This article addresses technologic advances in endodontics pertaining to new and emerging technology. Cone-beam computed tomography and optical occurrence tomography are 2 new imaging technologies that can assist the practitioner in the diagnosis of pulpal disease. The self-adjusting file and the Apexum device can be used for instrumentation and bulk debridement of an apical lesion, respectively. Neodymium:yttrium-aluminum-garnet laser, erbium:chromium:yttrium-scandium-gallium-garnet laser, EndoActivator, EndoVac, and light-activated disinfection may assist the practitioner in cleaning the root canal system. Computed tomography-guided surgery shows promise in making endodontic surgery easier, as does mineral trioxide aggregate cement for regenerative endodontic procedures.
According to the Merriam-Webster dictionary, technology is the practical application of knowledge especially in a particular area. It is also the specialized aspects of a particular field of endeavor. What is modern endodontic technology? As mentioned by various endodontic Web sites, modern technology is listed as: rotary nickel titanium (NiTi) instruments, apex locators, ultrasonics, the dental operating microscope, bonded resin root canal obturation, and mineral trioxide aggregate (MTA). Although all these technologies are considered technologic advances in root canal treatment, many have been commercially available for more than 10 years. Trade journals have advertisements about new techniques and advances in endodontics. Claims such as “300% less likely to separate,” “The right tool for the job,” “GP free endodontics,” and “Truly revolutionary” were listed. The trade journals are also filled with testimonials such as “This stuff was sent straight down from the top of Mount Olympus,” and “Stress free, superior Endo, While saving time and money. You’ll be a winner.” So what is the difference between advertising, marketing, and proven technology? The answer is the dental literature. How does a practitioner know when to make the leap to a new, possibly, unproved technology? Is it intuition, preliminary research, case studies, or controlled studies based on outcome?
This article addresses the technologic advances in endodontics pertaining to new and emerging technology. These technologic advances are separated into 5 categories: diagnosis, instrumentation, irrigation, surgery, and MTA cement. Dentists should use caution with a new device or material that lacks definitive published research.
Diagnosis
To assist in a pulpal diagnosis, tests such as biting, chewing, percussion, apical palpation, hot, cold, and an electric pulp test are used. On November 8, 1895, Wilhelm Röntgen produced and detected radiographs. Otto Walkhoff, DDS MD, in Brunswick, Germany took the first dental radiograph in January 1896. Since then, dental radiographs have become a fundamental part of diagnosing disease of pulpal origin. They are used to determine the presence of multiple roots, multiple canals, resorptive defects, caries, restoration defects, root fractures, the extent of root maturation, and the detection of pathosis.
Many investigators became aware of the limitations of dental radiographs. Drs Bender and Seltzer realized that lesions in cancellous bone cannot be detected roentographically, and early stages of bone disease cannot be detected by means of roentgenograms. In addition, the size of a rarefied area on the roentgenogram is not correlated with the amount of tissue destruction. In an article by Goldman and colleagues, there was agreement for the presence of pathosis in only 50% of the radiographically evaluated cases.
Two imaging technologies in endodontics are presented in this section: cone-beam computerized tomography (CBCT) and optical coherence tomography (OCT). CBCT is frequently cited in dental literature, and is a necessary radiographic adjunct for diagnosis for some endodontic cases. OCT is an emerging technology in dentistry, but well proved in ophthalmology.
CBCT
CBCT is more sensitive in detecting apical periodontitis compared with periapical radiographs (PARs). It is a reliable method to detect the MB2 canal in the maxillary first molars, and aids in determining the severity of root canal curvature. With the assistance of a CBCT scan, La and colleagues identified independent middle mesial canals in the mandibular first molar. CBCT scans are also effective for detecting vertical root fractures of different thickness. A CBCT scan seems useful in the evaluation of inflammatory root resorption, and its diagnostic performance is proved to be better than that of periapical radiography. Similar to PARs, a CBCT scan is not a reliable diagnostic method for differentiating radicular cysts from granulomas.
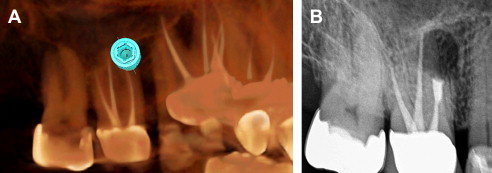
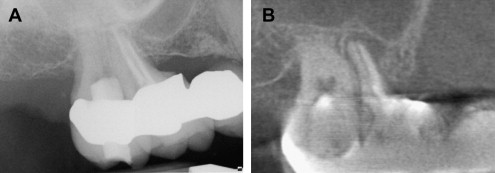
The CBCT can detect an apical radiolucency that may not readily show up on a PAR because of minimal cortical plate erosion. Fig. 1 A shows a digital PAR and Fig. 1 B shows a CBCT scan of teeth numbers 2 and 3.
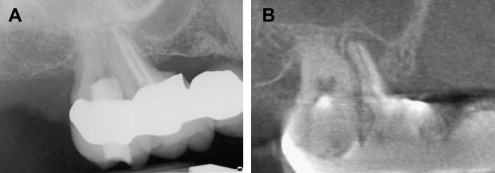
CBCT with proprietary software can reassemble a virtual tooth on a computer, showing exact root morphology. Fig. 2 A shows tooth number 25 with periapical radiolucency. Fig. 2 B and C, both taken with a CBCT scan, illustrate the vertical root fracture, making this tooth nonrestorable.
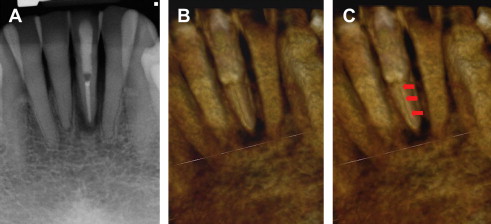
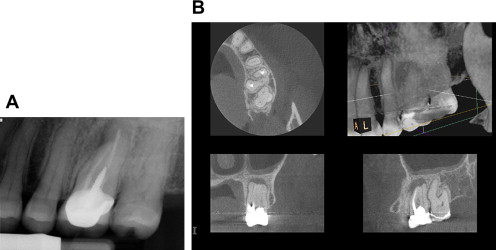
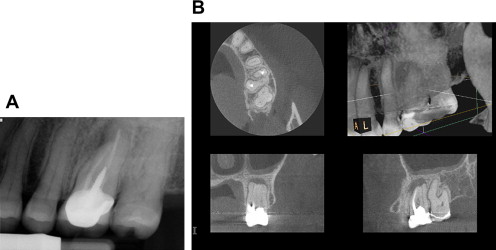
Fig. 3 A shows tooth number 14 with periapical radiolucency over the mesiobuccal root. On the other hand, the CBCT series (see Fig. 3 B) shows the absence of an obturated mesiolingual and distal buccal canals with a lesion surrounding the entire apex of the tooth. The additional information provided by a CBCT scan is invaluable in determining the prognosis of an endodontic retreatment. A recent study on the outcome of root canal treatment in dogs determined by periapical radiography and CBCT scans, concluded that CBCT was a more accurate way to determine the presence or absence of apical lesions after root canal treatment. CBCT may be the future standard to determine if periapical disease has resolved after completion of root canal treatment.
The CBCT has proved itself to be a necessary tool for endodontic diagnosis, as long as clear guidelines for endodontics are addressed. Perhaps the biggest concern is the amount of ionizing radiation that the patient is exposed to. Ionizing radiation, such as dental radiographs, has enough energy to damage DNA in cells, which may lead to cancer. Furthermore, dental radiography has also been associated with low infant birth weight.
The American Dental Association Council on Scientific Affairs recommends that dentists should weigh the benefits of dental radiographs against the consequences of increasing a patient’s exposure to radiation and implement appropriate radiation control procedures. The American Association of Endodontists (AAE) has a position paper on the use of CBCT for endodonticts. The AAE recommends using the ALARA principle, which stands for as low as reasonably achievable. I use CBCT in approximately 10% of all cases. However, if the device had no ionizing radiation output, I would use this technology for every case.
CBCT
CBCT is more sensitive in detecting apical periodontitis compared with periapical radiographs (PARs). It is a reliable method to detect the MB2 canal in the maxillary first molars, and aids in determining the severity of root canal curvature. With the assistance of a CBCT scan, La and colleagues identified independent middle mesial canals in the mandibular first molar. CBCT scans are also effective for detecting vertical root fractures of different thickness. A CBCT scan seems useful in the evaluation of inflammatory root resorption, and its diagnostic performance is proved to be better than that of periapical radiography. Similar to PARs, a CBCT scan is not a reliable diagnostic method for differentiating radicular cysts from granulomas.
The CBCT can detect an apical radiolucency that may not readily show up on a PAR because of minimal cortical plate erosion. Fig. 1 A shows a digital PAR and Fig. 1 B shows a CBCT scan of teeth numbers 2 and 3.
CBCT with proprietary software can reassemble a virtual tooth on a computer, showing exact root morphology. Fig. 2 A shows tooth number 25 with periapical radiolucency. Fig. 2 B and C, both taken with a CBCT scan, illustrate the vertical root fracture, making this tooth nonrestorable.
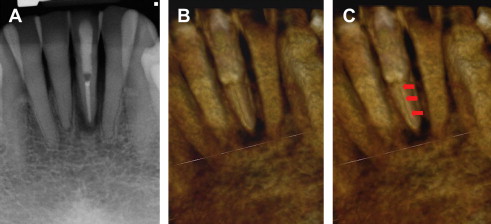
Fig. 3 A shows tooth number 14 with periapical radiolucency over the mesiobuccal root. On the other hand, the CBCT series (see Fig. 3 B) shows the absence of an obturated mesiolingual and distal buccal canals with a lesion surrounding the entire apex of the tooth. The additional information provided by a CBCT scan is invaluable in determining the prognosis of an endodontic retreatment. A recent study on the outcome of root canal treatment in dogs determined by periapical radiography and CBCT scans, concluded that CBCT was a more accurate way to determine the presence or absence of apical lesions after root canal treatment. CBCT may be the future standard to determine if periapical disease has resolved after completion of root canal treatment.
The CBCT has proved itself to be a necessary tool for endodontic diagnosis, as long as clear guidelines for endodontics are addressed. Perhaps the biggest concern is the amount of ionizing radiation that the patient is exposed to. Ionizing radiation, such as dental radiographs, has enough energy to damage DNA in cells, which may lead to cancer. Furthermore, dental radiography has also been associated with low infant birth weight.
The American Dental Association Council on Scientific Affairs recommends that dentists should weigh the benefits of dental radiographs against the consequences of increasing a patient’s exposure to radiation and implement appropriate radiation control procedures. The American Association of Endodontists (AAE) has a position paper on the use of CBCT for endodonticts. The AAE recommends using the ALARA principle, which stands for as low as reasonably achievable. I use CBCT in approximately 10% of all cases. However, if the device had no ionizing radiation output, I would use this technology for every case.
OCT
OCT is essentially an optical ultrasound that emits no radiation yet provides detailed information to the operator. It is widely used to obtain high-resolution images of the retina and the anterior segment of the eye.
OCT was first mentioned in the proceedings of the International Conference on Optics in Life Sciences in 1990, with the first in vivo images published in 1993. OCT is indicated for morphologic tissue imaging at a high resolution (better than 10 μm). This strategy gives it an advantage over ultrasound and magnetic resonance imaging, which are not ideal for tissue imaging.
OCT was first mentioned in the dental literature in 1998. Since then, more than 50 articles have been published on the benefits of OCT in dentistry. It is used to image hard and soft dental tissue, enamel demineralization and remineralization, and early caries. OCT is useful for a noninvasive approach on periodontal diagnosis, and to help visualize periodontal ligament changes in orthodontic movement.
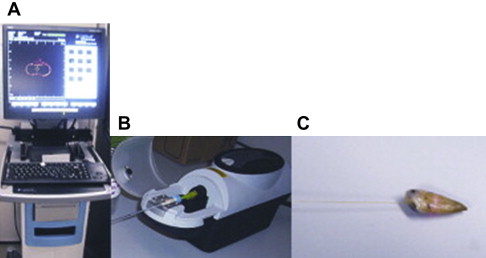
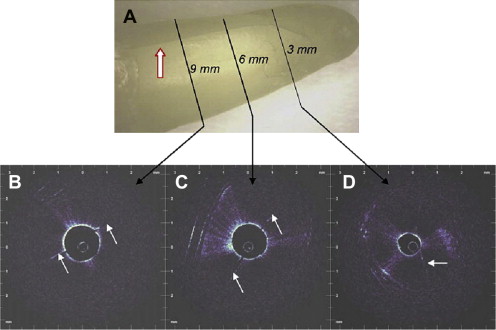
Shemesh and colleagues obtained OCT scans with a Lightlab imaging M2-CV system in combination with an ImageWire 2 catheter. This system is designed for intracoronary imaging in atherosclerotic plaque diagnosis. It is commercially available for clinical use in cardiac catheterization laboratories ( Fig. 4 ). Shemesh and colleagues also reported that OCT is a promising nondestructive imaging method for the diagnosis of vertical root fractures ( Fig. 5 ), and holds promise for full in vivo endodontic imaging to assess intercanal anatomy, cleanliness of the canal after preparation, and perforations. OCT scans can help determine the interface of the human pulp-dentin complex, and may be used in the future to prevent iatrogenic exposures of the pulp. Optical occurrence tomography was used in the laboratory to investigate apical microleakage after laser-assisted endodontic treatment.
OCT is an optical signal acquisition and processing method. It captures micrometer resolution and three-dimensional images from within optical scattering media. It is commercially available for ophthalmologic medicine, and used in art conservation. There is no commercially available product for use in dentistry. Future applications in dentistry may include caries detection, periodontal probing, digital impression taking, cancer screening, and endodontic imaging.
Instrumentation
The ideal endodontic instrument has yet to be invented. Ideally, it would be a single instrument that would navigate the canal to working length with ease. It would not break, ledge, or perforate the canal, as well as remove all the canal contents and preserve the dentin. Until approximately 20 years ago, endodontics relied on carbon and stainless steel instruments. NiTi rotary instrumentation has forever changed endodontic instrumentation. This is not a new technology. It is a modern technology proved in the dental literature, but it has limitations.
Perhaps the most frustrating shortcoming of NiTi instruments is file breakage. Torsional stress and cyclic fatigue are 2 frequently studied components of instrument separation. Torsional failure, which may be caused by using too much apical force during instrumentation, occurs more frequently than flexural fatigue, which may result from use in curved canals. Cyclic failure increases with increasing cross-sectional area. When the working end of a NiTi rotary file was bound, smaller files broke with less torque, as did files in more acute curvatures. Clinical use significantly reduces cyclic fatigue. Zhang and colleagues concluded that the cross-sectional design has a greater effect than taper or size of the instrument on the stresses developed in the instrument under either torsion or bending. Certain cross-sectional configurations are prone to fracture by excess torsional stress. Plotino and colleagues reviewed several devices that were used in the endodontic literature for cyclic fatigue testing. These investigators discovered that the differences in methodology affected the fatigue behavior of rotary instruments and outcome of studies, and recommended an international standard for cyclic fatigue testing.
Manufactures have come up with novel ways to prevent file breakage, such as increasing the pitch length, electropolishing, thermal nitridation, M-wire, and twisting the NiTi metal rather than milling it. Schrader and colleagues reported that an instrumentation sequence encompassing various tapers seems to be safer regarding torsional and fatigue failure compared with a sequence that used 1 single taper.
Hundreds of studies were performed testing NiTi rotary files, but this metal has limitations. We need to move away from NiTi and investigate other metals.
Ferrous Polycrystalline Shape-memory Alloy
Ferrous polycrystalline shape-memory alloy shows huge superelasticity. The iron alloy has twice the maximum superelastic strain obtained in NiTi alloys. The stress level is high so the alloy can be made into a thin wire that can reach the inner part of the body like the brain to deliver stents. Investigations are under way to determine if this metal has a practical application in endodontic rotary instruments.
Self-adjusting File
Another novel approach is to change the instrument design entirely. The self-adjusting file (SAF) (ReDent-Nova Inc, Ra’anana, Israel) was first introduced in the dental literature in April 2010. It is a hollow, thin cylindrical NiTi lattice that adapts to the longitudinal and cross-section of the root canal ( Fig. 6 ). The file is elastically compressible from a diameter of 1.5 mm to dimensions to those of a number 20 stainless steel K-file. Rather than a drilling or reciprocating action, the SAF is operated with a transline (in and out) vibrating handpiece with 3000 to 5000 vibrations per minute. This action has a scrubbing, sandpaperlike effect on the canal walls. The hollow design allows for constant irrigation throughout the procedure. Metzger and colleagues showed that the SAF operation resulted in root canal walls that were free of debris in all thirds of the canal in all (100%) of the samples. In addition, smear layer-free surfaces were observed in 100% and 80% of the coronal and middle thirds of the canal, respectively. In the apical third of the canal, smear layer-free surfaces were found in 65% of the root canals.
More research needs to be undertaken on this new file system. A limitation is the preestablishment of a glide path equivalent to a size 20 K-file before using the SAF. Overall, the SAF seems to have an advantage in cleaning and shaping oval canals, and may be a great adjunct to existing NiTi rotary instrumentation technologies.
Apexum Device
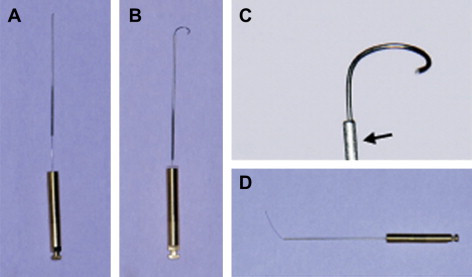
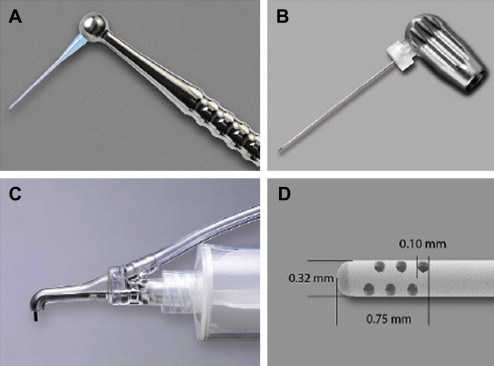
A new device developed by Apexum Ltd (Or-Yehuda, Israel) is based on minimally invasive removal of periapical chronically inflamed tissues through a root canal access. The Apexum device consists of 2 instruments: an Apexum NiTi ablator and an Apexum polyglycolic acid (PGA) ablator. The Apexum NiTi ablator is composed of a hollow tube, a sheath ( Fig. 7 A), and a NiTi precurved metal wire (see Fig. 7 B). The hollow tube and sheath are inserted into the canal to within 1 mm of the tooth apex. The NiTi precurved metal wire goes through the hollow tube into the periapical lesion (see Fig. 7 C). When the Apexum NiTi ablator is rotated at 250 revolutions per minute (rpm) using a slow handpiece it breaks up the periapical tissues. The second instrument, the Apexum PGA ablator, is a bioabsorbable filament, which is inserted through the sheath into the periapical tissues (see Fig. 7 D). This instrument whips into the periapical lesion at 7000 rpm for 30 seconds and liquefies its contents to be rinsed and then suctioned out.
This technology is presented after only 1 publication in the Journal of Endodontics . Metzger and colleagues showed that removing or debulking of the periapical inflamed tissue, using the Apexum procedure, seems to enhance healing kinetics with no adverse effect. More research needs to be completed to establish this technique as a viable treatment modality.
The Apexum device requires the root canal preparation to be open to a number 40 master apical file. A study by Usman and colleagues showed that a size 20 apical preparation with greater taper (GT) rotary instruments left more bacteria and debris in the apical third than a size 40 GT preparation. The conclusion was that apical third cleanliness could be predicted mainly by instrument size. Kvist and Reit studied the results of endodontic retreatment and concluded that even although the surgical retreatment seemed to result in a more rapid periapical bone fill after 4 years, results were similar between the 2 treatment modalities.
Lin and colleagues found it is not necessary to completely curette out all the inflamed periradicular tissues during surgery, because this granulationlike tissue is incorporated into the new granulation tissue as part of the healing process. Controlling the source of irritants in the root canal is more important than removing all periradicular tissues affected by the irritants.
The idea of having another instrument in our armamentarium that can help even 1 more patient heal faster, with low morbidity, makes this an instrument worthy of more study.
Lasers
No article on the technologic advances in endodontics is complete without the mention of lasers. A search of dental lasers in the US National Library of Medicine National Institute of Health ( http://www.pubmed.gov/ ) resulted in more than 4000 entries dating back to 1964 on the use of lasers in dentistry.
In the endodontic literature the neodymium:yttrium-aluminum-garnet (Nd:YAG), erbium:chromium:yttrium-scandium-gallium-garnet (Er:Cr:YSGG), and the erbium: yttrium-aluminum-garnet (Er:YAG) are the lasers that are most studied. The Nd:YAG laser has been shown to significantly reduce the number of bacteria, and reduced apical leakage after root canal obturation. Another study stated that there were no significant differences between laser-irradiated and nonlaser-irradiated groups. The Nd:YAG laser can soften gutta percha for retreatment and is an effective tool for the removal of root canal obturation materials. In addition, temperature rises on the root surface ranging from 17°C to 27°C can occur. A temperature increase greater than 10°C can be detrimental to the attachment apparatus.
The Er:Cr:YSGG laser is developed and manufactured by Waterlase MD (Biolase Technology, Irvine, CA, USA). This laser is equipped with a 200-μm radially emitting laser tip. The tip diameter is equivalent to a number 20 file. It can be used to remove the smear layer and debris from the root canal and reduce bacteria. An in vitro study by Rahimi and colleagues showed that the laser could be used for an apical preparation in root end surgery. The laser preparation resulted in fewer cracks and chipping compared with ultrasonics.
Conflicting in vitro studies were recently published in the Journal of the American Dental Association . Jha and colleagues concluded that neither the laser nor rotary instrumentation was able to eliminate endodontic infection. Contrarily, Gordon and colleagues found that bacterial recovery decreased when duration or power of laser irradiation increased. These last 2 studies simulated straight canals that were opened to a large diameter. More research is needed, especially to determine bacterial reduction or elimination around curved canals.
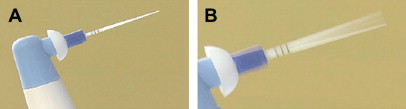
The Er:YAG laser might be suitable for clinical application, as a suppressive and removal device of biofilms in endodontic treatments, and it can be a potential therapy for human infected root canals. An Er:YAG laser that has recently been marketed in dentistry is the Powerlase (Lares Research, Chico, CA, USA). It has photon-induced photoacoustic streaming that has not been studied or published in the dental literature.
Because pulsed lasers create pressure waves in irrigant fluids within the root canal, the potential for extrusion of fluid from the apex should be considered when assessing intracanal laser treatments in endodontics.
Research has not proved that lasers are superior to other treatment modalities. The practitioner has to decide if the cost and risks associated with a dental laser outweigh its benefits. Most endodontic studies have used the laser for cleaning, shaping, and disinfection of the root canal system. There are no published case-controlled studies that show that the laser yields a higher degree of success than current endodontic procedures.
Irrigation
The goal of root canal treatment is total eradication of all bacteria from the canal system before obturation. A study by Nair and colleagues showed that 88% of teeth that were instrumented with stainless steel and NiTi rotary instruments, irrigated with 5.25% sodium hypochlorite (NaOCl), rinsed with 17% ethylenediaminetetraacetic acid and obturated with gutta percha and zinc oxide eugenol cement, still contained viable bacteria in the apical one-third of the root. In a study by Peters and colleagues, a microcomputed tomography scan was used to determine that a large portion of canal surfaces remained unchanged during NiTi preparation. Irrigation helps with the removal of debris, destruction of microorganisms, dissolution of organic debris, removal of the smear layer, and disinfecting areas inaccessible to endodontic instruments. There is no single irrigating solution that alone sufficiently covers all of the functions required from an irrigant. This section discusses 3 new ways to help reduce the number of viable organisms in the root canal system using adjuncts to irrigation alone.
EndoActivator
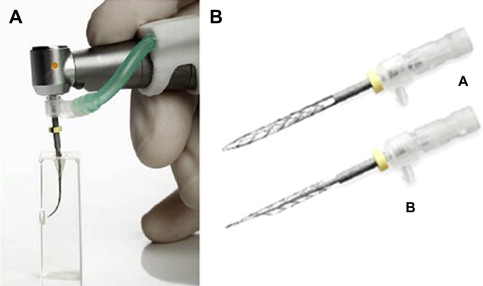
The EndoActivator (Advanced Endodontics, Santa Barbara, CA, USA) is a device that agitates solutions subsonically ( Fig. 8 ). Thirty seconds of NaOCl subsonic agitation with the EndoActivator seems to be slightly more effective in reducing bacterial load in the root canal compared with NaOCl irrigation alone. The EndoActivator provides a better irrigation of lateral canals compared with traditional needle irrigation alone, and it extrudes statistically less irrigant beyond the apex.
However, there is no statistically significant difference in canal isthmus cleanliness when used as an adjunct to aid in canal debridement compared with irrigation alone. Shen and colleagues showed that the structure of biofilm did not show any obvious change when 2 chlorhexidine solutions, surrounding the biofilm, were exposed to continuous ultrasonic or sonic agitation. Furthermore, Huffaker and colleagues revealed that there is no significant difference in the ability of the EndoActivator and a standard irrigation control group to eliminate cultivable bacteria from root canals.
EndoVac
Unlike conventional irrigation that uses positive pressure; the EndoVac system (Discus Dental, Culver City, CA, USA) is a negative pressure device. It consists of a disposable syringe, EndoVac macrocannula, and microcannula. After a complete instrumentation of the root canal system, the EndoVac system is first applied to flush the chamber with an irrigation/suction tip attached to a disposable syringe ( Fig. 9 C). Gross debris in the canal is removed with the macrocannula (see Fig. 9 A) while the dental assistant continuously adds irrigation into the chamber of the tooth. Subsequently, the microcannula (see Fig. 9 B) is inserted to the working length; irrigation is again added to the pulp chamber. The irrigation is then suctioned down the canal, through the holes in the microcannula, causing an apical negative pressure (ANP).
A study by Shin and colleagues reported that the EndoVac left significantly less debris behind than conventional needle irrigation methods. ANP removed more debris from narrow isthmi in mandibular mesial roots than manual dynamic irrigation in a closed system. The EndoVac is adept at penetrating NaOCl to the working length in a closed system, and produces less extrusion than needle irrigation. The use of ANP has a significant reduction of postoperative pain levels compared with conventional needle irrigation.
A study by Miller and Baumgartner showed that although there were fewer colony-forming units of Enterococcus faecalis bacteria when using the EndoVac, it was not statistically different than a 30-gauge side-vented needle. A study by Brito and colleagues compared NaviTip needles (Ultradent, South Jordan, UT, USA), EndoActivator, and the EndoVac system. The study concluded no evident antibacterial superiority with any technique used.
Light-activated Disinfection
Light-activated disinfection (LAD) is also known as photodynamic antimicrobial chemotherapy, photodynamic therapy, and photo-activated disinfection in the literature. The photosensitizer can be toluidine blue dye, methylene blue dye, and perfluorodecahydronaphthalene combined with methylene blue dye. Nanoparticle-based endodontic therapy using poly(lactic-co-glycolic acid) (PLGA) nanoparticles loaded with methylene blue are reported in the literature. The photosensitizer binds to the surface of a microorganism. After light activation the photosensitizer absorbs the light, which affects the oxygen present. The oxygen molecule is split into a reactive oxygen specimen that destroys microbial cell walls and other structures. The light source is usually a laser, white light, red light, or a light-emitting diode. Bacterial growth modes play a vital role in influencing the susceptibility to LAD in a dose-dependent manner. The nature of the photosensitizer formulation influences the susceptibility of biofilms to LAD.
The treatment is to fully instrument and irrigate the canal system. The canal is then filled with a photosensitizer and then illuminated with a light source. The root canal is then dried and obturated. The only commercially available unit is the FotoSan (CMS Dental Aps, Copenhagen, Denmark) ( Fig. 10 ). Although the unit is not available in the United States, it may serve as an adjunct in a multistep irrigation and disinfection protocol in the future.
Computed Tomography-guided Endodontic Surgery
Dr Stephen Buchanan demonstrated computed tomography (CT)-guided endodontic surgery in the San Diego Convention Center for the American Association of Endodontists annual meeting in April 2010. Using the treatment planning software Simplant R (Materialise Dental, Glen Burnie, MD, USA) and a surgical stent, Dr Buchanan performed a precise osteotomy and apicoectomy ( Fig. 11 ).