To prevent development of white spot lesions, orthodontists should assess each patient’s risk factors before and during treatment. Oral hygiene instruction is important, but patients might need to be assisted with additional measures, including fluoride varnish, chlorhexidine, xylitol, dietary modification, or calcium-containing remineralization products that can help prevent enamel demineralization, enhance remineralization, and modify patient and biofilm factors. Restorative treatment for established white spot lesions can range from the most conservative (remineralization with fluoride, calcium, and phosphate) to the most aggressive (tooth reduction and porcelain veneers).
-
What is the prevalence of white spot lesions in orthodontic practice?
-
Estimates of the overall prevalence of white spot lesions ( Fig 1 ) arising during fixed appliance therapy range widely from 2% and 96%.

Fig 1 White spot lesion. -
In a cross-sectional study, Mizrahi evaluated 527 patients before fixed appliance orthodontic treatment and 269 patients after treatment. There were significant increases in both the prevalence (72.3%-84%) and the severity (opacity index, 0.125-0.200) with treatment. Male patients experienced significantly greater increases in the severity of enamel opacities than did female patients. However, there was no significant sex difference in the prevalence of enamel opacities.
-
In a study by Gorelick et al, individual teeth with fixed appliances exhibited significantly more white spot lesions than did the teeth in the control group. The highest incidence of lesions was found at the labio-gingival area of the maxillary lateral incisors, and the lowest incidence was in the maxillary posterior segment. Interestingly, no white spots were found on the lingual surfaces of mandibular canines and incisors after prolonged use of a canine-to-canine bonded retainer. These findings suggest a relationship between resistance to white spot formation and the rate of salivary flow and emphasize the need for preventive regimens. Despite the lack of any preventive fluoride program among the study groups, 50% of the patients had resistance to white spot formation.
-
What is the etiology of white spot lesion development?
-
White spot lesions are areas of demineralized enamel that usually develop because of prolonged plaque accumulation.
-
Fixed orthodontic appliances create stagnation areas for plaque and make tooth cleaning difficult. The irregular surfaces of brackets, bands, and wires limit the naturally occurring self-cleansing mechanisms of the oral musculature and saliva. This encourages plaque accumulation and the colonization of aciduric bacteria; over time, this results in active white spot lesions, and, if not treated, a cavitated caries lesion can develop.
-
White spot lesions can occur on any tooth surface in the oral cavity where the microbial biofilm is allowed to develop and remain for a period of time. Also impacting their development are the patient’s modifying factors, including medical history; dental history; medication history; diet; levels of calcium, phosphate, and bicarbonate in saliva; fluoride levels; and genetic susceptibility ( Fig 2 ).
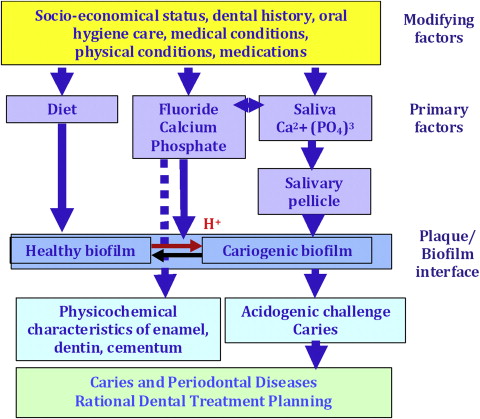
Fig 2 Caries risk-modifying factors(Chalmers 2006, modified from Ngo in Mount and Hume). -
A dynamic and continuous process of enamel demineralization and remineralization occurs that can progress from initial demineralization, to noncavitated lesions, and finally to cavitated lesions. Before the hypermineralized enamel surface layer is lost or cavitated, the demineralization process might encompass the full thickness of the enamel including the outer layer of the dentin. The white spot lesion’s chalky appearance is simply an optical phenomenon caused by mineral loss in the subsurface and the surface of the enamel.
-
What is the clinical differential diagnosis of white spot lesions?
-
White spot lesions can be either noncarious or carious. To differentiate between them, the clinician must first clean and dry the teeth and then closely evaluate the lesions using magnification and adequate lighting. The consistency and texture of the surface can be gently evaluated with a periodontal probe. Carious white spot lesions appear rough, opaque, and porous. Noncarious lesions appear mostly smooth and shiny.
-
Enamel crystal dissolution begins with subsurface demineralization, creating pores between the enamel rods. The alteration of the enamel refractive index in the affected area of a carious white spot lesion is a consequence of both surface roughness and loss of surface shine plus alteration of internal reflection, all resulting in visual enamel opacity, because porous enamel scatters more light than sound enamel.
-
Commonly identified when the teeth are dry, carious white spot lesions are typically found on the buccal surfaces beneath a thick accumulation of plaque and around the perimeter of orthodontic brackets where oral hygiene is difficult. The lesions can extend broadly over the surface of the teeth and sometimes involve proximal extensions. Orthodontic patients with carious buccal white spot lesions should be evaluated for proximal noncavitated and cavitated carious lesions.
-
Noncarious white spot lesions, classified as fluorosis, developmental enamel hypomineralization, and enamel hypoplasia, can have genetic and environmental bases. These noncarious white spots are usually limited to a few teeth (typically, anterior teeth) or generalized throughout the dentition, covering the entire tooth surfaces, and are not associated with orthodontic brackets or bands.
-
How can orthodontic patients at risk for developing white spot lesions be identified?
-
The likelihood of developing white spot lesions increases if the patient has any of the following: inadequate oral hygiene, inappropriate diet (high frequency of elevated carbohydrate beverages and snacks), history of recent caries lesions or high DMFS (Decay Missing Filled Surfaces), and lack of adjunctive preventive measures, such as fluoride or antibacterial exposure, xylitol gum, and calcium-derived supplements.
-
Geiger et al reported a significant association between poor patient compliance with home-care preventive procedures and the formation of white spot lesions in orthodontic patients. Surprisingly, no statistically significant difference was reported between the compliance levels of the sexes or the various age groups.
-
Caries indicators are clinical observations that inform us of a patient’s past caries history and activity. These clinical signs of recent disease and history of caries disease can provide clear information of past dental history. There are 4 strong caries disease indicators: frank cavitation, proximal lesions, white spot lesions, and any restorations or teeth extracted within the last 3 years because of active disease. Any of these indicators puts the patient in a high-risk category.
-
The relationship between refined sugar, frequency of snacks and meals, and dental caries is well documented. Individualized diet evaluation and counseling can be used to emphasize simple concepts to help reduce exposure or frequency of exposure to sugared beverages such as regular pop or soda, juice, and sports drinks, and sour or regular candy. The structure of meals and snacks influences the quantity and frequency of exposure to fermentable carbohydrates and to caries risk. An evaluation of sugared beverage intake is a key item that should be included in a patient’s dietary assessment. Although orthodontists do not typically assess patients’ dietary habits because of resource and time limitations, such evaluations are essential in preventing white spot lesions.
-
As described by Derks et al, preventive and chemoprophylactic products, such as high-fluoride toothpaste or gel, fluoride varnish, and chlorhexidine rinse, gel, or varnish, are rarely prescribed by orthodontists; 95% of orthodontists provide oral hygiene instructions. And 52% prescribe fluoride mouth rinse.
-
The caries risk assessment worksheet used at the University of Iowa College of Dentistry is based on the American Dental Association’s caries risk assessment form that was recommended as a standard of care by its Counsel of Scientific Affairs in 2009. This form is used to identify risk factors that contribute to dental caries as well as protective factors and is available at: http://www.ada.org/prof/resources/topics/topics_caries_instructions.pdf .
-
What strategies should be used to prevent white spot lesions in orthodontic patients?
-
Depending on the patient’s risk factors, a number of suitable agents and therapies can be applied: fluoride toothpastes, gels, varnishes, and mouth rinses; antimicrobials; xylitol gum; diet counseling; and casein derivates.
-
What fluoride treatment is recommended?
-
The use of higher-concentration fluoride toothpastes and gels (1500-5000 ppm) twice a day during orthodontic treatment has demonstrated a demineralization-inhibiting tendency.
-
For many years, fluoride toothpaste has been considered the most effective and widely used method of applying fluoride, in addition to fluoridated water. The efficacy of conventional fluoride toothpaste (1000 ppm) has been documented in many studies; evidence suggests that toothpaste containing 5000 ppm fluoride can further reduce demineralization and enhance remineralization. Recently, it was suggested that patients undergoing orthodontic treatment should brush twice a day with 5000-ppm fluoride toothpaste or gel. This regimen was reported to provide greater prevention than the daily use of 500-ppm sodium fluoride rinse.
-
As part of the recommended fluoride regimen, patients with orthodontic fixed bonded appliances should have an in-office fluoride varnish application at least twice a year; this provides a high concentration of fluoride to the teeth (5% sodium fluoride in an alcohol suspension of natural resins, approximately 22,000 ppm). The American Dental Association’s Council on Scientific Affairs recommends that “moderate-risk and high-risk patients should receive in-office fluoride varnish at six-month intervals. A fluoride varnish application at three-month intervals may provide an additional caries prevention benefit.” In case of poor patient compliance with using preventive protocols at home, it would be advantageous to apply fluoride varnish more than 2 times a year, perhaps at all orthodontic visits.
-
Do fluoride mouth rinses help?
-
In general, fluoride mouth rinses can add an extra exposure of fluoride and might be beneficial to some patients, but there is no strong evidence that fluoride mouth rinses can effectively prevent or reduce the severity of white spot lesions during orthodontic treatment.
-
There is some evidence that a daily sodium fluoride mouthwash is effective in reducing the severity of white spots in people undergoing orthodontic treatment, but it is not strong. Little has been published concerning its use in orthodontic patients or how successfully it minimizes the development of white spot lesions. The method of fluoride delivery is important: a fluoride mouth rinse will work best if it is used regularly by the patient. Geiger et al reported that only 42% of patients rinsed with sodium fluoride mouth rinse at least every other day, but patients who were more compliant had fewer white spot lesions.
-
Do chlorhexidine rinses need to be prescribed?
-
Chlorhexidine mouthwashes might be beneficial as part of an intensive, short-term regimen to prevent white spot caries lesions, when patients have been noncompliant with other oral hygiene regimens.
-
The main goal of antimicrobial therapy is to achieve a shift from an ecologically unfavorable to an ecologically favorable biofilm. Evaluation of salivary counts of Streptococcus mutans by using a semi-quantitative method for analysis is a diagnostic tool that can identify the need for antimicrobials.
-
Chlorhexidine mouthwash used as a complement to fluoride therapy has demonstrated demineralization-inhibiting tendencies in patients with fixed orthodontic appliances. However, its use in reducing the incidence of dental caries and its antimicrobial effect have been moderate. The materials tested that show the strongest evidence, such as 40% chlorhexidine varnish, are not available in the United States, and clinical application protocols vary in studies (percent, time, and frequency); this produces great variations in results.
-
Patients are instructed to use chlorhexidine rinse (available in nonalcohol formulations for patients with xerostomia or saliva dysfunction) for 30 seconds once a day, preferably before bedtime, because saliva flow diminishes overnight, and the concentration of the drug in the oral cavity remains high until morning. A 14-day regimen is usually used ; however, these cationic chemoprophylactic antimicrobial rinses cannot be used within 2 hours after using toothpastes containing anionic sodium lauryl sulfate (eg, Prevident 5000, Colgate, New York City, NY, and others). A drawback of all chlorhexidine products is their tendency to stain the teeth; this can be objectionable to some patients.
-
Can xylitol gum help?
-
Xylitol gum and mints have been shown to be effective as caries preventive agents, in arresting caries lesions, and decreasing the transmission of S mutans from mothers and caregivers to children.
-
Xylitol is a polyol (a type of carbohydrate) that is not a metabolizable substrate for S mutans and can be used as a low-calorie sugar substitute. It is noncariogenic and appears to have antimicrobial properties that help to inhibit S mutans attachment to the teeth, thus making it a good product for decreasing the bacterial load. Since there is no metabolism by bacteria, the salivary pH can remain stable, and the environment will not favor acidogenic bacteria.
-
Makinen et al showed that the systematic use of xylitol chewing gum can significantly reduce the risk of caries compared with gums that contain sorbitol and sucrose. Chewing xylitol gum for 5 minutes, 3 times a day, has shown consistently positive results, but long-term clinical trials with a standardized methodology are needed. The protocol we recommend for moderate and high-risk adult patients is to chew 2 pieces of xylitol gum, 3 to 5 times a day, at least for 10 minutes per chewing episode. In addition, the consumption of chewing gum and mints has been demonstrated to result in increased production of stimulated saliva containing more calcium and phosphate ionic concentrations when compared with nonstimulated saliva. Therapeutically, it is recommended that adults use 6 g of xylitol daily. However, xylitol can cause digestive problems (diarrhea) if the recommended doses are exceeded.
-
Do products containing casein phosphopeptides-amorphous calcium phosphate (CPP-ACP) help prevent or remineralize white spot lesions?
-
The application of products containing CPP-ACP might help to prevent enamel demineralization. However, there is insufficient clinical trial evidence to make a recommendation regarding its long-term effectiveness.
-
CPP-ACP is a nanocluster that binds calcium and phosphate ions in an amorphous form. CPP-ACP has been shown to adhere to the bacterial wall of microorganisms and tooth surfaces. When an intraoral acid attack occurs, the calcium and phosphate ions are released to produce a supersaturated concentration of ions in the saliva, which then precipitates a calcium-phosphate compound onto the exposed tooth surface.
-
Recaldent (CPP-ACP) is available in several forms (gum, solution, MI Paste and MI Paste Plus [GC America, Alsip, IL, USA]), has been shown to reduce dentin hypersensitivity, reduce demineralization of enamel, and enhance remineralization in laboratory studies. An In-vitro study have reported that enamel lesions remineralized with topical exposure to CPP-ACP gum were more resistant to subsequent acid challenges compared with normal remineralized enamel. However, MI Paste and MI Paste Plus have not yet been used specifically in extensive caries clinical trials, and there is insufficient clinical trial evidence (in quality and quantity or both) to make a recommendation regarding the long-term effectiveness of CPP-ACP in preventing caries, treating dentin hypersensitivity, and treating dry mouth.
-
The exact extent of substantivity of Recaldent has been reported to be from 30 minutes to several hours. Thus, several daily applications might be beneficial in high-risk patients, and, for this reason, MI Paste or MI Paste Plus can be recommended for daily use in patients undergoing fixed appliance orthodontic treatment. MI Paste Plus contains 900 ppm of fluoride and so may be helpful with 1000-ppm, but not 5000-ppm, fluoride toothpaste to optimize thorough remineralization and minimize superficial remineralization. If recommended, MI Paste Plus should be used after meals and snacks (if possible) and after brushing with 1000-ppm fluoride toothpaste before, during, and after orthodontic treatment, or MI Paste can be used, if the selected toothpaste contains 5000 ppm of fluoride. A pea-size amount can be gently brushed on and around the teeth and orthodontic appliances. The combination of Recaldent and 900 ppm of fluoride in the MI Paste Plus used with 1000 ppm of fluoride would need to be used for several weeks or months to maximize gradual and thorough remineralization.
-
MI Paste contains milk products and therefore cannot be used in patients with milk-protein allergies, but lactose-intolerant patients can use it.
-
Is there a difference in the type of white spot lesions that improve over time after treatment?
-
The prognosis for an active carious lesion (as opposed to an arrested carious lesion) is considered favorable because of its porosity that allows ready incorporation of calcium phosphate into the enamel and the reaction of fluoride ions with the enamel.
-
White spot lesions that develop during fixed appliance orthodontic treatment appear slightly supragingivally or surrounding the bracket. Usually the surface is dull, pitted, and irregular where the demineralization process has occurred, and plaque signifies an active lesion. A flat or shiny white and sometimes brown surface occurs when the remineralization process has started or has been completed, signifying an arrested lesion.
-
Active white spot lesions usually have a better prognosis to recover the translucency of the enamel than arrested white spot lesions because of their porosity and therefore easier incorporation of calcium phosphate ions. After the removal of fixed appliances, these lesions improve over time with adequate oral hygiene. Arrested lesions have a tendency to result in less favorable esthetic results, because of the lack of enamel porosity and the formation of a remineralized layer in the outer part of the enamel. Unfortunately, after orthodontic treatment, most white spot lesions have already been in a demineralization and remineralization cycle and are most likely arrested, so the prognosis for optimal esthetic outcomes is more questionable.
-
What treatment protocols should be followed after braces are removed?
-
If white spot lesions occur during treatment, it is advisable to first allow the teeth to remineralize naturally. If the lesions persist, professional bleaching of the teeth to diminish the contrast between the white spot lesion and the rest of the enamel surface should be considered. If the effect of bleaching is less than desired, microabrasion is an option. Lastly, aggressive restorative treatment such as direct or indirect veneers could be considered.
-
Within the first few weeks after debanding, there is usually a significant natural reduction of white spot lesion size by remineralization. Nearly half of the original lesions will have remineralized after 6 months with no specific additional treatment.
-
Treatments have been proposed to assist remineralization. Fluoride must not be used in high concentrations because it can arrest remineralization and lead to staining. Low concentrations of fluoride might assist remineralization, but this has not been demonstrated in a prospective randomized study. The application of CPP-ACP products and salivary stimulation by chewing gum might be effective in assisting remineralization. But there are currently no long-term clinical studies that demonstrate an improved benefit over natural remineralization.
-
After the natural remineralization process is allowed to happen, external bleaching might be an option to help camouflage white spot lesions and obtain better esthetic results for the patient. Knösel et al evaluated the efficacy of external bleaching on inactive white spot lesions after fixed orthodontic therapy compared with surrounding enamel areas. The lightness values of both the white spot lesions and the surrounding enamel regions were significantly higher after bleaching compared with the baseline. Sound enamel values increased significantly more compared with white spot lesion values, indicating better color matching of these 2 areas compared with the baseline. All patients were satisfied with the outcome of the bleaching therapy. This study was the first attempt to prove that bleaching therapy can camouflage white spot lesions after removal of orthodontic brackets. If bleaching therapy is used to mask decalcified areas, it must be considered that the microhardness of sound enamel surfaces and demineralized enamel surfaces after bleaching might be reduced. Moreover, the susceptibility to formation of caries-like lesions after bleaching increases. Therefore, this kind of therapy should be restricted only to well-selected patients with perfect oral health and hygiene. Fluoridation should be performed during and after the bleaching therapy to enhance remineralization of bleached teeth.
-
For severe cases, acid microabrasion is recommended when the esthetic results after external bleaching therapy are not satisfactory. Ardu et al described a minimally invasive technique based on reactivation of enamel by elimination of the hypermineralized external layer through microabrasion, followed by daily home application of CCP-ACP. The use of MI Paste Plus (CPP-ACP plus 900 ppm of fluoride) has also been suggested for the treatment of these lesions. “In cases of incipient white spot lesions, the subsurface water can be converted back into enamel because of the neutral ions moving by diffusion through the porous surface. When it reacts with the water, the hydroxyapatite formed will regenerate in the subsurface space. Once 80%-85% regeneration has occurred, the enamel will appear optically normal; this means that the appearance of the white spot lesion also disappears.”
-
Ardu et al stated that this technique eliminated white spot lesions without involving additional restorative procedures; however, this statement is based on clinical case reports. No randomized clinical studies have been published to support these results.
-
Lastly, aggressive restorative treatment such as a direct or an indirect veneer can be considered if the patient still sees the need for further esthetic improvement when white spot lesions cannot be totally removed. No studies address when to determine whether more aggressive restorative treatment, such as resin or porcelain veneers, is necessary only for esthetic purposes to cover white spot lesions. However, the most conservative approach to tooth structure should be considered first.
-
Putting it all together, what would you recommend in the following scenarios? A patient comes to your clinic requesting orthodontic treatment ( Fig 3 ). You note inadequate oral hygiene, generalized gingivitis, plaque accumulation, and white spot lesions at the bucco-cervical surfaces. The patient has no cavitated lesions; therefore, her general dentist referred her to you for treatment. How do you proceed?
-
Discuss with the patient the risk factors, make recommendations according to the problems (eg, diet and oral hygiene behavioral assessment), prescribe high-fluoride (5000 ppm) toothpaste and 0.12% chlorhexidine rinses, and reevaluate in few months to assess whether she has been compliant and able to proceed with orthodontic treatment.





