Approaches to the Maxilla
The maxilla can be approached through a variety of incisions, but most of it can be exposed with an incision hidden within the oral cavity. The maxillary vestibular approach is one of the most useful when performing any of a wide variety of procedures in the midface. It allows relatively safe access to the entire facial surface of the midfacial skeleton, from the zygomatic arch to the infraorbital rim and the frontal process of the maxilla. The greatest advantage of the approach is the hidden intraoral scar that results. The approach is also relatively rapid and simple, and the complications are few. Damage to branches of the facial nerve is nonexistent as long as one stays within the subperiosteal plane, and damage to the infraorbital nerve is rare with proper use of the technique.
When additional exposure is required, the maxillary vestibular approach can be combined with other approaches to broaden the access. Two such approaches, the facial degloving and the Weber-Ferguson, will be described later.
SURGICAL ANATOMY
Infraorbital Nerve
The only important neurovascular structure that must be negotiated during procedures in the midfacial region is the infraorbital neurovascular bundle. The infraorbital nerve is the largest cutaneous branch of the maxillary division of the trigeminal nerve. The artery and vein that accompany the infraorbital nerve are surgically insignificant. The nerve exits the infraorbital foramen, 7 to 10 mm inferior to the infraorbital rim just medial to the zygomaticomaxillary suture, or approximately at the medial and middle thirds of the orbit. After exiting the infraorbital foramen, the infraorbital nerve divides into terminal branches that spread fanlike into the lower eyelid, nose, and upper lip. The palpebral branches turn upward to supply the lower eyelid; the nasal branches supply the skin on the lateral surface of the lower half of the nose. Three of the four superior labial branches enter the lip between its muscles and the mucous membrane. These nerves supply not only the mucous membrane of the upper lip, but also its skin, which they reach by perforating the orbicularis oris muscle. Damage to this nerve results in loss of sensation in these areas, and possibly dysesthesia.
Nasolabial Musculature
The attachments of the facial muscles of the nasolabial region may be disrupted during the maxillary vestibular approach. Therefore, these muscles should be properly repositioned during closure to avoid undesirable esthetic changes to the face. The muscles of importance are the nasalis group, the levator labii superioris alaeque nasi, the levator labii superioris, the levator anguli oris, and the orbicularis oris (see Fig. 7.1).
The nasalis group has transverse nasal and alar parts. It originates along the midline of the nasal dorsum and spreads laterally over the external aspect of the upper lateral cartilages where it intermingles with fibers of the levator labii superioris alaeque nasi and the levator labii superioris. Part of the transverse nasalis inserts into the skin at the nasolabial groove, where it intermingles with fibers from the levator labii superioris alaeque nasi and oblique fibers of the orbicularis oris, forming a lateral nasal modiolus. Another portion of the transverse nasalis inserts onto the incisal crest and anterior nasal spine and is in deep contact with the depressor septi muscle. The alar portion is ultimately reflected inward, forming the anterior floor of the nose.
Several muscle groups elevate the upper lip. The levator labii superioris alaeque nasi rises from the frontal process of the maxilla alongside the nose and passes obliquely in two segments. One segment inserts onto the lateral crus of the alar cartilage and skin of the nose, and the other deeper segment extends to the nasal vestibule, blending with fibers of the nasalis muscle, depressor septi, and oblique bands of the orbicularis oris. The levator labii superioris arises from the infraorbital margin of the maxilla beneath the orbicularis oculi. It extends downward and medially, superficial to and intermingling with the orbicularis oris, beneath the skin of the ipsilateral lower philtral columns and the upper lip. The levator
anguli oris muscle lies deep to the levator labii superioris and the zygomaticus muscles. It arises from the canine fossa of the maxilla and courses downward and medially to the commissure, where it intermingles with the fibers of the orbicularis oris muscle.
anguli oris muscle lies deep to the levator labii superioris and the zygomaticus muscles. It arises from the canine fossa of the maxilla and courses downward and medially to the commissure, where it intermingles with the fibers of the orbicularis oris muscle.

Figure 7.2 Effects of the maxillary vestibular approach if simple closure is performed: the nasal tip loses projection, the alar bases widen, and the upper lip rolls inward.
|
The orbicularis oris muscle consists of three distinct strata. Horizontal fibers extend from one commissure to the other, passing beneath the philtrum. Oblique bands extend from the commissures to the anteroinferior aspect of the nasal septal cartilage, anterior nasal spine, and floor of the nose. The incisal bands extend from the commissures deeply to insert onto the incisive fossa of the maxilla. All these muscles and their investing fascia together contribute significantly to the position and configuration of the lateral nasal and labial regions.
The maxillary vestibular incision and the subperiosteal dissection attendant to this approach cut some of the muscular origins and strip the origins and insertions of most muscles from the bone (Fig. 7.1), causing superolateral retraction of the tissues by the action of the zygomaticus muscles and the natural tendency for muscles to reattach in a shortened position. Lateral displacement of the nasal modiolus causes widening of the alar base with flaring of the alae from unopposed action of the dilator naris. This displacement causes deepening of the alar groove and splaying of the alar bases, nostrils, and nasal tip (see Fig. 7.2). Loss of soft tissue fullness in the nasolabial region results in changes that are similar to those seen in the aging face: thinning and retraction of the upper lip, reduced vermillion exposure, and a more obtuse nasolabial angle. Down-turning of the corner of the mouth may occur when the levators of the upper lip are detached from their origin because the depressors of the mouth will then be unopposed.
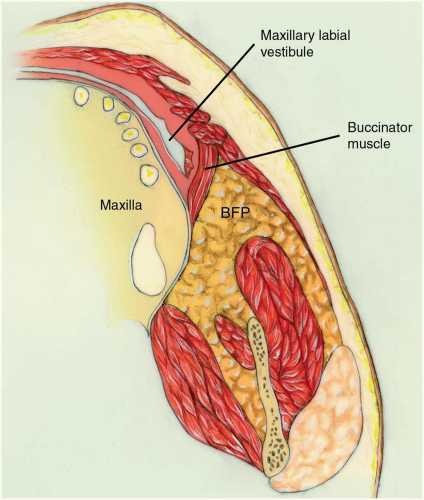
Buccal Fat Pad
The buccal fat pad consists of a main body and four extensions: buccal, pterygoid, superficial, and deep temporal. The body is centrally positioned. The buccal extension lies superficially within the cheek, and the pterygoid and temporal extensions are situated more deeply.
The main body of the fat pad is located above the parotid duct and extends along the upper portion of the anterior border of the masseter. It then courses medially to rest on the periosteum of the posterior maxilla (see Fig. 7.3). In this region, the body of the fat pad overlies the uppermost fibers of the buccinator muscle and travels forward along the vestibule overlying the maxillary second molar. Posteriorly, it wraps around the maxilla and travels through the pterygomaxillary fissure, where it is in intimate contact with branches of the internal maxillary artery and the maxillary division of the trigeminal nerve.
MAXILLARY VESTIBULAR APPROACH
The facial surface of the midface can be exposed using the maxillary vestibular approach. The length of incision and extent of subperiosteal dissection depend on the area of surgical interest and the extent of the surgical intervention. If the area of interest involves only one half of the midface, for instance, with a unilateral zygomaticomaxillary fracture, the incision can be made on one side only, leaving the other side intact.
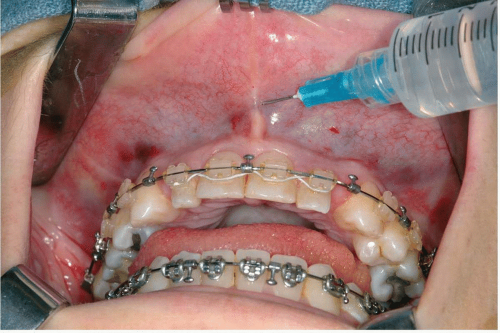
Figure 7.4 Photograph showing injection of local anesthesia with a vasoconstrictor into the submucosa.
|
TECHNIQUE
▶ Step 1. Injection of Vasoconstrictor
The oral mucosa, submucosa, and facial muscles are lushly vascularized. Submucosal injection of a vasoconstrictor can dramatically reduce the amount of hemorrhage during incision and dissection (see Fig. 7.4).
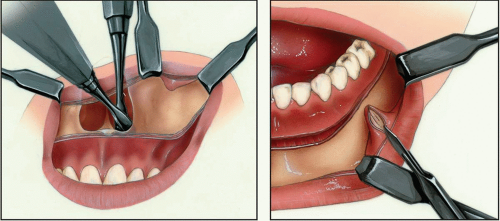
▶ Step 2. Incision
The incision is usually placed approximately 3 to 5 mm superior to the mucogingival junction (see Fig. 7.5). Leaving unattached mucosa on the alveolus facilitates closure. This tissue has many elastic fibers and contracts following incision, although, during closure, the tissue can be grasped and it holds sutures well. The incision should not be made more superior in the anterior region because entrance into the piriform aperture, with puncturing the nasal mucosa, may result. Some individuals have extremely low piriform apertures, which make this possibility a reality. Palpation of the inferior extent of the piriform aperture
and/or anterior nasal spine ensures incision placement inferior to these structures. In the edentulous maxilla, where atrophy of the alveolar bone brings the alveolar crest and floor of the nose in close apposition, incision along the alveolar crest is an excellent choice.
and/or anterior nasal spine ensures incision placement inferior to these structures. In the edentulous maxilla, where atrophy of the alveolar bone brings the alveolar crest and floor of the nose in close apposition, incision along the alveolar crest is an excellent choice.
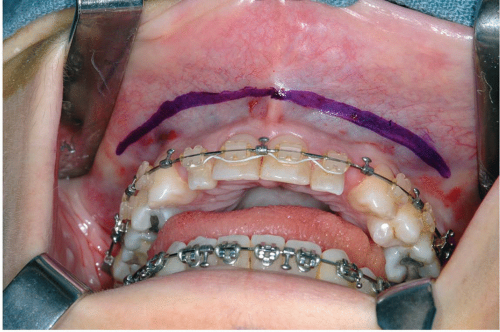
Figure 7.5 Photograph showing location of incision, 3 to 5 mm superior to the mucogingival junction.
|
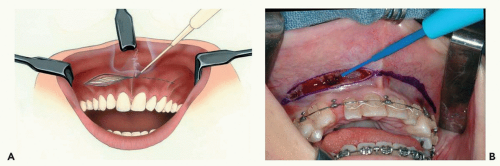
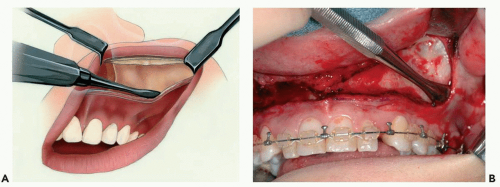
Figure 7.6 Illustration (A) and photograph (B) showing incision through the mucosa, submucosa, facial musculature, and periosteum.
|
The incision extends as far posteriorly as necessary to provide exposure, usually up to the first molar tooth, and traverses the mucosa, submucosa, facial muscles, and periosteum (see Fig. 7.6). The mucosa retracts during incision, exposing underlying tissues.
▶ Step 3. Subperiosteal Dissection of Anterior Maxilla and Zygoma
Periosteal elevators are used to elevate the tissues in the subperiosteal plane (see Fig. 7.7). Dissection of the tissues should be carried out in a specific order, first elevating the superior tissues, then the tissues along the piriform aperture, and then the posterior tissues behind the zygomaticomaxillary buttress. While elevating the tissues superiorly in the subperiosteal plane, small perforating vessels are encountered and are easily distinguishable from the infraorbital neurovascular bundle by their size. The infraorbital neurovascular bundle is identified by dissecting medially and laterally to the location of the infraorbital canal, working toward the bundle. After the bundle is located, the periosteum is dissected completely around the foramen. Dissection proceeds superiorly to the infraorbital rim. Subperiosteal dissection along the piriform aperture strips the attachments of the nasolabial musculature, allowing upward and lateral retraction of the muscles.
Subperiosteal dissection proceeds posteriorly to the pterygomaxillary fissure. Perforation of the periosteum at or behind the zygomaticomaxillary buttress produces herniation of the buccal fat pad into the surgical field, which is a nuisance during surgery. A helpful suggestion is to always keep the tip of the periosteal elevator in intimate contact with bone
when proceeding posteriorly around the zygomaticomaxillary buttress. The only anatomic hazards are the infraorbital neurovascular bundle above and posterior superior alveolar vessels along the posterior maxilla, which infrequently cause bleeding.
when proceeding posteriorly around the zygomaticomaxillary buttress. The only anatomic hazards are the infraorbital neurovascular bundle above and posterior superior alveolar vessels along the posterior maxilla, which infrequently cause bleeding.
The entire anterior face of the zygoma can be easily exposed, but reaching the zygomatic arch necessitates detachment of some of the masseter muscle attachments. Sharp dissection is needed to free these tenacious fibers. Dissection below the piriform aperture up the anterior nasal spine should be performed carefully to maintain the integrity of the nasal mucosa. When violated, the nasal mucosa bleeds profusely.
▶ Step 4. Submucosal Dissection of Nasal Cavity
If it is necessary to strip the nasal mucosa from the lateral wall, floor, or septum of the nose, this maneuver is done carefully, with periosteal or Freer elevators. A forked right-angle retractor is placed over the anterior nasal spine, and superior subperiosteal dissection allows the retractor to retract the septum and nasal mucosa above the level of the anterior nasal spine. A scalpel is used to make a horizontal incision on top of the anterior nasal spine, freeing the cartilaginous septum from the top of the spine and, the attachment of the nasal mucosa from the anterior nasal spine. The rim of the piriform aperture is thin and sharp, and the nasal mucosa is adherent. Periosteal elevators are used to strip the mucosa from the entire circumference of the piriform rim.
Dissection into the nasal cavity is easiest to perform along the lateral wall and floor. The anteroinferior margin of the piriform rim is usually located above the nasal floor. Therefore, after freeing the nasal mucosa from the piriform rim, the elevators should be inserted inferiorly before advancing posteriorly (see Fig. 7.8). Dissection of the lateral wall of the nose is performed by gently inserting a periosteal elevator between the nasal mucosa and the lateral wall of the nasal cavity. It is not advanced deeply until the entire circumference of the lower one half of the piriform has been dissected. The previously taut nasal mucosa can then be relaxed somewhat so that the elevator can be advanced deeper along the lateral wall. The elevator is advanced in a sweeping motion to free the entire lateral wall and floor of its mucosa to the level of the inferior turbinate. The posterior edge of the nasal floor is approximately 45 mm posterior to the piriform aperture and can be felt when the elevator steps off the posterior edge.
Once the lateral wall and floor of the nose are stripped of mucosa, the elevator is placed at the junction of the floor of the nose and the nasal septum. A tenacious attachment of the mucosa to the septal crest of the maxilla must be carefully elevated to prevent perforation. A simple maneuver for stripping the septal mucosa during this approach is to place a Freer elevator along the junction of the septum and the floor of the nose and to twist it so that the edge against the septum is twisted superiorly, freeing the mucosa on the septum.
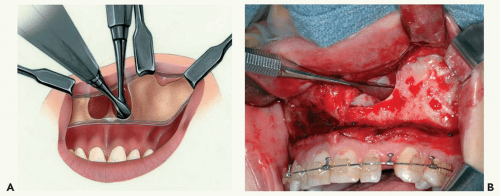
Figure 7.8 Illustration (A) and photograph (B) showing submucosal dissection of the nasal cavity. Note the tip of the periosteal elevator inside the piriform aperture.
|
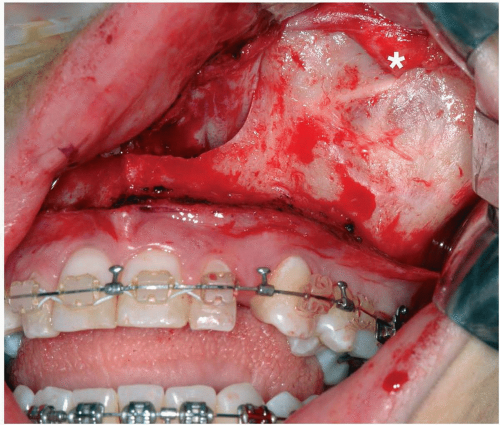
Figure 7.9 Photograph showing exposure of entire face of the left anterior maxilla. Note the position of the infraorbital nerve (*).
|
The entire anterior face of the maxilla is easily exposed using the maxillary vestibular approach (see Fig. 7.9).
▶ Step 5. Closure
Restitution of the nasolabial muscles is performed as three uniform steps during closure of the maxillary vestibular incision. The first step involves identification and resetting of the alar bases, the second involves eversion of the tubercle and vermillion, and the last involves closure of the mucosa.
To help control the width of the alar base, an alar cinch suture is placed prior to suturing the lip. Suture placement is accomplished in one of two ways. In the first, a small-toothed forceps or a single skin hook is placed through the vestibular incision to grasp the insertion of the transverse nasalis muscle. Pulling the instrument medially, allows the change that occurs in the alar base to be seen. A slowly resorbing suture is passed through this tissue, taking care to engage adequate tissue to resist the pull of the suture but not so much tissue that a subcutaneous dimple occurs when the suture is pulled medially. The suture is then passed through the opposite side and temporarily tightened to examine the effect of the medial pull of the alar bases on the nose (see Fig. 7.10). The second method is to evert the tissue into the incision area by pressing the thumb or finger into the alar-facial groove (see Fig. 7.11). A suture can then be passed through the incision, into the tissue, the depth of placement being guided by palpating with the thumb or finger. Whichever method is used to pass the suture through the nasalis muscle, the appearance must be symmetric and the desired curvature and definition of the alar base should be achieved after provisional tying. Tying the suture is delayed until a second suture is passed. The second suture is placed at a higher level or more laterally on the alar base, depending on the desired rotation of the ala. Generally, two sutures are adequate.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses