Exploit Growth to Obtain Predictable Orthopedic Correction
One of the most intriguing subjects in orthodontics is the growth and development of the maxillofacial complex. During the last 40 years, knowledge and understanding of this subject have changed greatly. Today it is clear that under certain circumstances, particular forces can be used to affect or control growth of the maxillofacial complex with excellent results. In orthodontic treatment, the affected areas include the maxilla, the mandible, and the dentoalveolar complex.
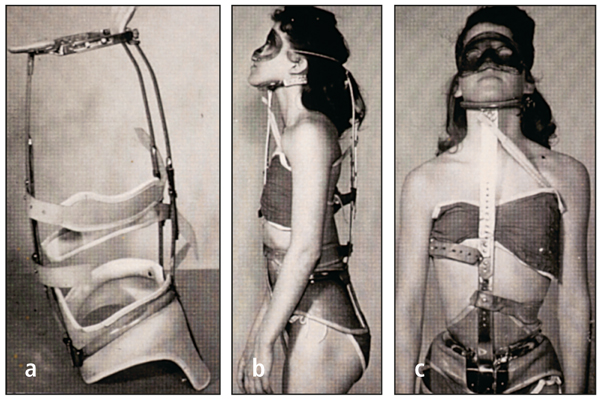
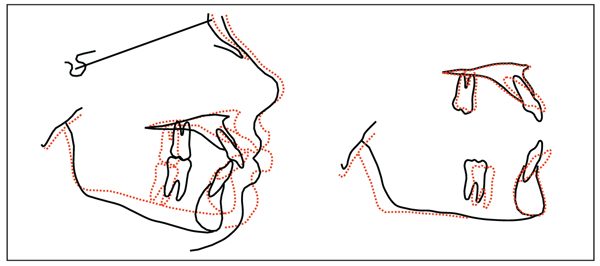
I first discovered this possibility in graduate school when studying the effects of scoliosis treatment with the Milwaukee brace on tooth position and maxillofacial growth. Dr Fred Schudy (Fig 8-1) provided valuable counsel as I attempted to interpret the findings of this study. For the first time in orthodontic literature,1 it was concluded that force applied to the mandible (through the Milwaukee brace) “demonstrates a directional change of growth in the lower face of a growing child” (Fig 8-2). The occlusal forces created by the brace flared the maxillary and mandibular incisors and depressed the molars. These forces also depressed the total anterior facial height (Fig 8-3).
Fig 8-1 Dr Fred Schudy, who shared his understanding of growth and development, had considerable influence on the author’s professional life.
The good news from this study was that maxillofacial growth can be altered. However, it is impossible, in orthodontic treatment, to create the same force levels as those achieved by patients wearing the Milwaukee brace, because the brace was worn almost 24 hours a day. The challenge, then, was to find a way to apply this new found knowledge to treating the abnormal skeletal patterns of orthodontic patients.
For orthopedic forces to have an opportunity to control or change growth, a patient must have the potential for significant growth. In general, a good rule to follow is that females grow earlier and males grow later. Therefore, early treatment in the mixed dentition is usually more successful with females. If possible, delayed treatment in males is preferred. Several methods to determine growth potential have been used; hand-wrist radiographs and cervical vertebrae radiographs are useful but tend to be less reliable in the borderline stages, when it is not known if the patient has any growth left. The old-fashioned method of observing the size of the parents and siblings and talking with parents about the growth potential of their child may be as good indicators as other approaches.
Possibilities for Growth
Transverse dimension
Growth takes place in three planes of space: transverse, vertical, and sagittal. Of the three directions, the transverse dimension is the most predictable. A narrow maxilla in a growing child can usually be expanded with rapid palatal expansion and have predictable and stable results. This is considered an orthopedic correction. Similar changes of less magnitude can be achieved with expanded archwires. In nongrowing patients, nonsurgical palatal expansion is also possible, although the long-term stability is less certain.
To a lesser extent, a narrow mandibular dental arch can be expanded with controlled stability, usually with a lip bumper or other functional appliance. This would be considered dentoalveolar expansion. Orthopedic expansion of the mandible is not possible without surgery.
Sagittal dimension
The maxilla is a very malleable bone. The forward growth of the maxilla can be controlled effectively by the use of orthopedic appliances, such as a facebow or other functional appliances. As shown in many studies, growth of the maxilla is actually inhibited while the mandible continues to grow to reach its genetic potential.1–3 In addition, in a skeletal Class III patient, the maxilla can be advanced slightly by the use of a face mask.
There are few if any appliances that can be used to affect mandibular growth. The claim that certain appliances can “grow” mandibles beyond their genetic potential lacks long-term evidence.4
The debate among orthodontists is whether it is possible to “stimulate” the growth of the mandible, as claimed by advocates of certain functional appliances. The reality, based on many studies and clinical experience, is that no type of orthopedic force can stimulate mandibular growth.2 The mandible has a certain potential genetic growth that will express itself if given the opportunity. This opportunity is accomplished by unlocking the mandible when growth has been inhibited as a result of malocclusion. To be able to grow the mandible beyond its genetic potential is just wishful thinking. Perhaps one day, genetic research will allow the stimulation of growth of the mandible, but it will require a different approach from the orthopedic appliances used today.
Vertical dimension
The vertical dimension is decidedly the most difficult skeletal pattern to change. The Milwaukee brace study1 indicated that it is possible to permanently decrease the mandibular angle if the force is severe enough. The reality is that such force and time requirements (24 hours per day) are not realistic for a patient to achieve. If the patient has a vertical skeletal pattern, it is extremely difficult to do anything more than control this pattern, to prevent it from worsening. This in itself is a clinical challenge.
Treatment of high-angle cases is accomplished with the use of a high-pull facebow and extractions, in some cases. Muscle “squeezing” exercises may also help, though to a lesser degree. With these treatments, if followed conscientiously, the high-angle pattern can be controlled.4
With the advent of miniscrews (temporary bony implants), a continuous intrusive force may be achievable. This could actually cause a reduction in vertical dimensions. Additional well-controlled studies are needed to confirm this possibility.
Orthopedic Diagnosis and Treatment Planning
The orthodontist can assemble certain facts to address orthopedic problems by studying the cephalometric tracing to determine the skeletal pattern and by measuring the intermolar width and occlusion on the study casts. Depending on the findings, specific orthopedic appliances can be used to address the skeletal discrepancies.
In orthodontic treatment of growing children, however, it must be realized that the patient is a “moving target.” The amount of growth that takes place during treatment can play an important role in the success of the treatment. Evaluating the amount of growth potential a patient has is an erratic science at best (see principle 2).
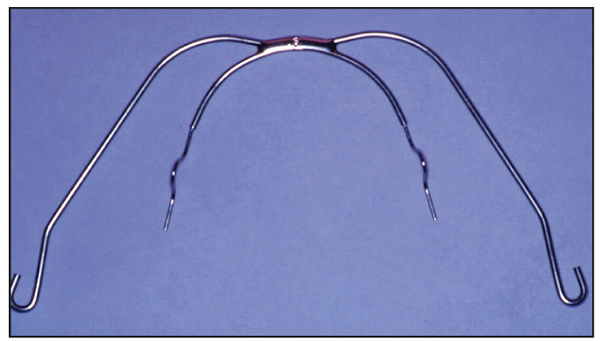
The facebow, utilized for the orthopedic correction of Class II skeletal patterns, has produced the best, most consistent, and most stable results. This appliance can be utilized as a cervical-pull, combination-pull, or high-pull appliance, all of which apply specific force vectors to the maxilla. The active force of the facebow is applied, via the maxillary first molars, to the maxillary-dental complex with archwires that are tied back. The great advantage of the facebow is that the opposing force is applied to the back of the neck or head, rather than to the mandibular anterior teeth, as is necessary with functional appliances. Therefore, the negative secondary reaction to most other devices, the flaring of mandibular incisors, is not produced by this extraoral orthopedic force.
Of equal importance to the success of the treatment is a patient’s ability to follow instructions. The patient must be educated to believe in the treatment and motivated to follow the instructions given by the orthodontist. Compliance is discussed further in principle 20.
The following sections describe the appliances used to obtain predictable orthopedic correction for various skeletal problems.
Correction of Class II Skeletal Patterns
A clarification of terminology is in order. In the Alexander Discipline, headgear effect is defined as inhibiting forward maxillary growth while allowing forward mandibular growth. No tipping, distalizing, or extrusion of the maxillary molars is caused by the facebow because these potential deleterious side effects are controlled by the maxillary archwire, which has omega loops and is tied back at the molar tubes.
In the following discussion on the applications and use of extraoral traction, the term facebow will be used to describe the use of a specific extraoral appliance with a cervical traction strap or an occipital traction strap attached. In the Alexander Discipline, a facebow or a face mask is used primarily to exert orthopedic forces. These forces are exerted on consolidated, tied-back archwires in growing patients. If the archwires are not tied back, the forces are changed to orthodontic forces, resulting in tipping, extrusion, and/or distal movement of the maxillary first molars.
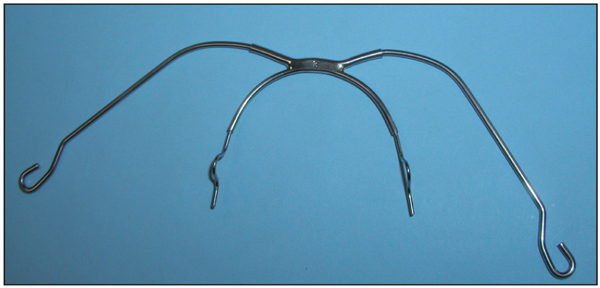
The facebow (Fig 8-4) is the appliance of choice for the correction of Class II skeletal malocclusions because it can affect growth in all three dimensions: control of sagittal growth requires cervical-pull headgear; in patients with vertical growth patterns a high-pull vector is used; and the transverse dimension can be controlled and improved by inner facebow adjustments. In addition, as mentioned previously, the reciprocal force is applied to the back of the neck or head, thus eliminating the negative reaction on the mandibular anterior teeth.
The keys to success in facebow therapy include proper adjustment of the facebow and the direction and amount of force, along with patient growth and compliance (number of hours worn).
Direction of pull
If the mandibular plane angle (sella-nasion–mandibular plane) is less than 36 degrees, the directional pull is cervical (see Fig 5-3). If the mandibular plane angle is 36 to 42 degrees, the directional pull is combination (see Fig 5-5). If the mandibular plane angle is greater than 42 degrees, the directional pull is high (see Fig 5-7).
Amount of force
The initial force is 8 oz (227 g). Subsequently, a force of 16 oz (454 g) is applied.
Hours worn
If point A–nasion–point B (ANB) is less than 3 degrees, the patient is instructed to wear the facebow for 8 hours daily (nighttime only). If ANB is from 3 to 5 degrees, the patient is instructed to wear the facebow 10 hours per day. If ANB is greater than 5 degrees, the patient is instructed to wear the facebow 12 hours per day.
Facebow adjustments
To achieve success with facebow treatment, this appliance must be adjusted properly.
Transverse adjustment
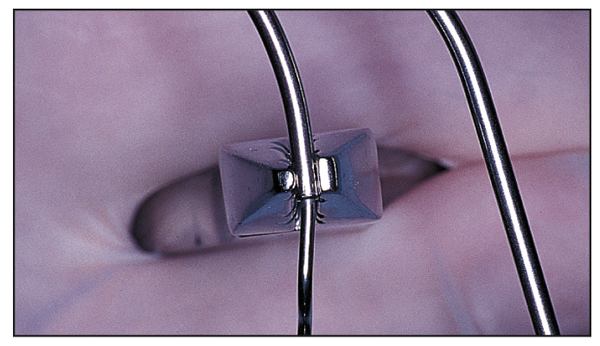
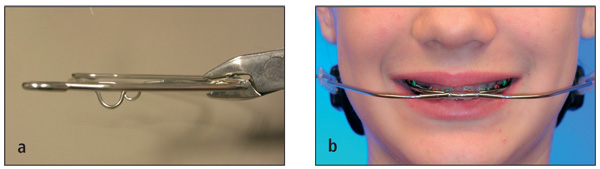
In the transverse dimension, an inner bow expansion of approximately 4 mm should be maintained (Figs 8-5 and 8-6).
Molar rotation
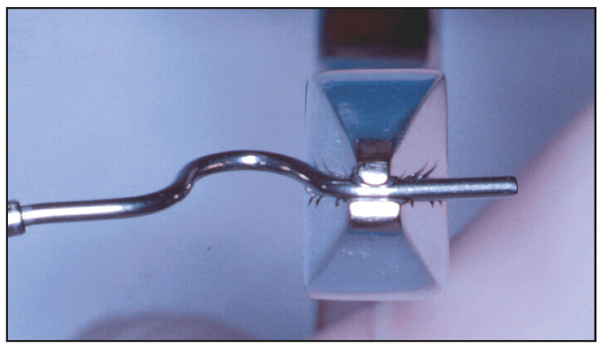
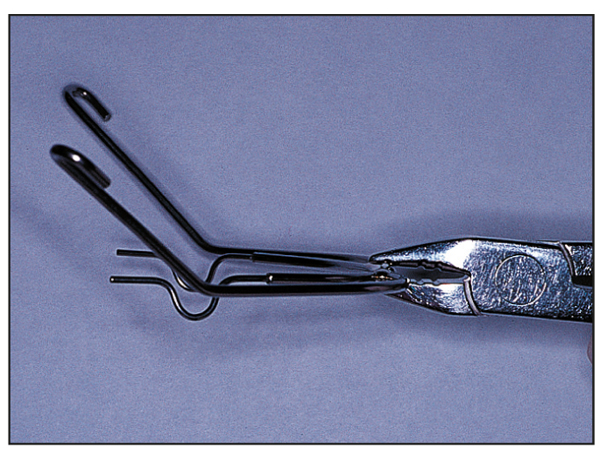
The distal end of the inner bow, the portion entering into the headgear tube, must be adjusted to insert passively into the headgear tube. As the molars rotate, this adjustment must be repeated at each appointment (Fig 8-7).
Sagittal adjustment
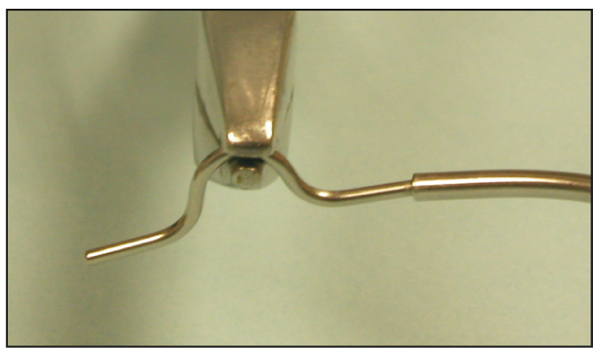
The anteroposterior position of the inner bow–outer bow connection is just anterior to the lips at rest (Fig 8-8). This positioning is accomplished by enlarging or constricting the adjustment loop on the inner bow (Fig 8-9).
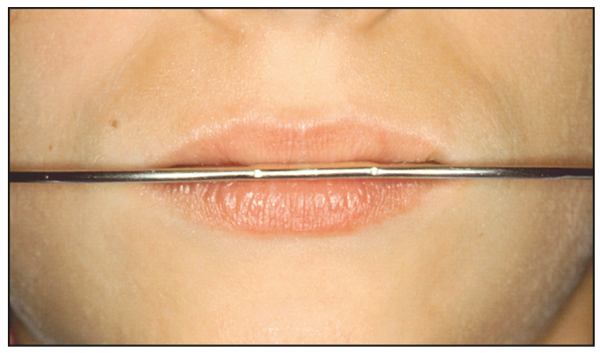
Fig 8-8 The connection of the inner bow–outer bow should be positioned just beyond the lips closure and balanced between the upper and lower lips.
Fig 8-9 The position of the inner bow–outer bow connection can be changed by expanding or constricting the adjustment loop.
Vertical adjustment
Vertically, the facebow is positioned at the center of the lips (see Fig 8-8). This is accomplished by bending the inner bow wire, where it enters the headgear tube, either up or down as necessary (see Fig 8-6). After the facebow is attached, the vertical position of the facebow should not change. Any significant rotation of the outer bow when connected to the strap indicates that a rotational moment is being applied.
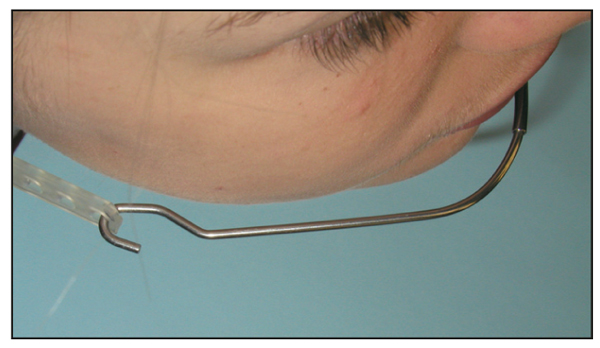
It is very important that the outer bow is parallel to the inner bow and parallel to the occlusal plane (Fig 8-10). If the force is directed in this manner, the vertical dimension will be controlled. The outer bows are adjusted so that they will be just lateral to the cheeks when the extraoral force is applied (Fig 8-11).
Figs 8-10a and 8-10b Vertical growth can be controlled by keeping the outer bow parallel to the occlusal plane.
Although this is only an intuitive statement, I believe that the outer bows of the facebow force the patient to sleep on the back of their head rather than on the side of their face. This allows the mandible to grow without the application of any abnormal forces, thus encouraging symmetric growth (Fig 8-12).
Fig 8-12 The outer bow forces the patient to sleep on the back of the head because it would press against the cheek if the patient slept on the side of the face. Since most growth takes place at night, the facebow facilitates more symmetrical mandibular growth.
Molar vertical control
In a high-angle case, it is critical that the facebow have no extrusive force on the molars. This is accomplished by raising the outer bow 20 to 45 degrees above the inner bow. The point of attachment of the headgear to the outer bow should be aligned with the first molars (Fig 8-13). The degree to which the outer bow is raised is determined by the severity of the skeletal angle. The extraoral force will then be exerted by a high-pull strap.
Fig 8-13 For high-angle Class II cases, the outer bows are bent at a 20- to 40-degree angle. This bend is placed parallel to the maxillary first molars.
Unilateral adjustment
In asymmetric occlusions (Class II subdivision), the facebow can be adjusted in the following manner. On the Class II side, the outer bow is bent outward, away from the face (Fig 8-14). The stop on the inner bow on the Class II side is lengthened. When the headgear is attached to the outer bow, more force is generated to the Class II side.
Fig 8-14 In asymmetric occlusions, the outer bow can be expanded, and the inner bow can be lengthened on the Class II side. This places more force on the Class II side to help correct the asymmetry.
It has been my experience that a regular facebow (without any adjustments) can work well in correcting minor and moderate asymmetries. More discussion of asymmetry is presented in principle 15.
Compliance
The only major alteration in the information thus far presented is in the time necessary to wear the facebow. On the day the patient’s appliances are removed, the tradition in our office is to have a celebration with the patient and parents. At this time, the results are discussed, instructions for retainer wear and maintenance are given, and the patient is praised for a job well done. When the Class II skeletal pattern has been beautifully corrected, I will always ask the patient, “Please tell me the truth, because whatever you did, it worked. How much did you really wear your facebow?” I have heard the following answer many, many times, and it has allowed me to change my thinking and instructions to the patient: “I did not wear it as much as you told me, but my parents made me sleep in it every night!”
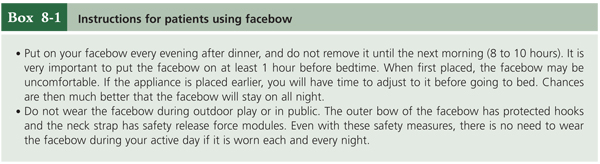
Those comments are significant in three ways. First, they expose the role parents play in the success of the treatment. Second, even severe Class II skeletal patterns were corrected with only nighttime wear. Third, usage had to be consistent. “Every night.” The clinical reality is that if the patient will consistently sleep in the facebow—and grow— the Class II skeletal pattern will be corrected within 6 to 12 months. Typical instructions for facebow patients are shown in Box 8-1. As a reward for consistent wear, the patient may have one “free night” every 2 weeks. Principle 20 delves further into this critical and important matter of compliance.
Research on facebow
Very significant knowledge has emerged in the past few years from research involving facebow patients from my office. Romine,6 Plunk,7 Glenn et al,8 and Elms et al9,10 have all studied the effects and stability of facebow correction in growing patients. These studies have changed clinical results from anecdotal observations to evidence-based facts:
- The results of nonextraction therapy for patients with Class II malocclusions can be relatively stable when the orthodontist ensures proper patient selection and compliance and attains the treatment objectives.
- Overall stability is relatively good.
- Arch length and intercanine width decrease postretention.
- Changes in overjet, overbite, and intermolar width remain stable following treatment.
Correction of Class III Skeletal Patterns
The original Alexander Discipline textbook11 devoted very little time to discussion of Class III and transverse skeletal problems. Today, each of these problems is encountered (or recognized) more often. Therefore, individual chapters are presented in a future volume to focus on the treatment of skeletal Class III and transverse problems. Only a brief overview is presented here.
In our practice, almost all growing, Class III patients are treated with a face mask. The elastics are attached to the anterior area of the maxillary arch (Fig 8-15), usually on the ball hooks present on the maxillary lateral brackets. It is imperative that the archwire be tied />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses