3.1 Soft-Tissue Management at Implant Placement
From the biological point of view, the apicocoronal positioning of an implant, particularly those of tissue-level design, should follow the principle of “as shallow as possible, as deep as necessary” (Buser and coworkers 2004) in order to avoid deep peri-implant probing depths, taking into account the prosthetic and esthetic factors in the area.
This concept has recently been confirmed in a case-control study on 19 patients that evaluated the modifying effect of a deep mucosal tunnel (DMT, ≥ 3 mm) on the induction and resolution phases of experimental peri-implant mucositis (Chan and coworkers 2019). All patients, each with a properly placed tissue-level implant, were assigned either to the test group (DMT, depth ≥ 3 mm) or to the control group (shallow mucosal tunnel, SMT, ≤ 1 mm). The subjects underwent a standard experimental peri-implant mucositis protocol, characterized by an oral-hygiene optimization phase, a three-week induction phase using an acrylic stent to prevent self-performed oral hygiene at the experimental implant, and a three-plus-two-week resolution phase.
The modified plaque index (mPI), gingival index (mGI), and IL-1β concentrations in the peri-implant sulcus fluid were determined over time. Both the mPI and the mGI increased during the induction phase. After normal oral hygiene had resumed, the mPI and mGI resolved towards baseline values in the SMT group, while they diverged in the DMT group. Although plaque accumulation was resolved in the DMT group, the resolution of inflammation was delayed and found to be of smaller magnitude during the first three weeks after resumption of oral hygiene. IL-1β Concentrations were significantly higher in the DMT group at the end of induction and during the resolution phase, corroborating the clinical findings. Removal of the crown and submucosal professional cleaning were needed to revert mGI to baseline values in the DMT group.
The fact that the depth of the peri-implant sulcus influenced the resolution of experimental mucositis raised doubts as to the efficacy of self-performed oral hygiene in scenarios where implants are placed too deeply. Therefore, since the risk of mucositis evolving into peri-implantitis appears to be higher in such clinical situations, clinicians should make every effort to place implants properly—not only for esthetic, but also for biological reasons (Berglundh and coworkers 2018).
It should be noted that, from a clinical point of view, this may be more easily achievable for implants without adjacent teeth, but more challenging if the implant has to be placed between two teeth, particularly if these teeth are periodontally compromised. Figures 1a-b show examples of correct implant positioning. Figures 2a-b show examples of incorrect implant positioning.

Fig 1a The implant was carefully selected and positioned in a periodontally compromised patient so as to present minimal probing depth (time of crown cementation).

Fig 1b Healthy interdental papilla between two tissue-level implants, after removing seven-year-old single ceramic crowns which had been kept in place with provisional cement.

Fig 2a The distal implant was placed at the level of the bone crest without considering the thickness of the soft tissue, resulting in a deep mucosal tunnel.

Fig 2b Residual resin-based cement around the distal Wide Neck Implant. The deep mucosal tunnel does not allow complete removal of the excess cement. Screw-retained restorations would have been preferable in both cases.
The ideal implant position for optimal soft-tissue integration should be planned before removing the teeth. Ridge preservation is one of the treatment options after tooth extraction, particularly in situations where one or more socket walls are missing (Roccuzzo and coworkers 2014c; Mardas and coworkers 2015). The rationale for this approach is that the maintenance of the ridge contour often facilitates subsequent treatment steps and limits the risk of an improper position of the implant collar, creating an ideal soft-tissue seal (MacBeth and coworkers 2017). Figures 3a-i show an example of long-term soft-tissue stability after implant placement following ridge preservation. The correct positioning of an implant, with a shallow peri-implant sulcus, could be particularly difficult in areas where the mucosa is too thick. Here an appropriate flap design is mandatory, especially if cemented restorations are planned. Figures 4a-h show an example of implant positioning in the posterior maxilla where a tissue excess needed to be removed.

Fig 3a Radiograph of a first molar with a severe endo-perio lesion. A large post-extraction bone defect with reduced bone levels near the adjacent teeth was anticipated, and therefore ridge preservation was planned.

Fig 3b After tooth extraction and careful removal of inflamed epithelium around the socket border, the marginal mucosa appeared mobile due to the lack of buccal bone.

Fig 3c Deproteinized bovine bone mineral (DBBM) with 10% collagen (Bio-Oss Collagen; Geistlich, Wolhusen, Switzerland) was inserted to fill the decontaminated socket and covered with a double layer of collagen membrane (Bio-Gide; Geistlich) secured with 4-0 Vicryl (Ethicon; Johnson & Johnson International) resorbable sutures.

Fig 3d After eight weeks of healing, a thick band of keratinized mucosa was visible.

Fig 3e After four months, the dimensions of the ridge were adequate to insert a fixture in the proper position, with no need for further augmentation.

Fig 3f A chemically modified titanium implant was placed (S, WNI SLActive, diameter 4.8 mm, length 12 mm; Institut Straumann AG, Basel, Switzerland).

Fig 3g The soft tissues were circumferentially adapted around the smooth collar of the implant for ideal non- submerged suturing.

Fig 3h Three months after placement, the implant was surrounded by a firm collar of keratinized tissue.

Fig 3i Good stability of the peri-implant soft tissues seven years after placement despite some buccal recession on the adjacent natural premolar.

Fig 4a Part of a panoramic radiograph. Large cyst in the maxillary left sinus. After consultation with an ENT surgeon, who did not suggest any specific treatment, it was decided to place implants without interfering with the sinus.
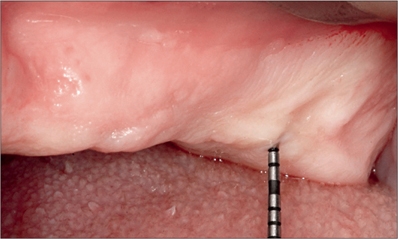
Fig 4b The left posterior maxilla. The probe used for bone sounding indicated the presence of very thick mucosa in the area of the second molar.

Fig 4c Primary incision lines.

Fig 4d Left posterior maxilla after removal of the excess tissue, which was later used as a graft in the anterior area.

Fig 4e Titanium implant at site 27 with a chemically modified surface (S, WNI SLActive, diameter 4.8 mm, length 10 mm; Institut Straumann AG). The standard implant with a 2.8-mm smooth collar was considered ideal for bringing the margin of the restoration to a more coronal level.

Fig 4f Intraoperative view following the placement of implant 24 (SP, WNI SLActive, diameter 4.1 mm, length 12 mm; Institut Straumann AG). The implant with a 1.8-mm collar was selected to reduce the risk of future soft-tissue dehiscences. The bone concavity on the buccal aspect of the mesial implant is a risk factor for dehiscence.

Fig 4g Autologous bone chips on the buccal aspect of the implant. The connective-tissue graft taken from the posterior area was adapted to protect the bone chips and to increase the width of the crest.

Fig 4h Semi-submerged healing in the anterior grafted area; non-submerged healing with close adaptation of the flap around the collar of the distal implant.

Fig 4i Optimal adaptation of the soft tissues around both implants six weeks after implant placement.

Fig 4j Solid abutments, 4 mm in height, connected eight weeks after implant placement.

Fig 4k Four-unit cemented metal-ceramic bridge in situ.

Fig 4l One-year follow up. Healthy peri-implant soft tissues with minimal probing depth (< 4 mm) and no bleeding after removing the provisionally cemented ceramic bridge.

Fig 4m Radiograph at the five-year follow-up. Stable interproximal bone levels.
One of the challenges in optimal flap design around non-submerged implants is the circumferential closure around the implant collar, especially when the soft tissues present anatomical irregularities. Figures 5a-k show an example of soft-tissue management for non-submerged tissue-level implants in the posterior maxilla with an irregular soft-tissue morphology.

Fig 5a Preoperative situation.

Fig 5b Incision placed slightly palatally to move keratinized tissue onto the buccal side.

Fig 5c Two wide-neck implants placed at sites 26 and 27 (SP, WNI SLActive, diameter 4.8 mm, length 10 mm; Institut Straumann AG).

Fig 5d Incision on the distal portion of the palatal flap.

Fig 5e The pedicle flap was rotated counterclockwise.

Fig 5f Pedicle inserted between the two implants.

Fig 5g The pedicle was adapted with a 4-0 Vicryl vertical mattress suture between the 2 implants.

Fig 5h Final suture, distally to the distal implant.

Fig 5i Preoperative occlusal view.

Fig 5j Postoperative occlusal view.

Fig 5k Periapical radiograph at eighteen months after implant placement. Favorable interproximal bone levels.
Creating an optimal flap for ideal transmucosal healing becomes even more difficult if no keratinized mucosa is present at all. In these circumstances, a free gingival graft may be advised, especially if bone regeneration is required, as discussed in Chapter 4.1.
Often, a small quantity of keratinized tissue will be sufficient to create a soft-tissue cuff around the implant collar, provided the tissue is properly surgically managed. Figures 6a–I show an example of soft-tissue management around a tissue-level implant in conjunction with bone regeneration in a case where there does not appear to be any keratinized tissue available.

Fig 6a Preoperative view of site 46, at the end of orthodontic treatment. Limited crestal width and no keratinized mucosa.


Fig 6b-c Once the implant was placed (S, SLA, diameter 4.1 mm, length 12 mm; Institut Straumann AG), the dehiscence on the facial bone was covered with autologous bone and a DBBM graft.

Fig 6d Resorbable collagen membrane prepared with a punched hole, placed over the graft, and secured with a healing cap.


Fig 6e-f
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


