Abrasion, Finishing, and Polishing
Chapter Objectives
On completion of this chapter, the student will be able to:
1. Define abrasion, finishing, polishing, and cleansing.
3. Identify the factors that affect the rate and efficiency of abrasion.
4. Compare the relative ranking of abrasives on restorations and tooth structures.
5. Identify methods by which dental abrasives are applied.
6. List the contraindications to the use of abrasives on tooth structure and restorations.
10. Describe the safety and infection control precautions taken by the operator when using abrasives.
KEY TERMS defined within chapter
Grit the particle size of the abrasive, typically classified as coarse, medium, fine, and superfine
Margination a procedure for removal of excessive restorative material from margins of restorations
Flash feather-like excesses of material present on occlusal and proximal surfaces
Overhang excessive material present at the cervical cavosurface margin
Proper finishing, polishing, and cleaning of tooth structures and restorative materials is clinically relevant because this improves esthetics, improves tissue health, and increases the longevity of the restorative material.
The removal of stains and soft deposits after scaling and root planing must be a selective procedure performed after the needs of the individual patient are considered and must not be performed on a routine basis.
The goal of finishing and polishing restorations, intraoral appliances, and tooth structure is to remove excess material, smooth roughened surfaces, and produce an esthetically pleasing appearance with minimum trauma to hard and soft tissues. The finishing and polishing of a surface involves removing marginal irregularities, defining anatomic contours and occlusion, removing the surface roughness of the restoration, and producing a mirror-like surface luster. Many benefits are derived from smooth tooth surfaces, restorations, or appliances in the intraoral environment. A smooth surface resists accumulation of soft deposits and stains, is less irritating to the gingival or mucosal tissue, and is esthetically pleasing because it reflects light better. A smooth, highly polished restorative surface is more resistant to the effects of corrosion and surface breakdown. A properly finished and polished surface will contribute to the appearance and longevity of the restoration or appliance and the health of the surrounding oral tissues (Figure 12-1). Clinicians who perform these functions must have a clear understanding of the factors that cause and control abrasion. Improper use of abrasives can lead to roughening and overreduction of tooth and restorative surfaces. The clinician must be able to recognize that different types of tooth structures and restorative surfaces abrade differently and must use the proper protocol for finishing, polishing, or cleansing that surface. It is also the clinician’s responsibility to teach the patient how to properly care for the surface with home care devices and how to prevent the staining habits that diminish their appearance.

Finishing and Polishing
The process of finishing and polishing involves using a diminishing series of abrasives on a surface to first contour, then smooth, and finally bring a luster to the surface. Finishing uses abrasives to produce the final contour of a restoration. Polishing is the process of abrading the surface of a restoration with a series of particles, causing scratches, coarse to fine, to produce a surface smooth enough to be esthetically pleasing, well tolerated by soft tissues, and resistant to biofilm adhesion. The effect of abrasion is directly related to the properties of the abrasive and the material it is abrading.
Factors Affecting Abrasion
An understanding of the properties of abrasives and the factors that control the rate or efficiency of abrasion will help the clinician make appropriate clinical decisions. The rate of abrasion is determined by size, irregularity, and hardness of the particles; the number of particles contacting the surface; and the pressure and speed with which they are applied. An understanding of these factors will assist the clinician in making appropriate clinical decisions in the control of abrasion.
Size, Irregularity, and Hardness of the Particles
The size, irregularity, and hardness of the abrasive particle determine the depth of the scratches in the material being abraded and therefore the amount of material being removed. An example is the effect of pumice, which comes in several grades of coarseness, on cementum and amalgam. Coarse pumice, a larger and coarser particle, will remove more surface of the softer cementum than the harder amalgam. If flour of pumice, a much smaller and more regular particle than coarse pumice, is used, the effect will be to polish the cementum as well as the amalgam. Diamonds are the most abrasive materials used in dentistry. Diamond abrasives can remove large amounts of tooth structure and restorative material, finish restorations, and polish restorations, all according to diamond particle size and irregularity. Their rate of abrasion will also depend on the material being abraded, the pressure applied, and the speed of the rotating device.
If the surface being abraded is harder than the abrasive, there is little or no effect. It is important for the clinician to have an appreciation for the relative hardness of various intraoral materials and abrasives. Hardness is the ability of a material to resist abrasion. Mohs’ scale ranks materials by their relative abrasion resistance. As seen in Table 12-1, diamond has the highest resistance to abrasion and is therefore considered the hardest; pumice rates a 6 on Mohs’ scale, which is similar to enamel but harder than amalgam and dentin. Therefore pumice may only polish amalgam, whereas it would be abrasive to dentin. It is important to note that porcelain is harder than enamel and dentin. Abrasive wear of tooth structures in contact with porcelain restorations is a problem for many patients. The greater the difference in the abrasive and the surface it is abrading, the faster and more effective the abrasive action is. Compare Mohs’ hardness ranking for enamel and dentin. You can surmise that exposed dentin is abraded at a much greater rate than enamel during dental polishing procedures. Compare Mohs’ ranking of composite and gold. If the same polishing agent is used on these as on enamel, the result would be greater loss of the restorative material.
TABLE 12-1
| Diamond | 10 |
| Silicon carbide | 9–10 |
| Tungsten carbide | 9 |
| Aluminum oxide | 9 |
| Emery | 7–9 |
| Sand–quartz | 7 |
| Pumice | 6–7 |
| Porcelain | 6–7 |
| Tin oxide | 6 |
| Amalgam | 5–6 |
| Enamel | 5 |
| Composite | 3–7 |
| Dentin | 4 |
| Gold | 3 |
| Acrylic | 2–3 |
| Cementum | 2–3 |
The size and shape of the particles is an important consideration in manipulating the abrasive. Particles that are large and irregular will cut more efficiently. The sharpness, or efficiency, of the particle is usually lost with use as the edges break down and the particle no longer grabs the surface. Unlike the shape of the particle, the size of the particle does not always break down with use. Abrasive particles are classified from coarse to fine based on their size measured in micrometers (also called microns). One micrometer, or micron, is equal to one thousandth of a millimeter (10−3) and uses the symbol µm. Abrasives are classified as coarse (particles 100 µm and above), medium (20 to 100 µm), and fine (20 µm to submicron particle sizes). Manufacturers use the term grit to refer to the size of the abrasive particles. Particles are passed through a standardized sieve that allows specific sizes of particles to pass and then categorizes them from coarse through superfine. Prophylactic polishing pastes are commonly manufactured in various degrees of coarseness, as are abrasive disks and rotary diamonds (Figure 12-2). The clinician must make decisions as to the coarseness of the abrasive and the application method needed for each procedure.
Numbers That Contact the Surface
The more concentrated the particles that contact the surface, the more quickly the surface will be abraded. If a lubricant is used to dilute the concentration of the particles, the abrasiveness of the material is reduced. Water and saliva are lubricants commonly used to dilute the effect of abrasion. When using an abrasive, the clinician has control of how much lubricant to add to the material, whether this is done before it is put onto the surface or while it is being used intraorally as it picks up saliva. Pumice is manufactured in a powder or paste, giving the clinician the opportunity to further dilute this abrasive. Rotary cutting instruments such as abrasive disks and stones will lose effectiveness as particles break away from their surface or debris clogs the surface. Many rotary cutting stones and diamonds use the water from the handpiece or three-way syringe to assist in the movement of debris from the cutting edge and act as a surface coolant, thus allowing the surface to maintain its abrasive action much longer.
Speed and Pressure
Increasing the speed and pressure of an abrasive will increase the rate of abrasion. Speed can also produce undesired effects if it results in lack of control. An increase in pressure will cause deeper scratches but also may produce less control of the amount of material being removed. An increase in pressure decreases the clinician’s tactile sensitivity and may produce an undesired overabraded surface. Too much pressure might even reduce the cutting efficiency of the abrasive by decreasing the instrument’s torque. Speed and pressure also produce frictional heat, which may produce a detrimental effect on the tooth structure and on patient comfort. Care must be taken to control the amount of pressure and speed with which abrasives are applied.
Determining the rate of abrasion is an important consideration when clinical decisions are made regarding what type of material is to be abraded, how much material is to be removed, and the desired outcome.
Delivery Design of Abrasives
Dental abrasives are supplied in a number of forms: paste abrasives, loose abrasives, coated abrasives, and bonded abrasives (Figure 12-3).
Paste Abrasives
Paste abrasives are found in the form of prophy paste and toothpaste. A more complete discussion of both follows under Preparations Used for Abrasion.
Loose Abrasives
Loose abrasives are manufactured in powders and pastes and are classified by their grit or particle size. Grits that are coarse, medium, fine, and superfine are available for finishing, polishing, and cleansing surfaces. These may be applied with wheels, brushes, cups, or soft pads. The concentration of particles that contact the surface is clinically controlled. If the clinician uses a coarse, dry paste, rapid removal of surface material will result, along with possible pulpal damage due to excessive frictional heat. However, if a superfine, highly diluted paste is used, little or no material may be removed. The proper grit and dilution of the loose abrasive must be considered to obtain the best results in finishing and polishing a given surface.
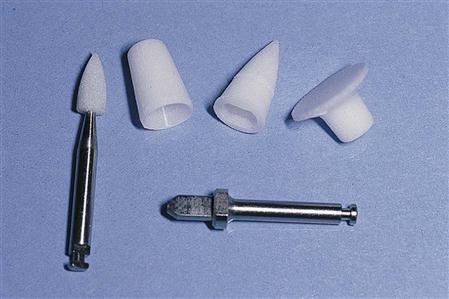
Bonded Abrasives
Bonded abrasives are attached to rotary instruments and have an abrasive particle uniformly incorporated in a binder to form the shape of the device. Shapes vary in form; points, disks, cups, brushes, and wheels are available. These devices are frequently used for intermediate finishing and initial polishing of restorations (Figure 12-4).
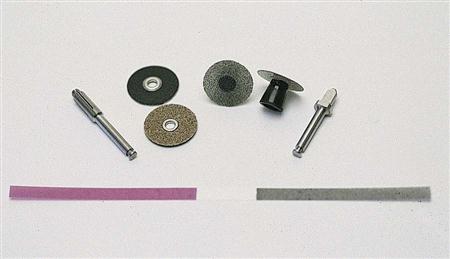
Coated Abrasives
Coated abrasives are supplied on rotary disks and handheld finishing strips. The abrasive particles are secured to one side of a flexible backing with an adhesive. Devices with coating on only one side protect the adjacent tooth from the abrasive and are referred to as safe-sided. Flexible backing such as paper or plastic gives them the advantage of flexibility but eliminates their ability to be sterilized. Coated abrasives on rotary devices use sterilizable mandrels for convenience and cost-effectiveness (Figure 12-5).
Abrasives are manufactured for use in the laboratory or at chairside. Some may be used for either purpose. Regardless of how the abrasive material is supplied, the rate of abrasion must be controlled by the clinician.
Materials Used in Abrasion
Many types of natural and synthetic (human-made) materials are available for use in dentistry. As listed from most to least abrasive, each of these materials leaves the surface of the restoration or tooth structure with varying degrees of roughness.
Diamond
Diamond is the hardest substance known, rating a 10 on Mohs’ hardness scale. It will efficiently abrade any substance. Rotary diamonds are expensive and usually are not disposable, so they are found most often bonded in varying degrees of coarseness to rotary cutting shanks or disks. They are sterilizable and have the capability of being reused several times before they wear out. Fine-particle diamonds come in a paste for polishing composite and porcelain restorations. They are used to cut crown and bridge preparations and to finish and polish composite restorations.
Carbide Finishing Burs
Tungsten carbide finishing burs come in several shapes, with designs ranging from 7 to 30 cutting flutes. The higher the number of flutes the bur has, the finer is the final finish. A bur that contains only seven flutes will have a very aggressive cutting action. These burs rank up to 9 on Mohs’ scale and are used primarily for finishing. They are used to cut preparations or to finish composite restorations.
Silicon Carbide
Silicon carbide is a synthetic material that produces an extremely hard and efficient abrasive material, Mohs’ 9 to 10. Silicon carbide–coated disks and bonded rotary devices are used primarily in finishing procedures.
Aluminum Oxide
Aluminum oxide is a synthetic abrasive that is often manufactured in a white or tan powder. The powder form is used in sandblasting restorations in preparation for cementation and air abrasion. It is used in bonded and coated rotary devices. Aluminum oxide–impregnated rubber wheels are called Burlew wheels. This popular abrasive comes in several grits and has largely replaced emery. It is used to smooth enamel or to finish metal alloys and ceramic materials.
Sand
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses