Q. 2. What are the aetiological factors of osteomyelitis of mandible.
Or
Classify osteomyelitis. Write in detail about the aetiology, clinical features, radiographic features and management of chronic suppurative osteomyelitis.
Ans.
• Osteomyelitis is defined as an inflammatory condition of the bone that begins as an infection of medullary cavity and the Haversian system and extends to involve the periosteum of the affected area.
Classification of osteomyelitis
Based on location
Based on duration and severity
Based on presence or absence of suppuration
Chronic suppurative osteomyelitis
• Chronic osteomyelitis is the persistent abscess of the bone characterized by the complex inflammatory process including necrosis of mineralized and marrow tissues, suppuration, resorption, sclerosis and hyperplasia.
• Chronic suppurative osteomyelitis exists when the defensive response leads to the production of granulation tissue, which subsequently forms dense scar tissue in an attempt to wall of the infected areas.
• The encircled dead space acts as a reservoir for the bacteria and antibiotic medication will have difficulty in reaching the site.
• The disease may be acute, subacute or chronic and presents with a different clinical course, depending on its nature.
Predisposing factors
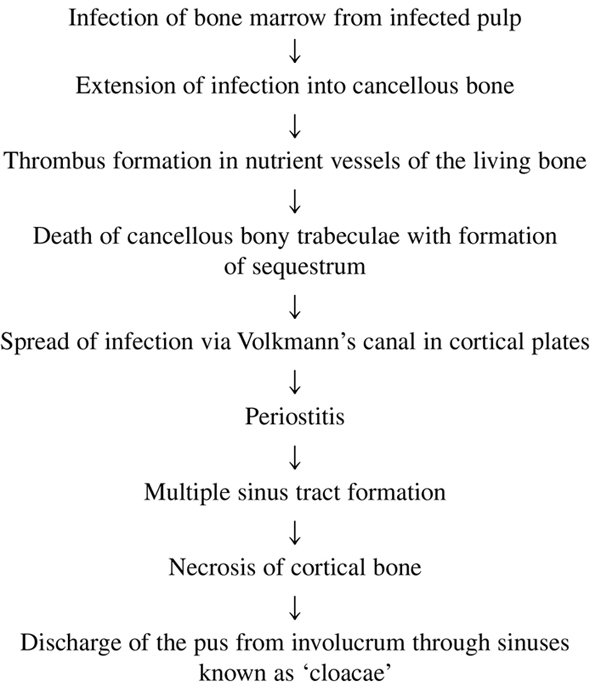
Pathogenesis
Clinical features
• If the acute osteomyelitis is not resolved expeditiously, the entrenchment of chronic osteomyelitis occurs, or the process may arise primarily without a previous acute episode.
• Swelling, pain, sinus formation, purulent discharge, sequestrum formation, tooth loss or pathologic fractures may occur.
• Patients may experience acute exacerbations or periods of decreased pain associated with chronic smoldering progression.
• The molar area of mandible is more frequently affected.
• Pain is usually mild and insidious and is not related to the severity of the disease.
• Jaw swelling is common feature but mobility of teeth and sinus tract formation are rare.
• Regional lymphadenopathy is common.
• There is thickened, woodened feeling of bone and slow increase in jaw size.
Radiographic features
• Radiography reveals a patchy, ragged, and ill-defined radiolucency that often contains a central radiopaque sequestra.
• On CT scan the osteolytic changes are continuous and may exhibit spread to the periosteum by direct extension.
• Occasionally, the surrounding bone may exhibit increased radiodensity, and the cortical surface can demonstrate significant osteogenic periosteal hyperplasia.
• The main radiographic feature of suppurative osteomyelitis is an expanding radiolucent osteolytic changes instead of the potential for peripheral sclerosis.
Treatment and prognosis
• Chronic osteomyelitis is difficult to manage medically, presumably because pockets of the dead bone and organisms are protected from antibiotic drugs by the surrounding walls of the fibrous connective tissue.
• Surgical intervention is mandatory.
• The most frequently used antibiotics are: penicillins, clindamycin, cephalexin, cefotaxime, tobramycin and gentamicin, but these antibiotics should be used intravenously and in high doses.
• The extent of the surgical intervention depends on the spread of the process; removal of all the infected material down to good bleeding bone is mandatory in all cases.
• For small lesions, curettage, removal of necrotic bone and saucerization are sufficient.
• In patient with more extensive osteomyelitis, decortication or saucerization is combined with transplantation of cancellous bone chips.
• In case of persisting osteomyelitis, resection of the diseased bone followed by immediate reconstruction with an autologous graft is required.
• Weakened jaw bones must be immobilized.
• The goal of the surgery is removal of all infected tissue.
• Persistence of chronic osteomyelitis is typically the result of diseased tissue.
Q. 3. Enumerate viral lesions occurring in the oral cavity and discuss in detail about acute herpetic gingivostomatitis.
Or
What are the viral infections in the oral cavity? Write about the aetiology, clinical features, diagnosis and differential diagnosis of acute herpetic gingivostomatitis.
Ans. The viral infections of oral cavity are classified depending on the presence of the major viruses as follows:
RNA viruses
DNA viruses
Herpes simplex virus
• Herpes simplex is a DNA virus, which causes the disease in the man.
• The tissues preferentially involved by herpes simplex virus are often referred to as herpes virus hominis and are derived from ectoderm principally the skin, mucous membranes, eyes and central nervous system.
• Two types of infections occur with herpes simplex virus:
• Primary herpetic infections may manifest clinically as primary gingivostomatitis, primary vulvovaginitis, inoculation herpes simplex, varicelliform eruption, meningoencephalitis, disseminated herpes simplex. Subclinical primary infection is common in 99% of cases the primary infection is subclinical with no visible clinical disease.
• Recurrent herpetic manifestations include fever blister, genital herpes simplex and dendritic corneal ulcers.
• HSV2 is associated with carcinoma of uterine cervix; HSV does not remain latent at site of original infection; reaches regional ganglia along the nerve path; HSV1 seen in trigeminal and HSV2 in lumbosacral ganglions.
Herpetic gingivostomatitis
Clinical features
• Herpetic gingivostomatitis is a common oral disease transmitted by droplet spread or contact with the lesions.
• This infection occurs in the persons who are not infected previously with herpes virus or they do not have circulatory antibodies against virus.
• It affects children and young adults.
• Disease occurring in children is frequently the primary attack and is characterized by the development of fever, irritability, headache, pain up on swallowing and regional lymphadenopathy.
• Within a few days mouth becomes painful, and the gingiva becomes intensely inflamed and appears erythematous and oedematous.
• Lips, tongue, buccal mucosa, palate and tonsils may be involved. Shortly, yellowish fluid filled vesicles develop in oral cavity.
• These vesicles rupture to form painful ulcers covered by grey membrane and surrounded by erythematous halo.
• Healing occurs in 7−14 days and leave no scar.
• Herpetic whitlows in hands of hospital staff and disseminated infection of new born are examples of primary herpetic infections.
Histological features
• Intra-epithelial fluid-filled vesicles
• Intranuclear inclusions known as Lipschutz bodies are present, these are eosinophilic, ovoid homogeneous structures within the nucleus.
• Perinuclear halo in nucleus produced by displacement of chromatin peripherally by Lipschutz bodies.
• Cytoplasm of infected cells forms giant cells and subjacent connective tissue is usually infiltrated by inflammatory cells.
Diagnosis
Treatment
Differential diagnosis
Q. 4. What are the predisposing factors of acute necrotizing ulcerative gingivostomatitis? How will you diagnose and treat a patient suffering from this disease?
Ans.
Aetiology
Role of bacteria
Local predisposing factors
• Poor oral hygiene, pre-existing marginal gingivitis and faulty dental restoration.
• Area of gingiva traumatized by opposing in maloccluded teeth such as the palatal surface behind maxillary incisors and labial gingival surface of mandibular incisors.
Systemic predisposing factors
Clinical features
Oral signs and symptoms
Signs
• Characterized by punched out, crater-like depressions at the crest of the interdental papillae, subsequently involving marginal gingival and rarely attached gingiva.
• Craters are covered by greyish pseudomembranous slough with a marked demarcation of linear erythema from the normal mucosa.
Symptoms
Extraoral and systemic signs and symptoms
Mild-to-moderate stages
Severe cases
Systemic reactions
Histopathology
• It involves both stratified squamous epithelium and underlying connective tissue.
• The surface epithelium is destroyed and is replaced by pseudomembranous meshwork of fibrin, necrotic epithelial cells, polymorphonuclear neutrophils and various microorganism that appears as a surface pseudomembrane.
• The underlying connective tissue is hyperaemic with numerous engorged capillaries and dense infiltration of polymorphonuclear neutrophils, which appears as a linear erythema.
• Numerous plasma cells may appear in periphery of infiltrate.
Treatment
• The conservative treatment is superficial cleaning of oral cavity by chlorhexidine, diluted hydrogen peroxide or warm salt water. This is followed by scaling and polishing under topical anaesthesia.
• Use of antibiotics is coupled with local treatment in patients with toxic systemic complications.
Q. 5. Describe the clinical features and treatment of actinomycosis of the jaw.
Ans.
Clinical features
• Actinomycosis is mostly found in young adults. Women are less frequently affected than men.
• Based on the site of involvement, actinomycosis can be grouped into the cervicofacial, pulmonary, abdominal and pelvic and cutaneous and genitourinary actinomycosis.
• Cutaneous actinomycosis is extremely rare and these are said to arise from wounds contaminated with saliva or as a consequence of haematogenous dissemination following a dental procedure.
• However, primary cutaneous actinomycosis have also been reported.
• The genitourinary form has been reported in patients using intrauterine contraceptive devices.
• The presenting symptoms of pulmonary actinomycosis are fever, cough thoracic pain and dyspnoea.
• The sputum is mucopurulent or even sanguineous. With the appearance of fistulae, the disease spreads to the mediastinum, the pericardium and finally to the skin of the chest.
• Actinomycosis is believed to be acquired by endogenous implantation into deep tissues where anaerobic conditions prevail.
• Actinomyces israelii is an anaerobic normal inhabitant of the mouth, especially in the teeth and tonsils.
• In the cervicofacial region, puncture wounds, dental extractions or compound fractures are some of the routes of infection.
• The cervicofacial variant is characterized by the appearance of solid sub- or supramandibular nodules or swellings and the overlying skin becoming purple to violet.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


