Surgical management of upper third molars in general is less complex compared to lower third molars. They cause less discomfort, are more likely to erupt, and are simpler to remove unless unerupted and encased in bone. Removal of upper third molars results in far less postoperative morbidity, and general anesthetics are rarely required.
1 The commonest type of impaction in maxillary third molar is vertical (Peterson et al, 2003).1
Classification of impacted maxillary third molars: The system of classification of upper wisdom tooth is essentially same as that for impacted mandibular third molar. Nevertheless, there are some additional parameters to be considered which will aid in preoperative assessment of the case and guide in planning the surgery for a successful outcome.
1. State of Eruption
1. Fully erupted
2. Partially erupted
2. Angulation of the Tooth (Figs 10.1 to 10.3)
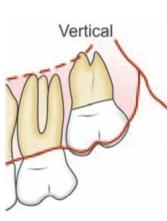
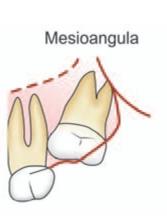
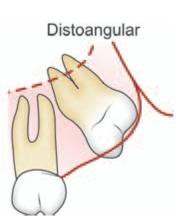
Fig. 10.1: Classification of impacted maxillary third molar based on angulation

Fig. 10.2: Periapical X-ray showing mesioangularly impacted 38
1.Vertical-63%
2.-25%Mesioangular
3.Distoangular-12%
4.Laterally displaced with the crown facing the cheek, horizontal, inverted and transverse positions- less than 1%
5.Aberrant position sometimes associated with pathological condition such as cyst
3. Pell and Gregory Classification
This is based on the relative depth of the impacted maxillary third molar (Fig.10.4).
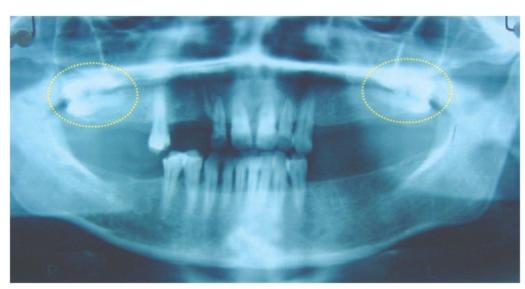
Fig. 10.3: OPG showing horizontally impacted maxillary third molars (yellow oval)
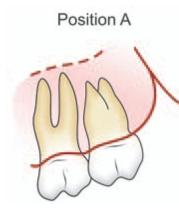
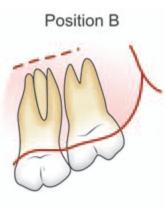
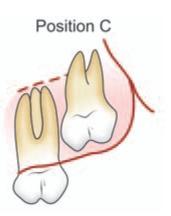
Fig. 10.4: Pell and Gregory classification based on relative depth of impacted maxillary third molar
PositionAOcclusal surface of third molar is at the same level as that of second molar.
PositionBOcclusal surface of third molar is located between occlusal plane and cervical line of second molar.
PositionCOcclusal surface of third molar is at or above the cervical line of second molar.
4. Relationship of Impacted Maxillary Third Molar to the Maxillary Sinus
1. Sinus approximation (SA): No bone or a thin partition of bone between the impacted maxillary third molar and maxillary sinus.
2. No sinus approximation (NSA): 2 mm or more bone between the impacted maxillary third molar and maxillary sinus.
5. Nature of Roots
1. Fused (conical )
2. Multiple-Favorable/Unfavorable
Indications for the Removal of Maxillary Third Molar
1.Extensive dental caries which is beyond restoration and causing food stagnation
2. Recurrent pericoronitis
3. Buccally or distally erupting tooth causing the patient to adopt a bite of convenience to avoid cheek biting. (Adopting such a bite of convenience leads to temporomandibular joint pain in certain cases)
4. Tooth involved in pathological process such as cyst.
5. Over erupted and non functional upper third molarWhen the opposing mandibular third molar has been removed, the maxillary third molar tends to over erupt leading to food impaction between the latter and second molar (Fig.10.5). This in turn leads to periodontal problems and dental caries of maxillary second and third molar.
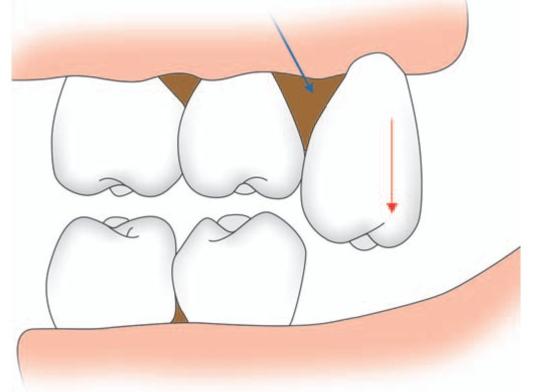
Fig. 10.5: Schematic diagram showing over erupted upper third molar (red arrow) leading to food impaction (blue arrow) between second and third molar tooth
Additionally because of over eruption, the upper third molar impinges on the edentulous lower third molar area upon closure of the mouth and causes ulceration (Fig.10.6).
6. Buccally erupting upper third molar impinging on the coronoid process during mandibular movements leads to pain during movement. Furthermore traumatic ulceration and hyperkeratosis of the buccal mucosa also can occur due to constant irritation.
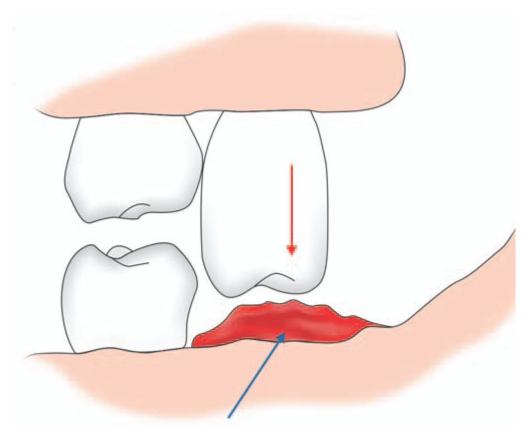
Fig. 10.6: Schematic diagram showing over erupted upper third molar (red arrow) impinging in lower third molar area causing ulceration (blue arrow)
7. Interference with placement of prosthesis-Erupting upper third molar will interfere with placement of a denture causing pain and/or retention problem. Hence they have to be removed.
Local Contraindications for Removal
1. Symptom-less upper third molar completely embedded in bone.
2. Upper third molar positioned high in the alveolussurgical removal of such teeth carry the risk of displacing the tooth into the maxillary antrum or infratemporal fossa.
3. Deeply impacted tooth, the removal of which may damage the adjacent second molar.
It has been observed that an impacted upper third molar tooth may begin to erupt and eventually reach the surface making its removal easy.
Radiographic Examination
The following are the useful radiographs-
1.Periapical X-ray
2.Orthopantomogram (OPG)
3.Occlusal X-ray
4.True lateral view-occasionally helpful
5.PNS view of maxilla-if associated pathology like cyst or tumor is suspected
6.CT scan-especially if associated pathology like cyst or tumor is suspected.
Bouquet et al (2004)2 reported that CT scan gives better qualitative and quantitative information compared to panoramic radiograph in the pre operative evaluation of impacted maxillary third molars. The CT scan was more precise than the panoramic radiograph for measurement of the level of impaction of the third molar, measurement of the third molar displacement, bone height separating the third molar roots and the sinus, and for assessing the length of roots in the sinus. The CT scan was equally accurate for measurement of the distance separating the crowns of second and third molars (Figs 10.7A to D).

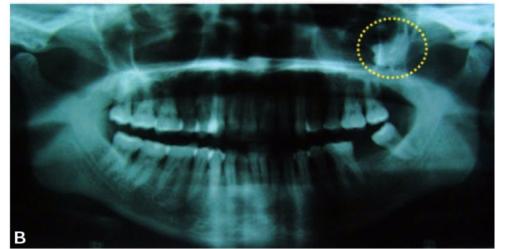
Figs 103A and B: (A) Impacted left maxillary third molar not visible in the periapical X-ray, (B) OPG of the same patient showing impacted 28 placed high in the tuberosity region of the maxilla (yellow circle)


Figs 10.7C and D: (C) Axial CT scan of the patient showing impacted 28 (yellow circle), (D) Coronal CT scan of the patient showing impacted 28 (yellow circle)
Determining the Degree of Difficulty of Removal
1. Angulation: While considering the angulation and degree of difficulty of removal vis – a- vis mandibular third molar, it has been found that the same angulations in mandibular third molar cause opposite degree of difficulty for maxillary third molar extraction. For example in case of maxillary third molars, vertical and distoangular impactions are easiest to remove, while mesioangular impactions are more difficult, i.e. exactly the opposite of mandibular third molars. Mesioangular impactions in maxillary third molar are more difficult to remove because the bone that is overlying the tooth which must be removed is on the posterior part of the tooth and is comparatively dense than in vertical or distoangular impaction. Moreover, accessibility is also less for a tooth in mesioangular position.
2. Position in buccoangular direction: This also contributes to determining the degree of difficulty of removal. Generally crown of maxillary third molars are directed towards the buccal aspect of the alveolar process. This makes the overlying bone thin and easy to expand. In such cases, a definite bulge can be felt on the buccal aspect. Rarely, the impacted maxillary third molar is positioned towards the palatal aspect of the alveolar process. This necessitates removal of more bone to gain access and thereby increases the difficulty of removal. When the crown is directed palatally, a bony deficit may be palpated on the buccal aspect of alveolar process. Digital palpation followed by radiographic examination will help to determine the buccopalatal position of maxillary third molar.
3. Type of overlying tissues or Degree of eruption: Similar to mandibular molars; tooth which has only soft tissue covering is easier to remove than complete bony impaction.
4. Proximity to maxillary sinus: Frequently the impacted maxillary molar is in close approximation to the floor or posterior wall of the maxillary sinus. Removal of such tooth may result in oro-antral communication or displacement of the tooth into the sinus. Necessary steps should be taken to prevent this.
5. Proximity to maxillary tuberosity: Because of proximity of impacted tooth to tuberosity, it can be fractured during extraction of impacted maxillary third molar. Factors contributing to this hazard are:
•Dense and non-elastic bone as in old age
•Multirooted tooth with large bulbous roots
•Large maxillary sinus expanded to include the roots of third molar
•Use of excessive force to elevate the tooth which has divergent roots.
•Mesioangular impactions where the tuberosity is frequently heavier and surrounding bone thinner.
6. Other factors influencing the degree of surgical difficulty : These factors are similar to that of impacted mandibular third molar. Morphology of the tooth especially that of the root plays a vital role in this regard.
•Tooth with roots which are thin, separated and with curvature are difficult to extract. Fortunately majority of maxillary third molars have fused conical roots.
•Hypercementosis of roots make removal difficult.
•Tooth with a wide periodontal space is easier to extract. When periodontal space decreases as in old age, surgical removal is difficult
•Tooth with a wide follicular space is easier to remove than with no follicular space.
•Bone when it is less dense and more elastic as in young patients makes extraction easier. While in old age when bone becomes denser and less elastic removal of tooth is more complicated.
•Close relationship of a deeply impacted tooth to adjacent second molar makes the removal difficult, since more bone should be removed to avoid damage to second molar.
•Fusion of third molar with roots of second molar makes removal difficult.
•Presence of large restoration on second molar requires the judicious use of elevator to luxate the impacted tooth.
•Difficult access due to small oral aperture or trismus complicates the removal.
Surgical Anatomy
a.Maxillary tuberosity: The impacted maxillary third molar is located in the tuberosity. It is surrounded by cancellous bone and a thin buccal cortical plate comparable to an egg shell. The palatal cortical plate is thick and dense. Such an anatomy dictates that the upper third molar should be removed by a buccal approach.
b.Mucoperiosteum: The buccal and distal side of the tuberosity is covered by mucoperiosteum of normal thickness in which is found branches of posterior alveolar artery and vein. On the palatal aspect, the tuberosity is covered by thick mucoperiosteum containing greater palatine neurovascular bundle. This is located at the junction between the alveolar process and horizontal part of maxilla.
c.Maxillary sinus: Impacted maxillary molar is located close to the floor of the maxillary sinus. Very often there will be only a thin plate of bone separating the floor of the sinus from the third molar root (Fig.10.8). In rare instances, this thin plate of bone may be absent and the root of third molar may protrude into the maxillary sinus. Similarly, the extension of maxillary sinus and its floor into the tuberosity area also varies. The close proximity of third molar root increases the possibility of accidentally pushing the third molar or its root into the maxillary sinus. The extension of sinus into the tuberosity weakens this area leading to accidental fracture of maxillary tuberosity while luxating a firmly fixed upper third molar.
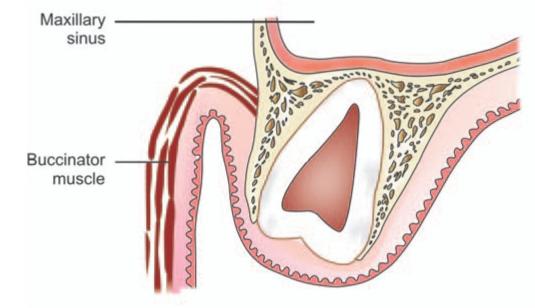
Fig. 10.8: Schematic diagram showing the relationship of impacted maxillary third molar to the floor of the maxillary sinus
d.Muscles: On the buccal side the buccinator muscle is inserted on the lateral aspect of the tuberosity above the molar teeth. The exact position of the attachment of buccinator muscle in relation to molar roots has a surgical implication with regard to spread of infection from the molar either to the buccal vestibule or into the buccal space.
The inferior head of the lateral pterygoid muscle originates from the outer surface of the lateral pterygoid plate, which is located immediately behind the tuberosity area. Damage to this muscle will lead to postoperative trismus.
e.Buccal pad of fat: This is present between the buccinator and masseter muscle. During surgery, accidental perforation of the buccinator muscle by surgical blade or retractor may result in prolapse of the buccal fat pad into the operative field. Sudden visualization of a yellowish material will be distressing for the operator. No attempt is made to remove the prolapsed fat by pulling it out. If this is attempted more fat will come out. Instead, that part of fat maybe resected or pushed back and a suture given.
f.Pterygopalatine fossa: This narrow space is located posterior to the maxillary tuberosity and the pterygoid process forms the posterior boundary. The fossa is limited medially by the vertical plate of palatine bone. Laterally, this fossa communicates with the infratemporal fossa. Excessive pressure exerted in a posterior direction during elevation of an impacted maxillary third molar may cause its displacement into the pterygopalatine fossa.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses