1
Symptoms, Clinical Characteristics and Consequences
Introduction
This chapter will discuss the underlying factors concomitant with dental fear and anxiety and dental phobia and how such different symptoms interact in the maintenance of the irrational fear and possible future consequences. In the text fear and anxiety will be used interchangeably. However, phobia has another grading, which is related to the definition according to DSM-IV, and will not be interchanged with other terms.
The phenomena of dental anxiety, where individuals typically show different signs and symptoms related to dental care, have been revealed to be similar, irrespective of country, culture and other living conditions (Armfield, Spencer and Stewart 2006; Hakeberg, Berggren and Carlsson 1992; Milgrom et al. 1988; Moore et al. 1993; Neverlien 1990; Stouthard and Hoogstraten 1990).
The prevalence of high dental anxiety ranges between 3 per cent and 10 per cent depending on measurement methods and sample selections. Moreover, since the first scientific reports on the epidemiology of dental anxiety it seems that it is as common today as it was 40 to 50 years ago (Armfield et al. 2006; Freidson and Feldman 1958; Hakeberg et al. 1992; Milgrom et al. 1988; Moore et al. 1993; Neverlien 1990; Stouthard and Hoogstraten 1990). We may ask why the prevalence has not changed during this period of time despite the continuing progress of dental care. Greater awareness of the problem, technological advances and better undergraduate curriculum and postgraduate education should possibly have decreased the prevalence of dental anxiety. One answer may be that the majority of the group of individuals with moderate dental anxiety has become less anxious. Several scientific reports indicate such a development when comparing cohorts over time in repeated cross-sectional studies (Hägglin 2000). However, there are still individuals who are highly fearful of dental care and procedures. These persons report that being highly fearful or even phobic of dental care affects their life situations in many different ways. This chapter introduces the major symptoms related to high dental anxiety or dental phobia.
Figure 1.1 A systems-oriented multi-causality model where different factors of physiological, psychological and social character interact in the development and maintenance of diseases. Modified from Carlsson and Jern 1982
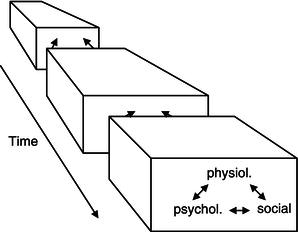
Since the 1970s a large amount of research literature has shown that individuals with reported dental anxiety and phobia are also affected by different negative manifestations and consequences related to physiological, psychological and social aspects of their health and life situations. In such a perspective we may relate to Carlsson and Jern’s (1982) theoretical model, which describes a specific causal theory and a paradigm shift concerning the relationship between biological, psychological and social factors (Figure 1.1). They suggested a systems-oriented multi-causality model where different factors interact in the development of a disease. It is assumed that social, psychological and physiological components are in constant interaction with each other, leading over time to psychological, social and somatic changes. Such changes affect the successive interaction.
The vicious circle of dental anxiety
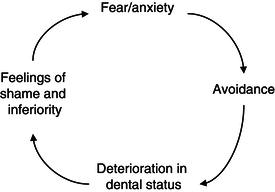
Applying this perspective to dentistry, Berggren presented a model that describes several components of the effects from severe dental anxiety resulting in the establishment of a vicious circle (Berggren 1984; Berggren and Meynert 1984). Such a vicious circle, or rather vicious cycle, since time is an important component in the development of disease and illness, is shown in Figure 1.2. A person’s initial fear and anxiety may lead to an avoidance of or irregular dental care. This can mean irregular dental visiting habits with only emergency dental treatments, or even total avoidance. If necessary treatment is not carried through then oral health may be affected negatively, for example, with the development of carious lesions in the teeth as well as a progress of periodontitis. Thus, deterioration of the oral status starts to progress, causing the individual to be aware of the effects on their oral health. Not being able to carry through with regular dental care and treatment may further initiate feelings of inferiority, shame and embarrassment about the situation and for a dentally anxious individual such feelings may over time give rise to obvious social problems in daily life situations such as during contact with people at work, with friends or relatives and/or at home within the family. With time, this pattern of effects may lead to higher and more widespread anxiety of dentistry and eventually less regular dental care or even avoidance of dental treatment.
Figure 1.2 The vicious cycle model of dental anxiety and fear according to Berggren 1984
Measurements of dental anxiety
Dental anxiety may be seen as a phenomenon measured on a continuum, from no anxiety to extreme anxiety. Several different measurement scales have been used in scientific studies. Global, single-item questions are frequent, via a visual analogue scale (VAS) and verbal rating scales using a Likert format (Hägglin et al. 1999; Milgrom et al. 1988; Pohjola et al. 2009). However, multiple item scales such as the Dental Anxiety Scale (DAS) (Corah 1969), the Modified Dental Anxiety Scale (MDAS) (Humphris, Morrison and Lindsay 1995), the Dental Fear Survey (DFS) (Kleinknecht and Bernstein 1978) and the Dental Anxiety Inventory (DAI) (Stouthard, Hoogstraten and Mellenbergh 1995) are applied more often. Armfield (2010a) has published a new measure of dental fear (Index of Dental Anxiety and Fear, IDAF-4C+) based on DSM-IV specific phobia categories and of emotional, behavioural, physiological and cognitive components of the anxiety and fear response. Although the IDAF-4C+ is promising, only a few studies have used the measure, implicating the need for obvious psychometric testing concerning reliability and validity in different samples of specific and general characters. Multiple item scales are often used with a cut-off value to identify highly dentally anxious subjects. Among other things, one problem with the analyses which use a transformation of a scale to dichotomize a variable after a specific value is that information about subjects may be lost. In addition, the scaling of the tests sometimes infers ceiling and/or floor effects which may hamper the interpretation of how anxious individuals really are. Such methodological aspects are important when analysing characteristics and consequences of dental anxiety among patients or individuals.
Another issue that should be taken into account is the differences between the subjects included in the scientific reports on dental anxiety. Generally, two different sample selections have been used in the research designs. Firstly, clinical samples of highly dentally anxious individuals or dental phobic subjects have been included in experiments using different treatments for dental anxiety. Typically, different aspects of negative effects of dental anxiety have been reported in these studies, but subjects have more or less also avoided dental care completely or nearly completely for a longer period of time. Thus, such clinical samples may describe a narrower effect of dental anxiety on negative consequences, such as health and psychosocial effects. Subjects attending special clinics for the treatment of high dental anxiety or dental phobia with avoidance behaviours of ordinary dental care usually show important and negative impacts on health and psychosocial consequences. However, when examining subjects randomly selected from the general population, who report high dental anxiety or dental phobia, the effects on health and psychosocial consequences show a wider spectrum with regard to these outcomes. This difference, is important to bear in mind when evaluating the symptoms, characteristics and consequences of dental anxiety due to the selected study sample. Having said this, this chapter will illuminate both types of study sample selections and associated impact on health and psychosocial factors.
Symptoms, Characteristics and Consequences of Dental Anxiety and Dental Phobia
The different symptoms, characteristics and consequences of dental anxiety, dental phobia and injection phobia (IP) are described below with regard to oral health, dental attendance behaviours, psychological and physiological factors. The effects of dental anxiety described in this chapter use the theoretical model of Berggren’s vicious circle; and results from both clinical and observational studies will be shown to exemplify important factors associated with the phenomena of dental anxiety.
Avoidance of dental care
Avoidance of dental care and treatment is usually a strong predictor of high dental anxiety. Individuals with dental phobia are, according to the defined criteria of phobia in DSM-IV, avoiders of dental care. However, in both clinical samples and observational studies there is a variability in the degree of avoidance behaviour. The measurement of dental attendance is mostly by self-reported data by the subjects, and concerns the last visit to a dental clinic or frequency of regular visits to a dental clinic (Armfield et al. 2006; De Jongh, Schutjes and Aartman 2011; Hägglin 2000; Pohjola et al. 2009). These measures vary in different studies, albeit there is reasonable congruence between reports. In general, there is an abundance of data supporting the association between high dental anxiety or dental phobia and irregular dental visiting habits regardless of culture and country. In an attempt to describe different categories of dental visiting habits, Milgrom discussed individuals’ level of dental anxiety and choice of regular dental care via an approach–avoidance conflict to dental care (Milgrom 1985). Four types of patient categories were allocated. Firstly, subjects that feel low to moderate dental anxiety have regular dental care. Secondly, moderate to high dentally anxious subjects visit the dentist on a regular basis and may, according to Milgrom (1985), be characterized as ‘goers but haters’. However, individuals in both of these categories may be vulnerable in the sense that they probably can change their visiting patterns to the dentist. Why and what factors can change the balance to more avoidance are not clarified, but speculation may include a negative treatment experience such as extreme or unexpected pain, or more cognitive aspects such as poor communication between the care-giver and the patient. Despite their regularity of dental care, patients in these categories may benefit from specific dental anxiety treatment, so as to alleviate their vulnerability to a change in dental visiting habits. The third category includes patients with high dental anxiety or possibly border dental phobia and are partial avoiders. Such individuals may accept emergency treatments and sometimes conventional dental care, but on an irregular basis. Finally, the last category includes subjects that have full avoidance behaviour of dental care, i.e. they do not go to the dentist at all.
Clinical studies
Internationally there are a few specialized clinical centres that have been organized and characterized by both patient treatments and clinical research. The clinics have different experiences depending on when and where they were established. However, these clinics are and have been using a referral system for patients and thereby have described systematically the patients with regard to their high dental anxiety levels and importantly, their inability to tolerate conventional dental treatment. In addition, the patients are mostly characterized by avoidant behaviour to dental care indicating irregular visiting habits. Among these clinics are centres in Gothenburg, Sweden; Bergen, Norway; Amsterdam, Netherlands; and Seattle, USA. These research centres have had a large and important impact on the development of treatments for dental anxiety, the knowledge of how and to what extent factors concomitant to dental anxiety and phobia develop over time and their impact on patients’ life situations. Avoidance behaviour of dental care associated with dental anxiety is clearly one of several important factors that research at these centres has been able to document. Keeping in mind that the patient groups have been and are special with regard to levels of dental anxiety and phobia, the range of avoidance time for dental care is estimated between 5 and 20 years among extremely dentally anxious patients or dental phobic individuals as reported from a variety of clinics and there is a clear and significant association between level of dental anxiety and length of avoidance (Aartman et al. 2000; Abrahamsson et al. 2003, Berggren 1984, De Jongh et al. 2011; Hakeberg et al. 1992; Moore, Brodsgaard and Birn 1991). A history of missed and cancelled dental appointments may be a reliable source to investigate if a person exhibits dental fear reactions. Avoidance of dental care plays an important role in escalating the manifestations and consequences of dental fear. It affects the level of dental fear, the magnitude of psychosocial effects and certainly most often the dental status (Berggren and Meynert 1984). For a majority of individuals with dental anxiety and an avoidance behaviour of dental care the deterioration of their dental health may progress over time at a different pace, but their awareness of the problem is definitely at hand and the size of the problem may also become a stigmata. Social pressure from surrounding family and friends and support may for some individuals reduce the level of avoidance (Berggren and Meynert 1984). Such pressure and support may also include other ways to conclude, e.g. dental care through treatment under general anaesthesia or sedation, thus using more expensive dental care.
Observational studies
There are many scientific publications during the past decades that show a statistically significant correlation between dental anxiety and avoidance of dental care among subjects in the general population (Hakeberg et al. 1992; Hägglin et al. 1996; Locker, Liddell and Burman 1991, Moore et al. 1993; Vassend 1993). Such associations are found both with regard to last visit to a dentist and regularity of dental visiting habits. Moreover, it has been shown that this relationship has a gradient, indicating that the higher the level of dental anxiety the longer the time of avoidance (Locker et al. 1991).
Oral health among individuals with extreme dental anxiety
Clinical studies
Surprisingly, the effects and consequences of severe dental fear and an avoidance behaviour on individuals’ dental status have not been established thoroughly in earlier research, maybe due to an empirical and an expected obvious relationship.
Table 1.1 The difference in oral status in a clinical study (Hakeberg et al. 1993) including a group of dental phobic patients (N = 90) and a group of ordinary dental patients (N = 90). Mean numbers and standard deviations are displayed.
| Oral status | Dental anxiety group | Control group |
| Missing teeth | 4.4 (4.9) | 2.5 (2.9) |
| Caries (surfaces) | 19.5 (11.1) | 7.9 (5.3) |
| Apical periodontitis | 4.0 (4.7) | 1.2 (1.6) |
| Marginal periodontitis (no. of tooth surfaces >4 mm) | 5.0 | 1.0 |
| Filled surfaces | 8.1 (6.4) | 13.1 (9.1) |
Berggren and Meynert (1984) found in a group of extreme dental fear patients that the oral status was more deteriorated, with respect to decayed surfaces, missing teeth, apical lesions (mean number 37, 5, 4, respectively) and periodontal disease (on average, marginal bone loss ≤ ⅓ of the root length), than would be expected in ordinary dental patients of similar age group. This study did not include a non-anxious comparison group. Hakeberg et al. (1993) investigated the oral health in a group of patients with extreme dental anxiety and an avoidance behaviour of dental care. A control group of ordinary patients with regular visiting dental habits and accepting conventional dental treatment procedures were matched according to age, gender, marital status and housing standard and included in the analysis. The results of the study described a substantial difference in oral status between the groups. There were significantly more missing teeth, higher frequency of caries, apical periodontitis and proximal periodontitis among patients with dental anxiety (Table 1.1). However, the numbers of restored tooth surfaces were significantly fewer among the dentally anxious individuals.
In a similar dental fears clinic in Bergen, Norway, Agdal et al. (2008) examined dental phobic patients according to DSM-IV criteria with regard to their oral status. The patients (N = 40) had extreme dental anxiety and had avoided dental care on average for 11.2 years. Mean missing teeth was about 2 (SD = 3.5) and the mean number of teeth with caries was 6.7 (SD = 4.3). There were differences between the above two studies, however, the oral status is clearly highly affected with regard to several measures on oral health and diseases. Patients attending special clinics for dental fear on a referral basis do have poor oral health and since the avoidance is a feature of the dental anxiety complexity there is a gradient of oral status with age. The older the patient the more worse the oral status is, as compared to younger individuals. Wide Boman et al. (2010) used a single group design with referred dental phobic patients who were examined with respect to their oral health. Results were similar to those in the previous studies with 3.4 (SD = 4.0) and 8.1 (SD = 5.2) for the mean number of missing teeth and decayed teeth, respectively. In the studies by Agdal et al. (2008) and Wide Boman et al. (2010) another outcome was analysed, namely the presence of root remnants. Such a feature may indicate a long-term period of avoidance of dental care and lack of a drive to even consider emergency treatment. In the Agdal et al. study nearly 40 per cent of the sample had one or more root remnants, while the figure was 57 per cent in the Wide Boman et al. study.
Figure 1.3 Two referred patients examined at a special dental fears and research clinic in Gothenburg, Sweden. These patients reported the same level of dental anxiety and the same time of avoidance of dental care. They were both in their early 20s when they were referred to the clinic. These cases indicate a wide spectrum of the relationship between dental anxiety and oral health status

Observational studies
In general, epidemiological studies reveal an obvious relationship between oral status and dental anxiety. Individuals with dental anxiety have more oral diseases than non-dentally anxious persons. In addition, studies also point towards a gradient in health inasmuch as the higher the dental anxiety levels the more negatively affected the oral health (Hällström and Halling 1984; Hägglin et al. 1996; Ng and Leung 2008). The differences/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


