Chapter 10
Nerve Involvement in Oral and Maxillofacial Surgery
Nerves can be injured when surgery is performed in the maxillofacial region. Knowledge of anatomy is important to avoid and prevent nerve injuries. The possibility of nerve injuries must always be explained to patients prior to surgery so the patient understands the risks and be part of the decision to carry out surgery when there is risk for nerve injuries.
Trigeminal Nerve
Injury to the terminal sensory branches of the trigeminal nerve (the lingual nerve, the inferior alveolar nerve, and the long buccal nerve) is relatively frequent and can occur as a result of many different forms of dental treatment.
Nerve Injuries as a Result of Inferior Alveolar Nerve Block
It is known that both temporary, and occasionally permanent, nerve damage can occur as the result of an inferior alveolar nerve block. The nerve predominantly affected appears to be the lingual nerve, which is affected approximately twice as often as the inferior alveolar nerve. The exact cause of injury with an inferior alveolar nerve block is unknown, but suggestions have included direct trauma from the needle in some way, hematoma to the nerve, or a neurotoxic effect from the local anesthetic itself. The incidence is unknown with estimates of permanent nerve damage resulting from inferior alveolar blocks varying from 1 in 20 000 inferior alveolar nerve blocks to 1 in 850 000 inferior alveolar nerve blocks. Transient damage from inferior alveolar nerve block probably occurs five or six times as frequently. Most cases recover within an 8–10 week-period, and a smaller number recover over a 9-month period. About 10% of cases prove to be permanent, with occasional disabling dysesthesia.
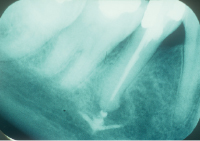
Inferior Alveolar Nerve Damage from Root Canal Treatment
Root canal therapy carried out on lower molars and premolars may damage the inferior alveolar nerve either from direct trauma from over instrumentation, from a hydrostatic pressure phenomenon or neurotoxicity from extruded root canal sealant (Fig. 10.1). Surgical removal of the material may be necessary in such cases.
Nerve Damage from Dental Implants
The insertion of osseointegrated implants into the mandible has the potential to damage the inferior alveolar nerve and mental nerves due to overextension (Fig. 10.2). Today, with cone-beam computer tomography (CBCT), the distance to the nerve can be measured and installation depth and direction better planned prior to surgery (Fig. 10.3). Cases can also occur from implants inserted anterior to the mental foramen if consideration is not given to forward looping of the inferior alveolar nerve before it exits the mental foramen.
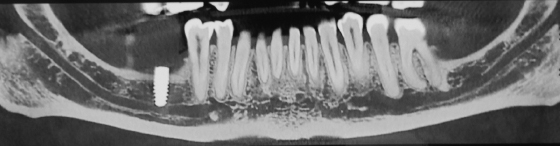
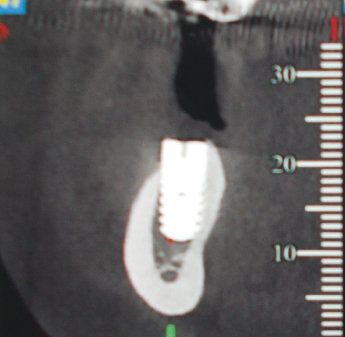
If there is anesthesia or paresthesia of the inferior alveolar nerve following implant insertion, once the local anesthetic has dissipated, consideration should be given to obtaining a cone-beam CT scan to accurately relate the position of the implant to the nerve, and early consideration should be given to removing the implant. This can be successful in the early stages when the involvement is due to pressure alone from the implants or hydrostatic pressure. However, many cases do not recover, presumably since the damage is more profound or was caused by the twist drill.
Periodontal Surgery
Periodontal surgery in the form of the distal wedge procedure and extensive surgery or deep root planing on the lingual side in the lower molar region can cause damage to the lingual nerve, particularly when the nerve lies in an aberrantly superior position as is known to occur in between 15 and 20% of cases (Fig. 10.4). In these cases the nerve can lie at the level of the crest of the lingual alveolar bone or even slightly above it. If periodontal surgery is to be performed in these areas, the surgeon must have knowledge of the possible aberrant positions of the lingual nerve and take this into account when performing the surgery. If the nerve is damaged with a sharp instrument such as a scalpel, early surgical nerve repair may give satisfactory results.

Dentoalveolar Surgery and Nerves
Dentoalveolar surgery carried out on the posterior mandible can cause damage to the lingual nerve, the inferior alveolar nerve, the long buccal nerve, and even the mylohyoid nerve. The commonest dentoalveolar procedure carried out in this area is third molar removal, but other surgical procedures in this area have also the potential to cause damage.
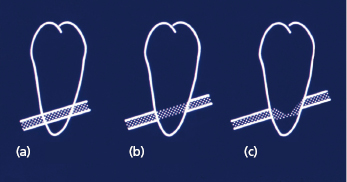
Inferior Alveolar Nerve
The incidence of inferior alveolar nerve damage from the removal of third molars varies in the literature from 0.5–5%. The cause is directly related to the anatomical relationship between the inferior alveolar nerve and the roots of the third molar. In many cases, this can be determined from panoramic radiograph, and criteria have been developed to determine more exactly from a panoramic radiograph the relationship of the inferior alveolar nerve to the tooth. This is shown in Figure 10.5. When the image of the inferior alveolar canal is superimposed over the tooth with no loss of lamina dura of the canal and no narrowing or change of direction, the relationship is probably one of superimposition with a low risk of nerve involvement as shown in Figure 10.5a. If, however, the nerve loses its lamina dura it may in fact be grooving the tooth, and the risk of inferior alveolar nerve involvement on removal of the tooth may be higher, as shown in Figure 10.5b. Figure 10.5c shows loss of the lamina dura, narrowing, and possible deviation of the path of the inferior alveolar canal and denotes an intimate relationship between the tooth and the nerve with a high risk of nerve involvement that may be 50% or higher. A pair of periapical films, taken at different angulations, may reveal relationships between the roots and nerves, by applying the parallax principle of movement (“same lingual, opposite buccal”). Cone-beam CT technology can now accurately show the relationship of the inferior alveolar nerve to the third molar in three dimensions and this has helped to quantify the issue of the risk involved in the removal of such teeth. Where suitable imaging shows an intimate relationship between the roots of the third molar and the inferior alveolar nerve, a decision must be made whether to proceed with the removal or not, or possibly consider intermediate strategies such as coronectomy or partial tooth removal whereby the portion of the root intimately related to the inferior alveolar nerve is left behind. Studies show that this is a safe and predictable technique with a high success rate in avoiding injury to the inferior alveolar nerve, although some of the roots may later move and some may even require subsequent removal.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


