Chapter 10 Available Bone and Dental Implant Treatment Plans
Long-term success in implant dentistry requires the evaluation of more than 50 dental criteria, many of which are unique to this discipline.1 However, the doctor’s training and experience and the amount and density of available bone in the edentulous site of the patient are arguably primary determining factors in predicting individual patient success. In the past, the available bone was not modified and was the primary intraoral factor influencing the treatment plan. Today the prosthodontic needs and desires of the patient should be first determined, relative to the number and position of missing teeth. After the intended prosthesis is designed, the patient force factors and bone density are then evaluated. The key implant positions, implant number, and size are determined. After these factors are considered, the most important element in the implant region is the available bone. Greenfield already appreciated its importance in 1913.2 This chapter describes the three-dimensional concept of available bone and the implant treatment options for each type of bone anatomy.
LITERATURE REVIEW
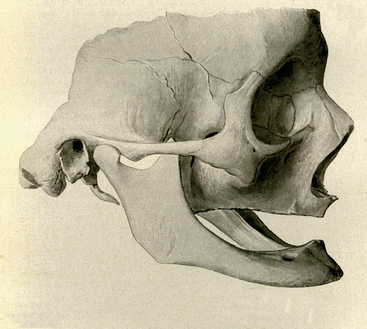
The process of bone volume atrophy after tooth loss and loss of alveolus has been fully documented (Figure 10-1).3–19 Characteristic bone volume changes after tooth loss were evaluated in the anterior mandible by Atwood (Figure 10-2).4–6 The six residual ridge stages are beneficial to appreciate the shapes and range of bone loss. Tallgren reported the amount of bone loss occurring the first year after tooth loss is almost 10 times greater than the following years.7 The posterior edentulous mandible resorbs at a rate approximately four times faster than the anterior edentulous mandible.8 It has been suggested that, in the mandibular synthesis, females present higher total reduction and more rapid bone loss during the first 2 years.9 More recent studies in complete denture wearers have confirmed the higher rate of resorption in the first year of edentulouness.10,11 The anterior maxilla resorbs in height slower than the anterior mandible. However, the original height of available bone in the anterior mandible is twice as much as the anterior maxilla. Therefore the resultant maxillary atrophy, although slower, affects the potential available bone for an implant patient with equal frequency.7 The changes in the edentulous anterior maxillary ridge dimension can be dramatic in height and width (up to 70%), especially when multiple extractions are performed.12 In addition, many patients lose additional bone by simultaneous alveolectomy procedures after tooth extraction before the delivery of a maxillary denture.13 Although slight differences exist between different alveolectomy techniques, all are detrimental to the ridge volume.14

Figure 10-2 Atwood presented a classification of bone loss after tooth loss in the anterior mandible in 1963.
The residual ridge shifts palatally in the maxilla and lingually in the mandible as related to tooth position, at the expense of the buccal cortical plate in all areas of the jaws, regardless of the number of teeth missing.15–19 However, after the initial bone loss, the maxilla continues to resorb toward the midline, whereas the mandibular basal bone is wider than the original alveolar bone position and results in the late mandible resorption progressing facially. This, in addition to a marked change in mandibular position, leads to the classical appearance of the denture wearer with a protruding chin and a mandibular lip.20 The posterior maxilla loses bone volume faster than any other region. Not only does periodontal disease cause initial bone loss before the loss of teeth, the crestal bone loss is substantial after tooth extraction. In addition, the maxillary sinus after tooth loss expands toward the crest of the edentulous ridge. As a result, the posterior maxilla is more often indicated for bone augmentation compared with any other intraoral location.
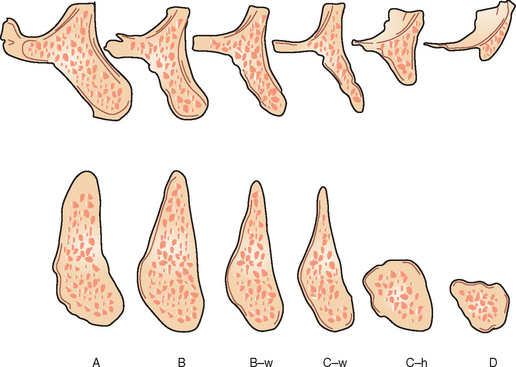
Weiss and Judy21 developed a classification of mandibular atrophy and its influence on subperiosteal implant therapy in 1974. Kent presented a classification of alveolar ridge deficiency designed for alloplastic bone augmentation in 1982.22 Another bone volume classification was proposed by Lekholm and Zarb in 1985 for residual jaw morphology related to the insertion of Brånemark fixtures.23 They described five stages of jaw resorption, ranging from minimal to extreme (Figure 10-3). The mandibular resorption was only described in loss of height. All the five stages of resorption in either arch used the same implant modality, surgical approach, and type of final prosthesis. In addition, as the bone volume decreased, the number of implants decreased.
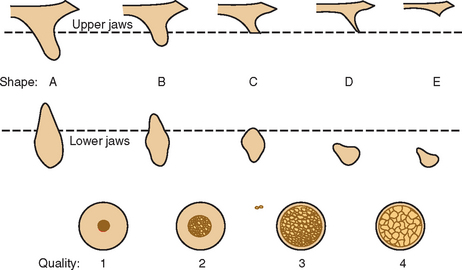
Figure 10-3 Lekholm and Zarb presented a classification of bone loss in the edentulous jaws in 1985.
A maxillary alveolar process of resorption after tooth loss after Atwood’s description for the mandible was presented by Fallschüssel in 1986.24 The six resorption categories of this arch ranged from fully preserved to moderately wide and high, narrow and high, sharp and high, wide and reduced in height, and severely atrophic. The classifications of Atwood, Zarb and Lekholm, and Fallschüssel do not describe the actual resorption process in chronological order and are more descriptive of the residual bone.25 Another bone resorption classification, which included the expansion of the maxillary sinuses, was also proposed by Cawood and Howell in 1988.26 Although similar to other categories, the bone volume changes are not reflective of the changes required for implant placement or bone grafting procedures.
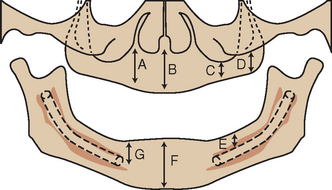
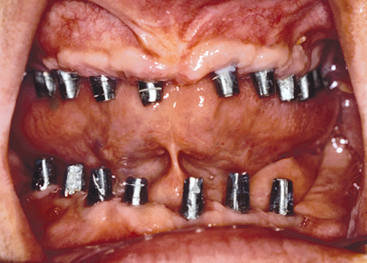
In 1985, Misch and Judy established four basic divisions of available bone for implant dentistry in the edentulous maxilla and mandible, which follow the natural resorption phenomena of each region, and determined a different implant approach to each category.1,27–33 The angulation of bone and crown height were also included for each bone volume, because they affect the prosthetic treatment. These original four divisions of bone were further expanded with two subcategories to provide an organized approach to implant treatment options for surgery, bone grafting, and prosthodontics (Figure 10-4). The ability to organize the available bone of the potential implant site into specific related categories of common treatment options and conditions is of benefit to both the beginning and experienced clinician alike. Improved communication among health professionals and the collection of relevant specific data for each category are also beneficial. The Misch-Judy bone classification has facilitated these processes during the past two decades within the profession, universities, implant programs, and international implant societies.
AVAILABLE BONE
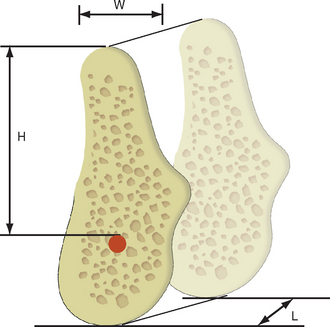
Available bone describes the amount of bone in the edentulous area considered for implantation. It is measured in width, height, length, angulation, and crown height space (Figure 10-5). Historically, the available bone was not modified and dictated the implant position and size. Today, if the bone is inadequate to support an ideal abutment for the intended prosthesis or bone grafting, the ideal site is often indicated or an alternative site may be considered.
Manufacturers describe the root form implant in dimensions of width and length. The implant length corresponds to the height of available bone. Therefore this text refers to root form implant height or length. The width of a root form implant is most often related to the diameter and mesiodistal length of available bone. Most root form implants have a round cross-sectional design to aid in surgical placement; therefore the diameter of the implant corresponds to the implant width. Many manufacturers propose implants with a crest module wider than the implant body dimension. Yet the often stated dimension of the manufacturer is the smaller body width. For example, the Nobel Biocare 3.75-mm-diameter implant has a 4.1-mm-crest module. The clinician should be knowledgeable of all implant dimensions, especially because the crestal dimension of bone (where the wider crest module dimension is placed) is usually the narrowest region of the available bone and where the implant is closest to an adjacent tooth.
Available Bone Height
The height of available bone is measured from the crest of the edentulous ridge to the opposing landmark. The anterior regions are limited by the maxillary nares or the inferior border of the mandible. The anterior regions of the jaws have the greatest height, because the maxillary sinus and inferior alveolar nerve limit this dimension in the posterior regions. The maxillary canine eminence region often offers the greatest height of available bone in the maxillary anterior.34 In the posterior jaw region, there is usually greater bone height in the maxillary first premolar than in the second premolar, which has greater height than the molar sites because of the concave morphology of the maxillary sinus floor. Likewise, the mandibular first premolar region is usually anterior to the mental foramen and provides the most vertical column of bone in the posterior mandible. However, on occasion, this premolar site may present a reduced height compared with the anterior region, because of the anterior loop of the mandibular canal (when present) as it passes below the foramen and proceeds superiorly, then distally, before its exit through the mental foramen (Figure 10-6).
The dilemma of available bone in implant dentistry involves the existing anatomy of the edentulous mandible and maxilla. The initial mandibular bone height is influenced by skeletal anatomy, with angle Class II patients having shorter mandibular height, and angle Class III patients exhibiting the greatest height. The initial edentulous anterior maxillary available bone height is less than the mandibular available bone height. The opposing landmarks for the initial available bone height are more limiting in the posterior regions. The posterior mandibular region is reduced because of the presence of the mandibular canal, approximately situated 12 mm above the inferior border of the mandible. As a result, in the areas where greater forces are generated and the natural dentition has wider teeth with two or three roots, shorter implants, if any, are often used and in insufficient number because of the anatomical limiting factors. A study of 431 patients revealed that in the partially edentulous maxilla and mandible, the placement of posterior implants at least 6 mm in length was possible in only 38% and 50%, respectively. The anterior regions of edentulous arches could receive implants 55% and 61% of the time, respectively.35 The existing bone anatomy of the implant patient often requires modification to enhance long-term implant success. For example, sinus grafts in the posterior maxilla permit the placement of posterior endosteal implants into restored bone height.
The suggested minimum bone height for predictable long-term endosteal implant survival approaches 12 mm. Before 1981 the Brånemark screw–type implant body and osteointegrated approach was provided as a single diameter (3.75 mm) and was used only in the completely edentulous anterior maxilla and mandible.36 The implant drills cut 10 mm deep, and the “10-mm” implant was 9 mm in length. By 1990 this philosophy had been expanded to all jaw regions and many implant sizes. However, failure rates reported in the literature for implants shorter than 9 mm tend to be higher independently from the manufacturer design, surface characteristic, and type of application.37–52 Therefore the initial implant length should approximate 12 mm, because the ideal treatment plan should first be designed. The inexperienced dentist may wish to have 14 mm of bone height to place a 12-mm-high implant body before proceeding with the surgery. This precaution allows 2-mm surgical error or permits an osteoplasty to gain additional width of bone. The 12-mm height minimum applies to most screw-shape endosteal implant designs in good-density (D2) bone. This minimum implant height requirement may be reduced in the very dense bone (D1) in the symphysis of an atrophic mandible, when the prosthesis has fewer forces (as an overdenture) or when the shorter dimension can be compensated by implant number, width, or design.53–55
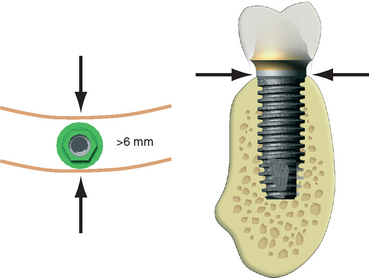
Available Bone Width
After adequate height is available, the next most significant criterion affecting long-term survival of endosteal implants is the width of the available bone. Root form implants of 4-mm crestal diameter usually require more than 6 mm of bone width to ensure sufficient bone thickness and blood supply around the implant for predictable survival. These dimensions provide more than 1 mm of bone on each side of the implant at the crest. Because the bone usually widens apically, this minimum dimension rapidly increases. For root form implants, the minimum bone thickness is located in the midfacial and midlingual contour of the crestal region exclusively (Figure 10-7). The crestal aspect of the residual ridge is often cortical in nature and exhibits greater density than the underlying trabecular bone regions, especially in the mandible. This mechanical advantage permits immediate fixation of the implant, provided this cortical layer has not been removed by osteoplasty.
Available Bone Length
The mesiodistal length of available bone in an edentulous area is often limited by adjacent teeth or implants. As a general rule, the implant should be at least 1.5 mm from an adjacent tooth and 3 mm from an adjacent implant. This dimension not only allows surgical error, but also compensates for the width of an implant or tooth crestal defect, which is usually less than 1.4 mm. As a result, if bone loss occurs at the crest module of an implant or from periodontal disease with a tooth, the vertical bone defect will not spread to a horizontal defect and cause bone loss on the adjacent structure.56 Therefore, in the case of a single-tooth replacement, the minimum length of available bone necessary for an endosteal implant depends on the width of the implant. For example, a 5-mm-diameter implant should have at least 8 mm of mesiodistal bone, so 1.5 mm is present on each side of the implant. A minimum mesiodistal length of 7 mm is usually sufficient for a 4-mm-diameter implant. Of course, the diameter of the implant is also related to the width of available bone and, in multiple adjacent sites, is primarily limited in this dimension. For example, a width of bone of 4.5 mm without augmentation requires a 3.5-mm or smaller implant, with inherent compromises (such as minimal surface area and greater crestal stress concentration under occlusal loads). Therefore in the narrower ridge, it is often indicated to place two or more narrow-diameter implants when possible to obtain sufficient implant-bone surface area to compensate for the deficiency in width of the implant. Because the implants should be 3 mm apart and 1.5 mm from each tooth, 13 mm or more in available bone mesiodistal length may be required when the narrower implant dimensions are used to replace a posterior tooth.
The ideal implant width for single-tooth replacement or multiple adjacent implants is often related to the natural tooth being replaced in the site. The tooth has its greatest width at the interproximal contacts, is narrower at the cement-enamel junction (CEJ), and is even narrower at the initial crestal bone contact, which is 2 mm below the CEJ.57 The ideal implant diameter corresponds to the width of the natural tooth 2 mm below the CEJ, if it also is 1.5 mm from the adjacent tooth. In this way, the implant crown emergence through the soft tissue may be similar to a natural tooth. For example, a maxillary first premolar is approximately 8 mm at the interproximal contact, 5 mm at the CEJ, and 4 mm at a point 2 mm below the CEJ. Therefore a 4-mm-diameter implant (at the crest module) would be the ideal implant diameter, if it also is at least 1.5 mm from the adjacent roots (2 mm below the CEJ).
Available Bone Angulation
Rarely does the bone angulation remain ideal after the loss of teeth, especially in the anterior edentulous arch (Figure 10-8). In this region, labial undercuts and resorption after tooth loss,12,15,16 often mandate greater angulation of the implants or correction of the site before insertion. In the posterior mandible, the submandibular fossa mandates implant placement with increasing angulation as it progresses distally. Therefore, in the second premolar region, the angulation may be 10 degrees to a horizontal plane; in the first molar areas, 15 degrees; and in the second molar region, 20 to 25 degrees.
Crown Height Space
The crown height space (CHS) is defined as the vertical distance from the crest of the ridge to the occlusal plane. It affects the appearance of the final prosthesis and the amount of moment force on the implant and surrounding crestal bone during occlusal loading. The CHS may be considered a vertical cantilever. Any direction of load that is not in the long axis of the implant will magnify the crestal stresses to the implant- bone interface and also to the abutment screws in the restoration. The greater the CHS, the greater the moment force or lever arm with any lateral force or cantilever. Esthetically, the prosthesis is less likely to replace the sole anatomical crowns of natural teeth when a greater CHS is present. The absence of a peri-implant ligament means that the bone-implant stresses cannot be managed by increasing the implant height. Therefore, as the CHS increases, a greater number of implants or wider implants should be inserted to counteract the increase in stress. For an ideal treatment plan, the CHS should be equal to or less than 15 mm for ideal conditions (see Chapter 6).
DIVISIONS OF AVAILABLE BONE
Division A (Abundant Bone)
Division A abundant bone often forms soon after the tooth is extracted. The abundant bone volume remains for a few years, although the interseptal bone height is reduced and the original crestal width is usually reduced by more than 30% within 2 years.12 Division A bone corresponds to abundant available bone in all dimensions (Box 10-1 and Figures 10-9 to 10-11). It should be emphasized that the available bone height may be 20 mm for Division A, but this does not mean the implant length must be equal to the bone height. Because the stresses to the implant interface in good- density bone are captured at the crest of the ridge, an implant of 12 mm or more has been shown to be without compromise for long-term success, even though the implant does not engage the opposing cortical plate.
The Division A width of more than 6 mm is predicated on an implant diameter of at least 4 mm at the crest module, because abundant long-term data have been published regarding this implant size.37,45 In abundant bone width (A+ bone) of greater than 7 mm, a wider (5-mm diameter) implant may be inserted, provided that 1 mm of bone remains around the buccal and lingual aspects of the implant. Osteoplasty may often be performed to obtain additional bone width.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses