Armamentarium
|
History of the Procedure
Autogenous bone grafts have a long and well-documented history in maxillofacial reconstruction. The first report of autogenous tibial bone graft for use in the maxillofacial region was by Catone in 1992. Since that time, multiple citations in both the orthopedic and maxillofacial literature have demonstrated the effectiveness of the autogenous tibia bone graft harvest. The tibia bone graft harvest provides an adequate quantity and quality of bone, is technically easy to perform, and has a low complication rate.
History of the Procedure
Autogenous bone grafts have a long and well-documented history in maxillofacial reconstruction. The first report of autogenous tibial bone graft for use in the maxillofacial region was by Catone in 1992. Since that time, multiple citations in both the orthopedic and maxillofacial literature have demonstrated the effectiveness of the autogenous tibia bone graft harvest. The tibia bone graft harvest provides an adequate quantity and quality of bone, is technically easy to perform, and has a low complication rate.
Indications for the Use of the Procedure
The autogenous tibia graft harvest provides cancellous bone that has multiple uses in the maxillofacial region. Essentially, any indication for cancellous bone grafting in the maxillofacial region can be accomplished using the autogenous tibia graft. Traditionally, these autogenous bone grafts were harvested from the iliac crest. Alternatively, surgeons have the options of using banked bone, artificial bone, and now bone morphogenetic protein. The autogenous tibia graft harvest has given surgeons and patients another treatment option for maxillofacial reconstruction. The risks and benefits of each bone grafting technique must be evaluated and individualized for each patient.
Dental implantology, trauma, and reconstruction are the primary uses of autogenous bone grafting in the maxillofacial region. Tibia bone grafts have been used for maxillary sinus lift procedures and to augment existing bone for placement of dental implants. In trauma, tibia bone grafts have been used to treat difficult clinical situations such as defect fractures and atrophic, edentulous fractures of the mandible. There is a wide range of reconstructive needs that can be fulfilled by the autogenous tibia bone graft, such as treatment of pathology defects, alveolar cleft grafting in skeletally mature patients, and restoring continuity defects of the jaws.
Limitations and Contraindications
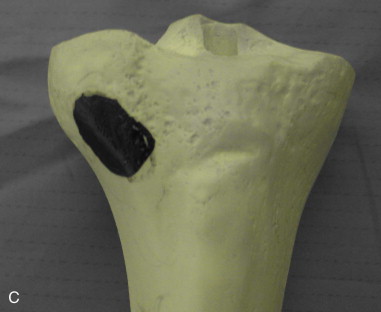
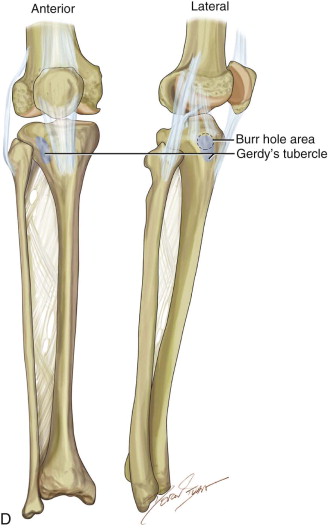
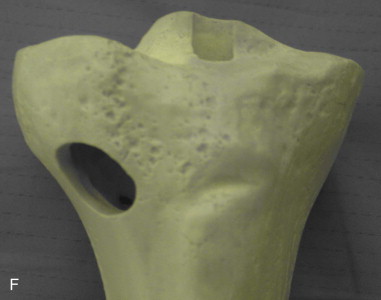
Any surgical procedure has limitations and contraindications, and this certainly applies to the tibia bone graft harvest technique. This procedure is generally performed on skeletally mature patients. There is a growth plate in the tibial plateau region, which can be damaged during the harvest technique. Therefore, we do not perform this procedure on growing patients. However, several authors have successfully reported the safe use of autogenous tibia bone grafts for alveolar cleft grafting procedures in children. The skin over the harvest site should be free of infection or pathology and be in good general condition. It is recommended to avoid sites that have had prior surgery such as fractures with orthopedic hardware or total joint replacements. Careful evaluation of the patient’s activity level should be considered. We have avoided tibia graft harvest on distance runners who place large amounts of force on the tibial plateau on a repetitive basis. Lastly, the surgeon must consider the volume of bone required for the procedure. One can predictably harvest 25 cc of bone from the proximal tibia. Reports have revealed that one may obtain 40 cc of bone from the proximal tibia, which is generally equivalent to an anterior iliac crest bone graft harvest. If larger amounts of bone are required, the surgeon must consider the addition of fillers or an additional autogenous bone graft harvest site. Simultaneous bilateral tibia bone graft harvests have been performed.
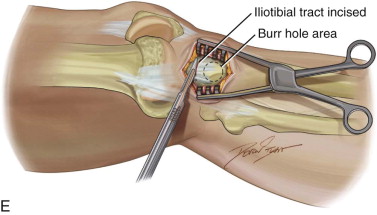
Technique: Tibial Bone Graft
Step 1:
Preparation
The patient should have a sterile surgical preparation of the operative field, which extends 12 inches above and below the planned incision site. The patient is given a broad-spectrum antibiotic prophylaxis such as a cephalosporin within 30 minutes of incision time. Once the incision site has been marked, local anesthesia is infiltrated into the subcutaneous tissues to bone. We have used Marcaine with epinephrine for its vasoconstriction properties and long half-life for patient comfort. A lower extremity tourniquet is applied to the upper thigh and inflated to 50 mmHg above the patient’s systolic blood pressure. If a formal tourniquet is not available, a thigh blood pressure cuff can be used. Time with the tourniquet inflated should be monitored and not exceed 2 hours.
The surgical procedure is generally done in the operating room under general anesthesia as an adjunct to the main maxillofacial procedure. However, the procedure can easily be adapted to the office and performed under intravenous sedation and local anesthesia. The tibia graft harvest techniques can also be done under local anesthesia alone in cooperative patients. ( Figure 123-1, A ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses