
| 14. Angle rubber cup to flare at gingival margin. | Enhances stain removal at cervical third of tooth. |
| 15. Adapt rubber cup to reach distal, facial and lingual, or mesial surfaces. | Ensures access to all surfaces with extrinsic stain. |
| 16. Adapt cup to tooth by rotating handpiece or pivoting on fulcrum as necessary. | Decreases tissue trauma; provides adequate tooth coverage. |
| 17. Adapt brush to occlusal surface. | Removes extrinsic stain from pits and grooves. |
| STROKE | |
| 18. Fill cup with paste and evenly apply to surfaces to be polished. | Ensures adequate and even distribution of paste. |
| 19. Place cup on tooth; activate handpiece by gently stepping on rheostat. Stroke from the gingival third to the incisal third with just enough pressure to make the cup flare while using wrist-forearm motion to polish the teeth. | Controls speed of handpiece; reduces finger fatigue. |
| 20. Use low speed and intermittent, dabbing, overlapping strokes with light to moderate pressure in a cervical to occlusal or incisal direction (Figure 27-3). | Dissipates heat, reduces abrasion, ensures complete coverage where needed. |
| 21. Remove rubber cup from tooth at completion of stroke; readapt cup for next stroke. | Dissipates heat. |
| 22. Hold mirror in nondominant hand to retract buccal mucosa. Instruct client to close mouth halfway and to tilt head slightly toward the ceiling. Polish buccal surfaces of maxillary right posterior quadrant (Figure 27-4). | Mirror use facilitates access and direct observation of buccal and mesial surfaces and indirect observation of distal surfaces. |
| 23. Polish facial surfaces of maxillary anterior teeth. Palm mirror and retract lip with fingers of nondominant hand (Figure 27-5). | Allows for direct vision; keeps mirror accessible. |
| 24. Hold mirror in nondominant hand to retract buccal mucosa. Instruct client to close mouth halfway and to tilt head slightly toward the ceiling. Polish buccal surfaces of maxillary left posterior quadrant (Figure 27-6). | Mirror use facilitates access, direct view of b/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


