Chapter 13
Fixed appliances – what they do and what is used
This chapter will concentrate on what is meant by fixed appliance therapy and what the nurse needs to prepare when either fitting or adjusting a fixed appliance in the surgery.
Fixed appliance therapy:
- moves teeth with great accuracy and control
- normally moves a number of teeth at the same time
- is more sophisticated than a removable appliance
- can move crowns and the roots of teeth bodily, not just tip them
- can be used with extraction or non-extraction treatments
- is sometimes used following removable or functional appliance treatment
- extra-oral traction (EOT) can be worn with it (e.g. night time to prevent first molars drifting forward)
- is used in conjunction with multi-disciplinary treatments such as orthognathic surgery and hypodontia cases
- cannot be taken in and out by the patient
PATIENT EXPECTATION – THE POPULAR CULTURE OF TRAIN TRACKS
When patients speak of orthodontic treatment, the majority of them think of fixed appliances (Figure 13.1), a system that they often refer to as ‘train tracks’. A look at clinic lists would reveal a high proportion of ‘fixed’ adjustment appointments on them.
For most patients of normal orthodontic age, this is the appliance that they would all prefer if they had the choice.
It is regarded:
- as the gold standard, ‘the proper brace’
- that braces that are removable are often seen by the patients as inferior
- as fashionable, most of their friends have it, and it gives them status
Figure 13.1 Upper and lower fixed appliances with metal brackets.

PEER PRESSURE
Much discussion of their treatment goes on at school break times and experiences are exchanged.
Most teenage patients like to be seen:
- as having the same appliances as their friends
- to be part of the crowd
However, for the patients who try to be seen as different, train tracks are also requested as they have ‘alternative’ role models, such as:
- Ugly Betty, the girl who does not fit in with the popular stereotype of a teenager
or
- Sid, the evil kid next door, the opposite of the stereotypical good guy, Andy, in Toy Story.
Patients have their own language when talking about fixed appliance treatment.
Apart from the system being known as ‘train tracks’, they call:
- the appliance – ‘braces’
- the bands – ‘rings’
- the brackets – ‘blocks’
By definition, it is a system that is fixed to the teeth and one which the patient is not able to remove.
STAGES OF TREATMENT IN FIXED APPLIANCE THERAPY
There are four stages in fixed appliance therapy:
- Alignment – aligning irregular teeth including rotations, height differentials, etc.
- Working – resolving abnormal overbites and overjets and space closure after extractions
- Finishing – torquing incisors and fine aesthetic detailing
- Retention – maintenance of the treatment results with retainers
Fixed appliances can be fitted to the teeth either by:
- direct bonding
- indirect bonding
WHAT IS USED IN FIXED APPLIANCE THERAPY
The basic mechanics of ‘train tracks’ are:
- each tooth has an attachment fitted to it
- initially, a fine arch wire is fitted into these attachments
- the teeth can be moved along the wire into alignment or be moved by the flexibility of the arch wire itself
In order to do this, the system uses:
- bands (on molar teeth)
- brackets
- and/or buccal tubes (on molar teeth)
Brackets and buccal tubes are bonded to the teeth with composite adhesive and glass ionomer cements.
Molar bands are first fitted to the teeth and then cemented.
These provide ‘handles’ on the teeth which engage the arch wire.
The capability of fixed appliances is such that a finished result should include:
- A balanced occlusion (all teeth biting evenly together)
- no residual spacing
- no rotated or submerged teeth
- an acceptable gum line (the margins look even)
While removable appliances can expand arches and tip teeth, the fixed appliance is more sophisticated.
It has a great many applications and can achieve many kinds of tooth movement:
- positional
- rotational
- ability to extrude and intrude teeth
- ability to torque the roots
THE ATTACHMENTS
- bands
- brackets
- buccal tubes, buttons, eyelets and cleats
Bands
Bands are fitted exactly around a tooth, usually on the molars and being in the masticatory regions of the dentition provide extra strength. (In some cases, however, buccal tubes may be sufficient.)
They are (Figure 13.2):
- usually made of stainless steel
- pre-formed and come in a large range of sizes
- used on both first and second molars
- stored in separate trays, for each molar and for each quadrant, so eight trays (Figure 13.3)
- have buccal tubes welded to accommodate both arch wire and headgear (Figure 13.4)
- have size and quadrant etched onto the surface of each band for identification
- have a straight occlusal edge, the gingival edge is contoured
- are for single use only
(However, if a patient’s band comes loose, it can be re-cemented for them but not used for another patient.)
Figure 13.2 Molar band.

Figure 13.3 Tray of first molar bands.

Figure 13.4 Molar band with tube.

If the molar bands are to be used as part of a trans palatal or lingual arch system, the bands will be soldered to the arch. The other teeth in the arch anterior to the first molars are fitted with brackets. This allows the arch wire which fits into the bracket slots to continue further back into a buccal tube which is attached to the side of the band. There are a great many variations on the size and type of buccal tube that can be used.
Bands can:
- have a variety of auxiliaries:
- single tubes
- double tubes
- triple tubes (Figure 13.5)
- have cleats welded to them, palatally or lingually
- can have triple tubes if two arch wires are being used and headgear (EOT) can also be fitted
Figure 13.5 Band with triple tube (for EOT).

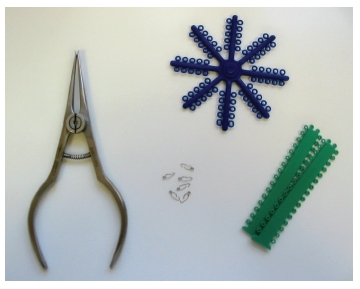
Figure 13.6 Green anterior and blue posterior separating rings, separating springs and separating pliers.
Separation
Bands cannot be fitted in cases of crowding and tight contact points unless the patient has worn separating modules to create an interproximal space to allow the band to be seated comfortably and accurately. These are fitted several days prior to the band fitting to open the contact point. They are placed between the teeth using separating pliers. Springs are occasionally used, placed by pliers, especially for partially erupted teeth (Figure 13.6).
Brackets
They can be made of
- metal (Figure 13.7a):
- stainless steel
- are the most commonly used in the growing patient, are tooth-friendly, not as hard as ceramic brackets not likely to fracture with a direct blow (sports, etc.)
Figure 13.7 (a) Metal bracket with hook. (b) Aesthetic bracket.
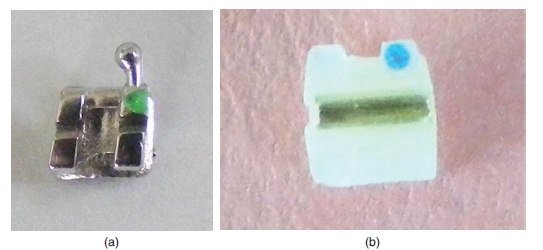
- aesthetic (Figure 13.7b):
- tooth coloured or clear
- not as noticeable
- superior aesthetics
- preferred by adults
- often have metal insert in the arch wire slot as metal slides well over metal which results in less friction and more efficient movement of teeth
- slightly bulkier
Brackets can be:
- fixed to the labial and buccal surfaces of the teeth. This is more easily accessible for the clinician but is visible
- fixed to the lingual (palatal and tongue) surfaces of the teeth, when it is not visible
- self-ligating or conventional requiring the arch wire to be held into the bracket with ligatures or O-rings
They have a rectangular section channel (slot) in the bracket which houses the arch wire. Round section wires do not fit as snugly as rectangular wires. This allows some ‘play’ while rectangular wires are more firmly engaged.
- Brackets are almost always of the pre-adjusted design
- The prescription dictates the levels of tip and torque
- (torque is the correction of inclination labiolingually)
- These can be to different prescriptions, e.g. Roth, Andrews and MBT
- Each tooth has its own prescribed individual bracket
- Pre-adjusted brackets developed from the Begg technique are marketed as the Tip Edge system
Figure 13.8 APCTM PLUS adhesive coated appliance system. (Reproduced with permission of 3M Unitek. © 2010 3M Unitek. All rights reserved.)

The arch wire is held positively in the bracket by:
- a metalligature
or
- an elastomeric
Some self-ligating brackets do not use this method
- they have a latch built into the bracket itself, which makes it self-ligating
- the latch is opened to insert or remove the arch wire using a special tool that opens and closes the latch
Brackets can either be
- fixed to the tooth by applying composite adhesive in the surgery
- come from the manufacturer ready pre-coated with adhesive (Figure 13.8)
There are two techniques for doing this:
- Direct bonding – fixing the individual attachments directly onto the teeth (most commonly used)
- Indirect bonding – positioning them on a model, transferring them to a tray, placing tray in mouth and curing them together through it
It is crucial that the brackets are placed very accurately, because if they are at the wrong height or angulation the tooth will not subsequently align correctly.
Figure 13.9 Metal brackets on orientation card.
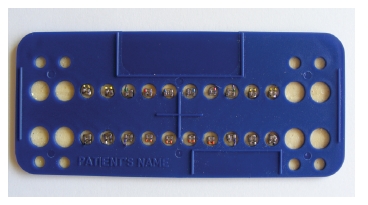
Brackets are:
- usually mounted on orientation cards for ease of delivery (Figure 13.9)
- often have a coloured identification dot to show which way up they are and for which tooth
- some have angles of torque as well as tip built into the wire slot
- popular prescriptions are Roth, Andrews and MBT (McLauglin, Bennett and Trevisi)
- canine brackets can have ‘hooks’ to aid elastic wear
- osteotomy patients often need hooks on canines and premolars
- bases are textured for extra glue retention
- are contoured to the surface of the tooth
Very occasionally a Begg bracket is used as single attachments together with a removable appliance which uses a whip arm spring to extrude or intrude a tooth.
Brackets can be supplied with gold chain attached to them (These are fitted in theatre under general anaesthesia when patients are having ectopic canines exposed).
Buccal tubes
/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


