Rationale for Dental Implants*
Carl E. Misch
The goal of modern dentistry is to restore the patient to normal contour, function, comfort, esthetics, speech, and health, whether restoring a single tooth with caries or replacing several teeth. What makes implant dentistry unique is the ability to achieve this goal regardless of the atrophy, disease, or injury of the stomatognathic system.1 However, the more teeth a patient is missing, the more challenging this task becomes. As a result of continued research, diagnostic tools, treatment planning, implant designs, materials, and techniques, predictable success is now a reality for the rehabilitation of many challenging clinical situations.
The number of dental implants used in the United States increased more than 10-fold from 1983 to 2002, and that number increased another 10-fold from 2000 to 2010. More than 5 million dental implants are inserted each year in the United States. This number continues to increase steadily, with an expected yearly growth sustained at 12% to 15% for the next several years.2 More than $1 billion in implant products was sold in the United States in 2010, up from $550 million of implant products sold in 2005 and compared with $10 million in 1983. When bone grafting materials are included in implant products, it is estimated the field of implant dentistry in 2010 sold $10 billion in products to provide services to patients.3 More than 90% of interfacing surgical specialty dentists currently provide dental implant treatment on a routine basis in their practices, 90% of prosthodontists restore implants routinely, and more than 80% of general dentists have used implants to support fixed and removable prostheses compared with fewer than 50% of specialists and fewer than 25% of general dentists 20 years ago.4–8
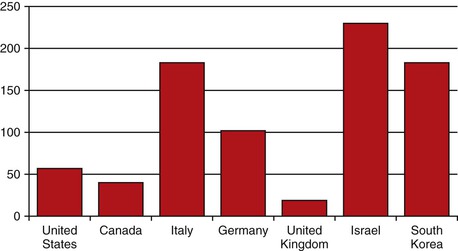
Despite these figures demonstrating implants are incorporated into dentistry more than ever before, there is still much room for continued growth. Utilization of dental implants varies widely in different countries of the world. For example, it is estimated that the number of implants each year per 10,000 people is 230 for Israel (the greatest number); 180 for South Korea and Italy; 140 for Spain and Switzerland; 100 for Germany; and 60 each for Brazil, the Netherlands, and the United States (Figure 1-1). Japan and France (50), Canada and Australia (40), and Taiwan and United Kingdom at 20 per year use implants less often. The six countries with greatest use of implants (Europe and South Korea) accounted for more than half the total market growth from 2002 to 2007. A long-term growth of 12% to 15% is expected in the future in most countries using implants at this time.
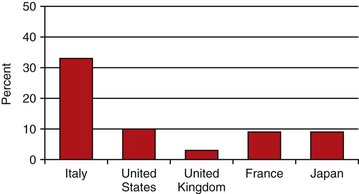
The percentage of teeth replaced with an implant, rather than traditional fixed or removable prostheses, also dramatically varies by country. In Israel, Italy, and South Korea, 30% to 40% of teeth replaced incorporate an implant. In Spain, Switzerland, Germany, and Sweden, 20% to 26% of restorations to replace teeth are supported by an implant. Brazil and Belgium come in at 13% to 16% of restorations use and implant. Surprisingly, the United States, Japan, France, and Canada use implants in 10% or fewer of the teeth replaced.8 In other words, in a 2011 report, only one of 10 teeth replaced in the United States uses an implant for an abutment (Figure 1-2).
The increased need and use of implant-related treatments in the future result from the combined effect of several factors, including (1) aging population living longer, (2) tooth loss related to age, (3) consequences of fixed prosthesis failure, (4) anatomical consequences of edentulism, (5) poor performance of removable prostheses, (6) consequences of removable partial dentures, (7) psychological aspects of tooth loss and needs and desires of aging baby boomers, (8) predictable long-term results of implant-supported prostheses, (9) advantages of implant-supported restorations, and (10) increased public awareness.
Effects of an Aging Population
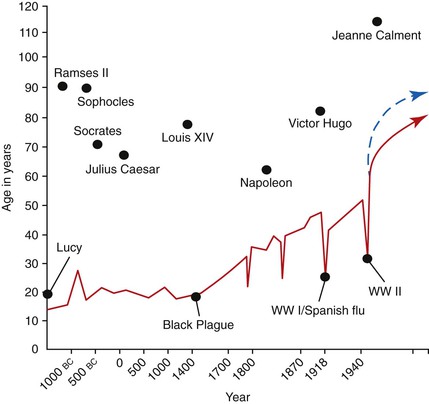
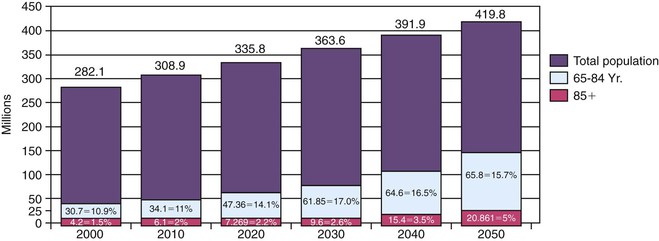
According to the literature, age is directly related to every indicator of tooth loss.9,10 Therefore, the aging population is an important factor to consider in implant dentistry. Although some famous individuals in the past have lived past the age of 80 years (e.g., Ramses II, King Louis XIV), the average life span remained below 40 years until the 18th century. For example, when Alexander the Great conquered the ancient world, he was only 17 years old. However, life expectancy at that time was only 22 years of age. From 1000 BC to 1800 ad, life span remained less than 30 years (Figure 1-3). Since 1960, the increase in life expectancy has been more rapid than at any other time in history (Figure 1-4). In 1980, 30% of the U.S. population was older than age 45 years, 21% was older than 50 years, and 11% was older than 65 years. In 1995, 15 years later, these individuals were older than age 60 years. The group older than age 65 years is projected to increase from 12% in 2000 to more than 20% of the population within the next 15 years11 (Figure 1-5).
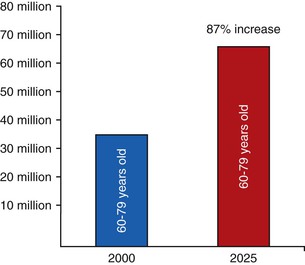
In addition, not only is the percentage of the population over 65 years of age increasing, but the overall population is also increasing. The population in 2000 was 282 million and is projected to increase 49% to 420 million by 2050. Considering the effect of both a population increase and a greater percentage of that population being older than age 65 years, a dramatic overall increase in geriatric patient numbers can be expected. In 2003, 35 million people were older than age 65 years. This number is expected to increase 87% by 2025, resulting in almost 70 million people being older than age 65 years in the United States12 (Figure 1-6). Because older people are more likely to be missing teeth, the need for implant dentistry will dramatically increase over the next several decades.
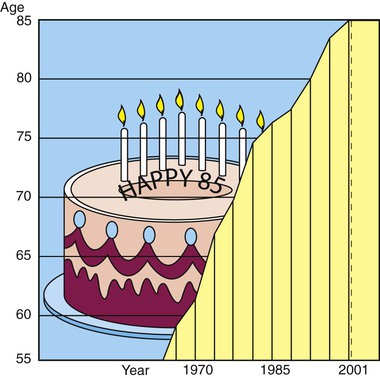
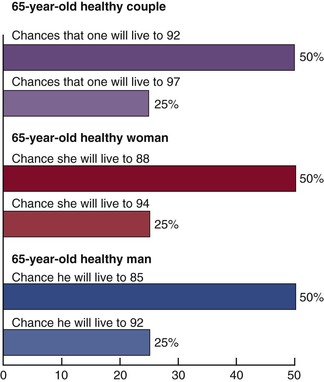
Life expectancy has increased significantly past the age of retirement. In 1965, the average life span was 65 years; in 1990, it was 78 years. Life expectancy in 2001 was 85 years for a nonsmoking individual of normal weight.13 A 65-year-old woman can now expect to live 25 more years 40% of the time and 30 more years 19% of the time14–16 (Figure 1-7). Women represent two thirds of the population older than age 65 years and are more likely to use implants to replace their teeth compared with men.17 It is not unusual for a 70-year-old patient to ask, “Is it worth it for me to spend more than $30,000 to repair my mouth at my age?” The response should be very positive because the patient’s life expectancy may extend for two more decades, and his or her current oral situation will normally become worse if not corrected.
Social pleasures, including dining and dating, continue throughout advanced life. In the past, geriatric dentistry meant inexpensive treatment emphasizing nonsurgical approaches. The poverty rate for elderly adults, however, is less than 10%, and retiree median income has grown 8% in recent years. The median net worth of retirees is 15 times the net worth of those younger than age 35 years and three times as high as “working families” ages 35 to 44 years.17,18 Close to 20% of today’s retirees have a net worth of more than a quarter of a million dollars.
Today, the full scope of dental services for elderly patients is increasing in importance to both the public and the profession because of the increasing age of our society. Treatment alternatives that consider fixed prostheses with implant support should be presented to almost any patient. Only when all treatment options are discussed can a person’s desires related to the benefit of implant dentistry be truly appreciated.
Dental services for elderly patients clearly represent a growing demand for the dental profession. In 2000, 28.8% of all income from a dentist came from patients age 60 years and older—a group that represented only 12% of income in 1988. When the dentist is older than age 40 years, income from those older patients represents 64.3% of the dentist’s income; in 1988, it was 30.3%.19 Clearly, the demographics of our population have dramatically changed the economics of dental practice.
Age-Related Tooth Loss
Single-Tooth Edentulism (Single-Tooth Loss)
Adult patients often have one or more crowns as a consequence of previous larger restorations required to repair the integrity of the tooth. Longevity reports of crowns have yielded very disparate results. The mean life span at failure has been reported as 10.3 years. Other reports range from a 3% failure rate at 23 years to a 20% failure rate at 3 years. It has been estimated that a $425 crown for a 22-year-old patient will cost $12,000 during the patient’s lifetime to replace or repair.20
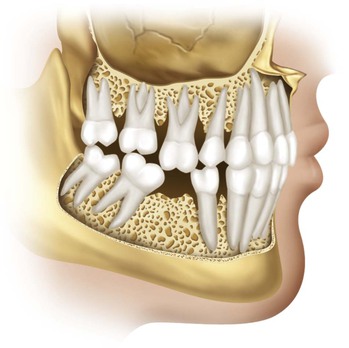
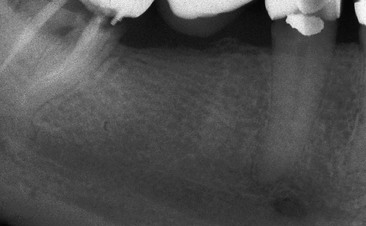
The primary cause of failure of the crown is caries followed by endodontic therapy.21–29 The tooth is at risk for extraction as a result of these complications, which are the leading causes of single posterior tooth loss in adults (Figure 1-8).
As a consequence, the posterior regions of the mouth often require the replacement of a single tooth.30–32 The first molars are the first permanent teeth to erupt in the mouth and, unfortunately, are often the first teeth lost as a result of decay, failed endodontic therapy, or fracture (usually after endodontics). They are important teeth for maintenance of the arch form and proper occlusal schemes (Figure 1-9).
Fixed Partial Dentures (Dental Bridges)
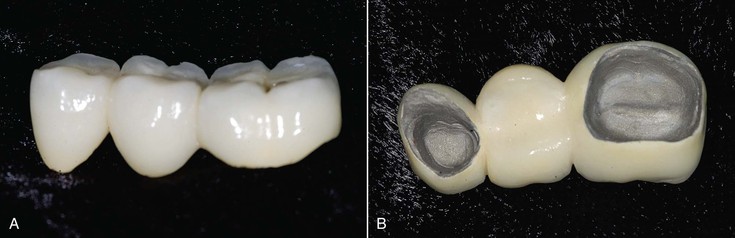
The most common choice to replace posterior missing teeth is a fixed partial denture (FPD). The adjacent teeth next to the missing tooth are prepared, and crowns are inserted that are connected to the missing tooth (pontic) (Figure 1-10). This three-tooth restoration can be fabricated within 1 to 2 weeks and satisfies the criteria of normal contour, comfort, function, esthetics, speech, and health. Because of these benefits, FPD has been the treatment of choice for the past 6 decades. Bone and soft tissue considerations in the missing tooth site in the posterior regions are few. Every dentist is familiar with the procedure, and it is widely accepted by the profession, patients, and dental insurance companies.
Almost 30% of the 50- to 59-year-old adults examined in a U.S. National Survey exhibited either single or multiple edentulous spaces bordered by natural teeth. In 1990, more than 4 million FPDs were placed in the United States.21,22,32 Treatments to replace single teeth with a fixed prosthesis represent 7% of the annual dental reimbursement from insurance companies and more than $3 billion each year. Less than half of our population in the United States has dental insurance, and of those who do, only 50% of treatment costs are reimbursed. Hence, the entire three-unit FPD costs in the United States may approach more than $10 billion each year.
A three-unit FPD presents survival limitations to the restoration and, more importantly, to the abutment teeth.27,29 The survival rate of a FPD is lower than for a single crown restoration. In an evaluation of 42 reports since 1970, Creugers et al. calculated a 74% survival rate for FPDs for 15 years.25 Mean life spans of 9.6 to 10.3 years have been reported by Walton et al.27 and Schwartz et al.,21 respectively. However, reports are very inconsistent, with as little as 3% loss over 23 years to 20% loss over 3 years.21–29,32
The incidence of failure is greater for a FPD compared with a single crown and places the abutment teeth at more risk. Caries (decay) and endodontic (root canal) failure of the abutment teeth are the most common causes of prostheses failure.27,28 Whereas the caries risk for a crown at 5 years is 1%, the caries risk for a FPD is over 20%. The pontic acts as a plaque reservoir in a FPD and the abutment teeth often decay (Figure 1-11). As a result of structural failure from decay or failed endodontic therapy, the abutment teeth are at increased risk of loss. Up to 15% of abutment teeth for a FPD require endodontic therapy compared with 3% of nonabutment teeth that have crown preparations25 (Box 1-1). In addition, the prepared and crowned abutments may be sensitive to cold from hyperemia related to the trauma of a tooth preparation.
Unfavorable outcomes of FPD failure include both the need to replace the failed prosthesis and the loss of an abutment and the need for additional pontics (replacement teeth) and abutment teeth in the replacement bridge. Approximately 8% to 12% of the abutment teeth holding a FPD are lost within 10 years.8 The abutment teeth of a FPD may be lost at rates as high as 30% within 14 years.26 The most common reason for single-tooth loss is endodontic failure or fracture of a tooth (usually after endodontic therapy). Because 15% of abutment teeth require endodontics and root canal therapy may have a 10% failure rate at the 8-year mark, abutment teeth are at increased risk of loss.
Almost 80% of abutments prepared for a three-unit FPD have no existing or only minimal restorations33,34 (Figure 1-12). Rather than removing sound tooth structure and crowning two or more teeth—thus increasing the risk of decay and endodontic therapy (and splinting teeth together with pontics, which have the potential to cause additional tooth loss)—a dental implant may replace the single tooth (Box 1-2).
Single-Tooth Implants
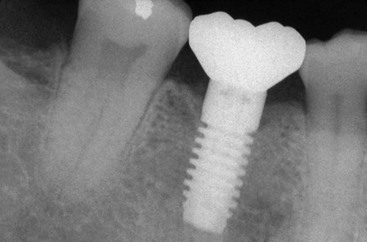
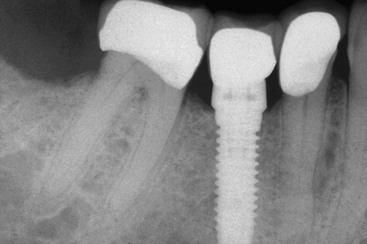
A primary treatment option to replace a posterior single missing tooth is a single-tooth implant (Figure 1-13). For years, patients were advised to put their desires aside and accept the limitations of a FPD. However, many believe the most natural method to replace a tooth is to use an implant rather than preparing adjacent teeth and joining them together with a prosthesis. The primary reasons for suggesting the FPD were its clinical ease, reduced cost, and reduced treatment time. However, if this concept were expanded, extractions would replace endodontics, and removable partial dentures would be used instead of fixed prostheses. The primary reason to suggest or perform a treatment should not be related to treatment time, costs, or difficulty of the procedure but instead should consider the best possible long-term solution for each individual.

From 1993 to the present, single-tooth implant survival reports have validated this procedure as the most predictable method of tooth replacement. There are more refereed reports in the literature for single-tooth implant replacement than for any other method of tooth replacement,35 and all reports demonstrate a higher survival rate for single-tooth implants. In 1995, Haas et al. reported on 76 single-tooth implants over a 6-year period and found a 97% survival rate and a 2.6% implant loss.36 Fugazzotto evaluated 1472 implants over a 13-year period and found a 97% survival rate during that period.37 In 2008, Misch et al. reported on more than 1300 implants over a 10-year period and found over a 99% survival rate.34 As important, the adjacent teeth survival and restoration rate was greater than with any other treatment method to replace a tooth (Figure 1-14).
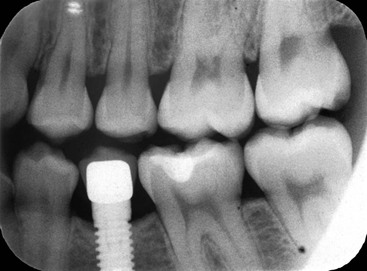
Goodacre et al. performed a Medline literature review from 1980 to 2001 and found the single-tooth implant success rate to be in the range of 97%—higher than any other implant restoration.35 In comparison, FPD failure rates may be as high as 20% within 3 years, and 50% rates at 10 to 15 years are expected. As a result, the single-tooth implant exhibits the highest survival rates presented for single-tooth replacement. As important, reports indicate less restoration or loss of an adjacent tooth, which is a considerable advantage33,34 (Figures 1-15 and 1-16). Despite some limitations and obvious clinical challenges, the single-tooth implant represents the treatment of choice from both a health and value standpoint.38

When adjacent teeth are healthy or when the patient refuses their preparation for the fabrication of a traditional three-unit fixed partial restoration, a posterior single-tooth implant is an excellent solution. Health-related advantages of this modality over a fixed partial restoration are listed in Box 1-3 and include a decreased risk of decay and periodontal disease, decreased risk of abutment tooth loss from endodontic failure or caries, and improved esthetics (because the adjacent teeth may remain unrestored). In fact, even when the adjacent teeth require crowns, a single-tooth implant is often the treatment of choice because a crown decays less often than abutments for a FPD (Figure 1-17). Psychological advantages, especially with congenitally missing teeth or the loss of a tooth after a crown restoration, are significant as well. These advantages are so significant to the health and periodontal condition of the adjacent teeth and maintenance of the arch form that the single-tooth implant has become the treatment of choice in most situations.
Economic considerations may play in disfavor of the implant restoration only during the first several years. Compared with a FPD, a single-tooth implant becomes more advantageous economically, not only for health considerations but also financially after the break-even point of 7 years, at which time the patient will not need a replacement prosthesis. As a result, the future savings will offset the initial higher cost, especially because the adjacent teeth are more likely to survive longer and replacement of a restoration is unnecessary.39,40
Partial Edentulism (Tooth Loss)
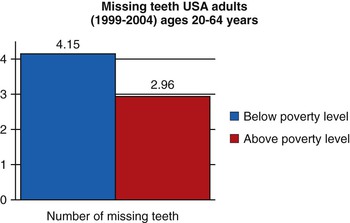
The prevalence of partial edentulism is also of interest because a growing number of implants are used in these patients. A 1988 to 1991 survey in the United States found that only 30% of patients had all 28 teeth. Partially dentate patients had an average of 23.5 teeth.9,32,41 In the 1999 to 2004 follow-up survey, the average number of missing teeth was fewer than two of 28 teeth for the 20- to 39-year-old group. However, this number rapidly increased to an average of nine teeth missing in adults older than age 60 years.42 The average missing teeth in the population below the poverty level was four teeth compared with three missing teeth above the poverty level (Figure 1-18). Hence, income was not a major factor for the number of teeth loss. Partially edentulous seniors older than age 60 years have lost an average of 10 teeth, with older seniors having lost three more teeth than the younger seniors. Statistics for partial edentulism are similar for both men and women.
The greatest transition from an intact dental arch to a partially edentulous condition in the 1987 study occurred in the 35- to 54-year-old group.19,32 The growth rate of this portion of the population was approximately 30% in 1982 and is continuing to increase, more than any other age group. For example, in 1982, this 35- to 54-year-old group increased from 39 million Americans to 79 million in 2005. Although the number of teeth missing per patient may seem to decrease, the overall number of missing teeth will continue to increase as a result of the aging population. Therefore, the need for implant services in partially edentulous patients will dramatically increase during the next several decades.14
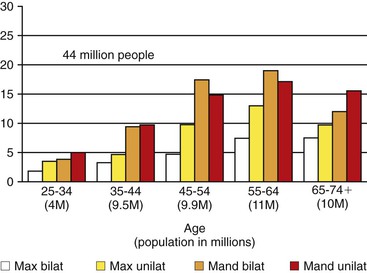
The most common missing teeth are molars.31 Partial free-end edentulism is of particular concern because in these patients, teeth are often replaced with removable partial prostheses. This condition is rarely found in persons younger than age 25 years. Mandibular free-end edentulism is greater than its maxillary counterpart in all age groups. Unilateral free-end edentulism is more common than bilateral edentulism in both maxillary and mandibular arches in the younger age groups (ages 25 to 44 years). About 13.5 million persons in these younger age groups have free-end edentulism in either arch (Figure 1-19).
In 45- to 54-year-old patients, 31.3% have mandibular free-end edentulism, and 13.6% have free-end edentulism in the maxillary arch. Approximately 9.9 million persons in the 45- to 54-year-old group have at least one free-end edentulous quadrant, and almost half of these have bilateral partial edentulism.10 The pattern of posterior edentulism evolves in the 55- to 64-year-old group, in whom 35% of mandibular arches show free-end edentulism compared with 18% of maxillary arches. As a result, approximately 11 million individuals in this age group are potential candidates for implants. An additional 10 million show partial free-end edentulism at age 65 or older.
Additional studies have documented that in the population of noninstitutionalized U.S. civilians, one of five had a removable prosthesis of some type.43–45 The total number of potential patients in the U.S. survey with at least one quadrant of posterior missing teeth is more than 44 million people.10 If each of these arches requires three implants to support a fixed prosthesis, 132 million implants would be required.
Removable Partial Dentures
Removable soft tissue–borne partial dentures have one of the lowest patient acceptance rates in dentistry. Half of patients with a removable partial denture chew better without the device. A 44-year Scandinavian study revealed that only 80% of patients were wearing such prostheses after 1 year. The number further decreased to only 60% of the free-end partial dentures worn by the patients after 4 years. This rate was reduced to only 35% at 10 years.46–50 In another study, few partial dentures survived more than 6 years.51 Although one of five U.S. adults have worn a removable dental prosthesis of some type, 60% reported at least one problem with it.44
Reports of removable partial dentures indicate the health of the remaining dentition and surrounding oral tissues often deteriorates.46,52 In a study that evaluated the need for repair of an abutment tooth as the indicator of failure, the “success” rates of conventional removable partial dentures were 40% at 5 years and 20% at 10 years.48 Patients wearing the partial dentures often exhibit greater mobility of the abutment teeth, greater plaque retention, increased bleeding upon probing, higher incidence of caries, speech inhibition, taste inhibition, and noncompliance of use.49–52 A report by Shugars et al. found abutment tooth loss for a removable partial denture may be as high as 23% within 5 years and 38% within 8 years.26 Aquilino et al. reported a 44% abutment tooth loss within 10 years for a removable partial denture53 (Box 1-4).
The natural abutment teeth, on which direct and indirect retainers are designed, must submit to additional lateral forces. Because these teeth are often compromised by deficient periodontal support, many partial dentures are designed to minimize the forces applied to them. The result is an increase in mobility of the removable prosthesis and greater soft tissue support. These conditions protect the remaining teeth but accelerate the bone loss in the edentulous regions.54 It should be noted that bone loss is accelerated in the soft tissue support regions in patients wearing the removable device compared with the case in patients not wearing the device (Figure 1-20). Therefore, alternative therapies that improve oral conditions and maintain bone are often warranted.
Total Edentulism
Complete edentulism is not an eventual, healthy occurrence in an adult population. Rather, it is most often the result of repeated tooth extractions from the combined pathologic processes of dental caries, periodontal disease, or a method to reduce the costs associated with dental treatment.55–57 Similar to other pathologic outcomes of disease, the occurrence of total loss of teeth is directly related to the age of the patient. The rate of edentulism increases by 4% per 10 years in early adult years and increases to more than 10% per decade after age 70 years.57
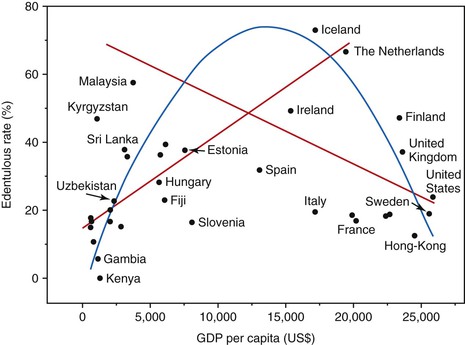
The average total edentulous rate around the world is 20% of the adult population at age 60 years, although there is wide disparity from the countries with the highest and lowest rates.57 For example, from the 65- to 74-year-age group, the total edentulous rate in Kenya and Nigeria was 4%, but the Netherlands and Iceland have a 65.4% and 71.5% rate, respectively. The edentulous Canadian rate was 47% at 65 to age 69 years and 58% from ages 70 to 98 years (with Quebec at 67% for those older than age 65 years compared with Ontario with a 41% rate).
One of the factors influencing total edentulism is the level of education. In data from the Canadian Health Promotion Survey from 1990, whereas the least educated population had an edentulous rate of 50%, those with a college education had a low 4% rate.58 The United States showed a similar pattern in the period 1988 to 1994, with an edentulous rate of 22% for those with less than 8 years of education, 12% for those with 9 to 11 years of school, 8% for those with 12 years of school, and 5% for individuals with more than 12 years of education.41
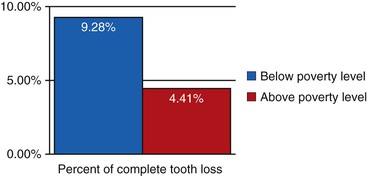
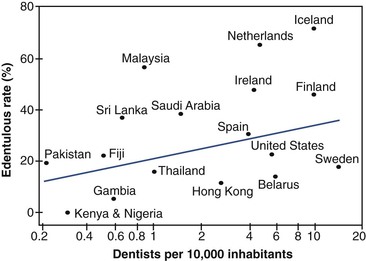
Although income is often related to education, it plays less of a role in the rate of edentulism. The complete tooth loss in the U.S. adult below the poverty level from 1999 to 2004 was 9.28% and 4.41% above the poverty level, only a 5% difference (Figure 1-21). Countries with higher income levels do not necessarily have less tooth loss. For example, whereas Iceland and the Netherlands have the greatest complete tooth loss by age 70 years with a gross domestic product (GDP) of $17,000, Kenya and Gambia have one of the least complete edentulusm rate with a GDP of less than $2500 (Figure 1-22). An interesting note is that an increasing number of dentists in a country (per 10,000 inhabitants) does not reduce the complete edentulous rate. In fact, countries with the most dentists often have a higher complete edentulous rate (Figure 1-23).
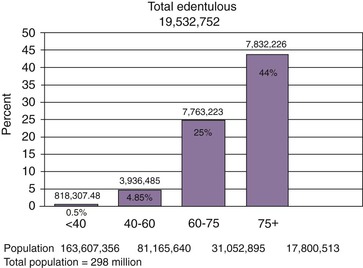
A 1999 to 2002 survey found that total edentulism in the United States of both arches occurred in 7.7% of the adult population in the United States, or almost 20 million people.41 The present younger population is benefiting from today’s advanced knowledge and restorative techniques. Total edentulism has been noted in 5% of employed adults ages 40 to 44 years, gradually increasing to 26% at age 65 years and almost 44% in seniors older than age 75 years9 (Figure 1-24). As expected, older persons are more likely to be missing all their teeth. Gender was not found to be associated with tooth retention or tooth loss after adjustments were made for age.
The maxillary (upper) arch may be completely edentulous, opposing at least some teeth in the mandible (lower jaw). This condition occurs 35 times more often than the reverse situation. At age 45 years, 11% of the population has maxillary total edentulism opposing teeth, which increases to 15% by 55 years of age and then remains relatively constant.45 Therefore, a total of approximately 12 million individuals in the United States have total edentulism in one arch, representing 7% of the adult population overall.
The percentages of one or two arch total edentulism translate into more than 30 million people or about 17% of the entire U.S. adult population.45 To put these numbers in perspective, 30 million people represent approximately the entire U.S. African American population, the U.S. Hispanic population, the whole population of Canada, or the total population in the United States older than 65 years of age.
Although the edentulism rate is decreasing every decade, the elderly population is rising so rapidly that the adult population in need of one or two complete dentures will actually increase from 33.6 million adults in 1991 to 37.9 million adults in 2020. The total numbers of edentulous arches are estimated at 56.5 million in 2000, 59.3 million in 2010, and 61 million in 2020.59 Complete edentulism, therefore, remains a significant concern, and affected patients often require implant dentistry to solve several related problems. If four implants were used to help support each complete edentulous arch, a total of 226 million implants would be required. Yet only 10 million implants were inserted in 2010 for all patient treatment. Almost 70% of dentists spend less than 1% to 5% of their treatment time on edentulous patients, leaving a great unfulfilled need for implant dentistry.
When the posterior partially edentulous figures are added to the complete edentulous percentages, more than 30% of the adult U.S. population are candidates for a complete or partial removable prosthesis. The need for additional retention, support, and stability and the desire to eliminate a removable prosthesis are common indications for dental implants. As/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses