Figure 3.25 Pain location as reported by the patient.
C. Medical History
- No other health issues.
D. Psychosocial History
- Patient studied physical therapy years ago but was never active in this profession.
- She and her husband lived abroad for years and returned to the home country 1 year ago (when the pain complaints started).
- Her daily activities are housekeeping, spending time with her family and working with the computer.
- Patient specific complaint: pain is interfering in her daily life: 55 (VAS 0–100).
- Patient reports moderate stress, especially since the move (PSS-10).
- Moderate pain-related disability (Grade II; GCPS).
- Mild anxiety (GAD-7).
- Mild depression (PHQ-9).
- Parafunctions: lip-biting (OBCL).
- Bruxism: not aware of clenching or grinding (OBCL).
E. Previous Consultations and Treatments
- None.
F. Extraoral Status
- No asymmetries.
- Jaw movement capacity: normal mandibular movements, no pain on movement.
- TMJ: no palpation pain, no noises.
- Palpation: familiar pain with palpation of the right masseter and temporalis muscles; for the temporal muscle the pain was familiar to the headache.
- Dynamic: static provocation tests of the jaw. All static tests (opening, closing and protrusion) gave familiar pain from the right masseter muscle, while the dynamic tests gave familiar pain from both masseter and temporalis muscles on the right side.
G. Intraoral Status
- Tooth indentations in the cheek and lips, tongue scalloping.
- Full dentition except wisdom teeth.
- Stable occlusion.
H. Additional Examinations and Findings
- Neck movement: limited range of motion on rotation with radiating pain to the right ear and jaw.
- Palpation of the right sternocleidomastoid and trapezius muscles gave familiar pain.
- The static provocation tests of the neck flexion, rotation to the left, lateroflexion to the left, were positive and provoked jaw pain on the right side.
- The dynamic neck tests were negative.
I. Diagnosis/Diagnoses
DC/TMD
- Myalgia in masticatory muscles.
- Headache attributed to TMD.
ICHD-3 beta
- Headache attributed to cervical myofascial pain.
Other
- Cervical spinal pain, myalgia spreading to orofacial region.
J. Case Assessment
- Clenching (suspicion based on the intraoral examination) and psychosocial aspects (stress) in combination with tightening shoulders, especially while working at the computer, are likely background factors to the masticatory muscle and neck pain and headache.
- The onset of pain complaints was at the same time as moving to the home country.
- Returning to live in the home country as well as concerns about children and grandchildren that adds to her total stress level seem to play a role in experiencing increased muscle tension, as well as concerns about the pain complaint itself. This could be considered a risk factor, as her concerns might influence a good outcome negatively.
K. Evidence-based Treatment including Aims
- The main aim of the treatment plan is to substantially reduce the interference by the jaw and neck pain on her daily life.
- The physical therapy is focused on offering tools such as counselling, exercises and insight in the complaints to the patient so that she can manage her pain in such a way that it does not interfere with her daily life.
- As the patient reports that her pain mainly increases during the day, the first choice of treatment is physical therapy (a splint is mainly indicated for night-time bruxism and is therefore less likely to be beneficial in this case).
- If necessary, re-evaluate after 4 months for more extensive treatment with splint and behavioural therapy.
L. Prognosis and Discussion
- The prognosis for physiotherapy as described in this case is good since physiotherapy can provide a coordinated therapy for neck and jaw pain.
Background Information
- TMD patients four times more often show neck pain than persons without TMD.
- Patients with both TMD and neck pain report higher psychological and stress scores than patients with only TMD pain. (Visscher et al., 2001).
Diagnostic Criteria
ICHD-3 beta criteria for Headache attributed to cervical myofascial pain (Headache Classification Committee of the International Headache Society (IHS), 2013). Sensitivity and specificity have not been established.
- A. Head and/or neck pain fulfilling criterion C.
- B. A source of myofascial pain in the muscles of the neck, including reproducible trigger points, has been demonstrated.
- C. Evidence of causation demonstrated by at least two of the following:
- 1. Either or both of the following: (a) pain has developed in temporal relation to onset of the cervical myofascial pain disorder; (b) pain has significantly improved in parallel with improvement in the cervical myofascial pain disorder.
- 2. Significant pressure-tenderness is elicited in cervical muscles corresponding to the pain perceived by the patient.
- 3. Pain is temporarily abolished by local anaesthetic injections into trigger points, or by trigger-point massage.
- D. Not better accounted for by any other ICDH-3 diagnosis.
DC/TMD criteria for Myalgia, see Case 3.3, for Headache attributed to TMD, see Case 4.1 (Schiffman et al., 2014).
Fundamental Points
- Literature suggest that for patients with persisting pain the treatment should focus on coping with the pain. This case study presents a practical approach to guide such patients.
- A good therapeutic relationship is a prerequisite to gain information about the (chronic) pain experience in order to set an adequate treatment.
- A patient with chronic TMD and neck pain serves as an example on providing guidance on how to stimulate a patient in changing the way of coping with pain in their life.
- Three perspectives on the functioning of the clinician in this are: medical focus, focus on pain education and a focus on combined expertise.
- These three perspectives are all valuable with subtle but considerable differences on the relation between the patient and clinician and, in the long run, on compliance and treatment outcome (Table 3.2).
- Dynamic/static tests imitate joint and muscle function. During dynamic tests, the joint structures are tested for pain on articulation and the muscles are slightly loaded. During static tests the muscles are tested for pain on isometric contraction (Figure 3.26; Visscher et al., 2000).
- Positive findings on static tests point in the direction of myalgia.
- Positive findings on dynamic test point in the direction of arthralgia.
Table 3.2 Aligning the relation between clinician and health-care provider that is not influenced by a biomedical focus can bring balance in the relation between the patient and the clinician
| Perspective | Clinician expertise | Patient expertise |
| Medical focus | ++ | − |
| Focus on pain education | ++ | + |
| Focus on combined expertise | ++ | ++ |
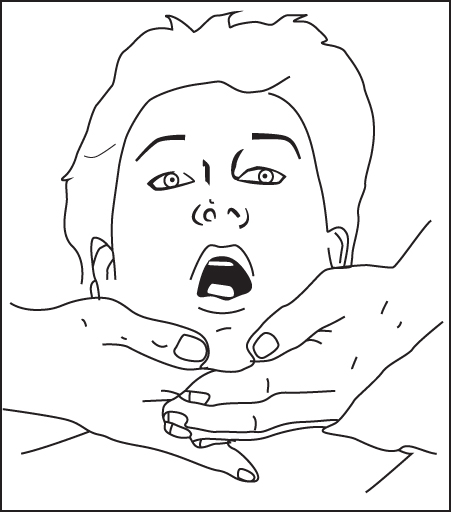
Figure 3.26 An example of the dynamic opening test for the masticatory system.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


