Improvements in software removal of scatter artifacts; reduced x-ray dose; and delivery of interpretive reports, analyses, appliances, and images will continue, and use of cone beam volumetric tomography will increase. Distributive networks will be introduced to simplify all of these tasks. Virtual articulators, computer assisted design and computer assisted manufacturing devices will improve, and online delivery of some of these services will increase concomitantly. Consequently, dentistry will improve and, along with it, patient care.
This issue of Dental Clinics of North America has covered old and new imaging modalities, their current applications, and some more contemporary applications such as image-guided surgery. What is left to be said?
I will start first with what dentists and oral and maxillofacial radiologists will most likely not do, even with our newest imaging technique—cone beam volumetric tomography (CBVT).
Although at least one manufacturer has previously shown vessels in the head and neck region in their CBVT machine brochure, dentists and oral radiologists will probably never do contrast procedures. Blood is not stationary, and to see the flow patterns, contrast nonionic agents such as Omnipaque (GE Healthcare, Piscataway, New Jersey) are used. Many of us have used these agents for sialography in the past, but this salivary gland investigative technique is labor intensive and has largely been replaced by conventional CT with contrast and MRI for salivary gland evaluation.
We are neither trained to perform these interventions, nor do we require any application for evaluation of head and neck problems with which we deal. Cerebral angiography is used to detect aneurysms, clots that have made their way to the brain giving rise to stroke and other vascular problems. The catheter is inserted into the femoral or carotid artery, and the injected contrast medium administered. The procedure takes hours to perform and must be done in a hospital setting by an interventional radiologist. We will never be trained or licensed to do these procedures. We cannot image vessels in the head and neck region with cone beam technology.
Another “head and neck” radiology task we will never perform is the interpretation of neurologic structures in the brain—at least with CBVT. The exposure factors and the image acquisition technique do not allow us to visualize “gray and white” matter of the brain. In fact, we wouldn’t want it to. Again, although many oral and maxillofacial radiologists are “familiar” with the features of disorders and disease affecting the brain such as multiple sclerosis and disseminated herpetic lesions, we are neither trained nor licensed to perform interpretation of these neural structures and problems. And, luckily for us, CBVT cannot image these types of problems. The CBVT machines and techniques are suitable for bone and some soft tissue imaging tasks we require but are vastly inferior to conventional CT for most medical problems.
Finally, it is my opinion that dentists and dental specialists will never completely replace some conventional imaging techniques such as intraoral and panoramic with CBVT.
These restrictions aside, CBVT has opened a new door for all of us in the dental profession. We can now perform limited imaging tasks, like our medical radiology colleagues, with software tools that rival theirs for visualization of anatomy and pathology specifically related to our desired applications. Let’s now see what the “future” might hold for us with all of the imaging techniques available. What follows is a series of questions we’ve been asked or ask ourselves, followed by my “predictions” of how and why oral and maxillofacial imaging techniques will evolve.
Predictions for intraoral, panoramic, and “advanced” imaging modalities
Question #1: Will intraoral and panoramic imaging disappear or be replaced by CBVT?
My response is a resounding, “NO!” Certainly the ability to “slice” through a patient’s dental anatomy at 0.15 mm thicknesses could uncover a carious lesion, right? The answer is “Yes” and “No.” Although we can see cavitations in some volumes more precisely ( Fig. 1 ), in others the scatter artifact, running horizontally through the occlusal region, will obscure many lesions ( Fig. 2 ). Besides, it is currently, and I think for many years to come, unjustified to use CBVT for caries detection . Why you might ask?
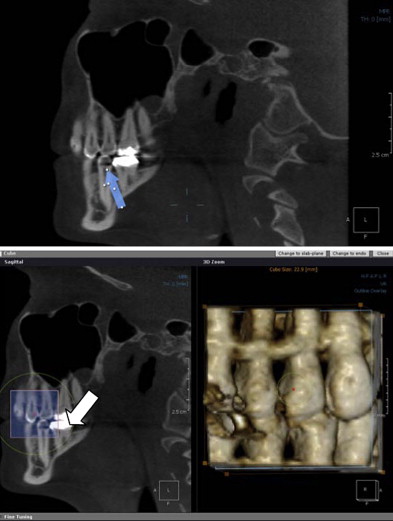
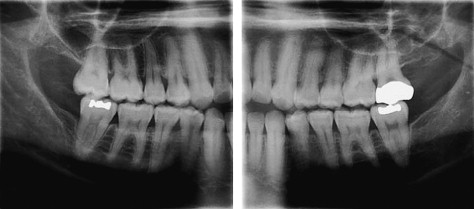
First, as low as the x-ray doses are for CBVT machines, the x-ray dose is still too high for many dental imaging tasks. Second, the simpler, more conventional techniques to image interproximal cavities still have the highest resolution. In addition, certain panoramic machines can now provide high-resolution interproximal images, collimated to reduce dose and provide periapical information that may reduce the total number of intraoral images we require for treatment planning ( Fig. 3 ). The large bitewing images below also could replace some posterior intraoral images from the cuspid posteriorly. Note how they even give a detailed view of the third molar region. This would leave only a few anterior views in an initial new patient examination. And, those are the images the auxiliary likes to do!
Prediction #1 Although we may use fewer intraoral images, both bitewing and periapical, and even with advances in panoramic techniques and software that can replace some intraoral images, we still will need the higher resolution capability of film or digital intraoral images for high-risk “caries patients” to see the earliest lesions. Cone beam imaging will not replace intraoral or panoramic.
Question #2: Will tomography or panoramic imaging technique be replaced by CBVT?
My response to this question is a hearty “Yes”! Although tomographywas considered “state-of-the-art” for implant planning, even with the best machines and tomographic programs that are available in some panoramic machines, the technique is “labor intensive” once again. Despite the acceptable quality that these images may have, they cannot be made thin enough to precisely locate the alveolar crest in many cases. The technique’s magnification factors with either dedicated tomography or panoramic tomography programs must always be considered. Clinicians still have to factor in these technique parameters and leave the traditional 2 mm of “safety margin.” With CBVT the measurements are accurate to within 1/10 mm in most software. And, all structures are rendered in a 1:1 ratio in the image reconstruction software. The margin of error is more precise with CBVT. You can “recapture” 1 to 1.5 mm of space that might mean the difference between being able to place a fixture and not being able.
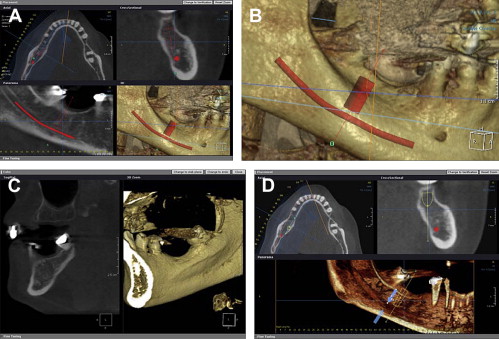
As an aside, many clinicians first encountering CBVT images, and stuck in their conventional imaging techniques, confuse the term 1:1 ratio with their perception of “life size!” If the structures are rendered in a precise 1:1 ratio, we can make the image of an implant site into an 8- × 11-inch glossy print. And if the measured length says 12.2 mm, it IS 12.2 mm to within 1/10 of a millimeter! You do not have to use tiny little transparency overlays with implant icon fixtures over a tiny little image of the mandible or maxilla. Those days are gone! That is not the “state-of-the-art” any longer. Images like that in Fig. 4 illustrate this point.
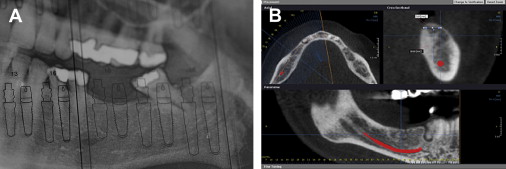
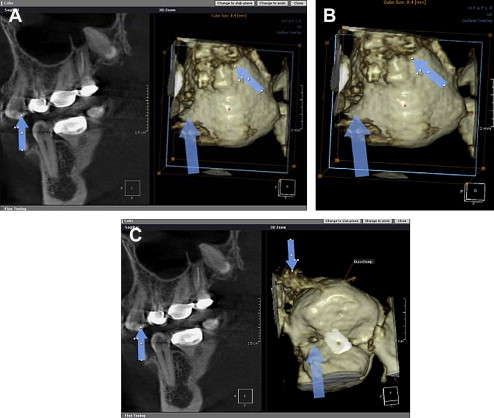
As for panoramic imaging remaining a “standard of care,” I can state this. In my opinion it really was never a standard of care. Clinicians, including oral and maxillofacial surgeons, were placing themselves at some risk for using a panoramic image as the sole radiographic means of implant site assessment. Some still do. Now that CBVT has become so widely available, the use of a panoramic image, with the myriad of positioning errors made and the lack of the cross-sectional information cannot be justified. Anyone who persists using this image as their only image for implant site evaluation will have a serious liability issue in my opinion. Fig. 5 A–D show the improved information available with CBVT technique software.
Prediction #2 CBVT will replace conventional tomography as the “standard of care,” and should now be used in place of panoramic imaging to assess any implant site.