Armamentarium
|
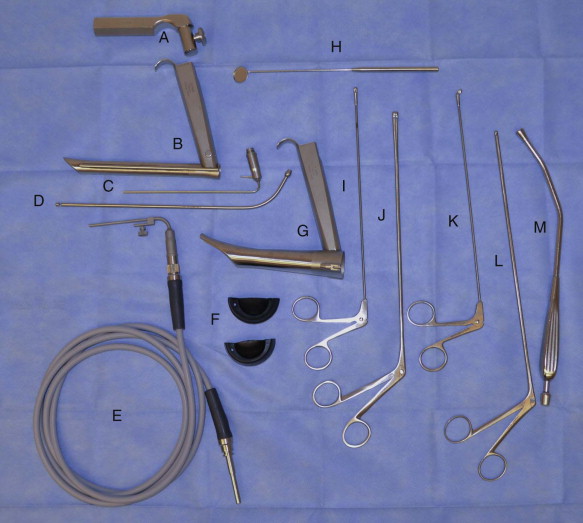
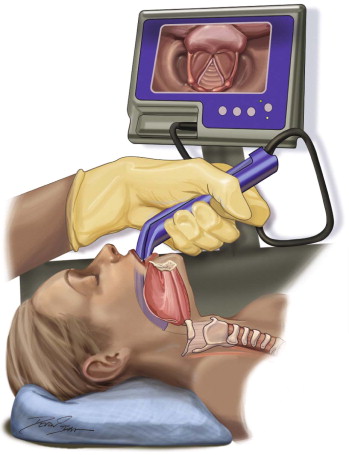
| Direct Laryngoscopy ( Figures 96-1 and 96-2 ) |
|
|
| Rigid Bronchoscopy |
|
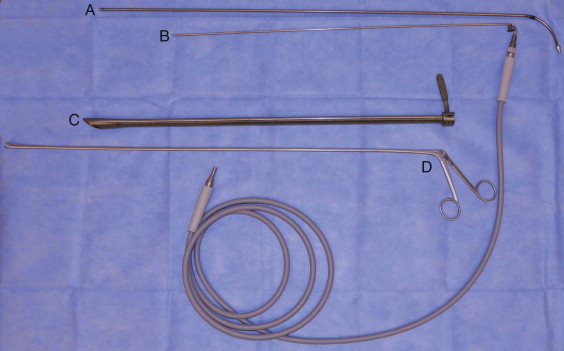
| Flexible Bronchoscopy ( Figure 96-3 ) |
|
| Esophagoscopy ( Figure 96-4 ) |
|

History of the Procedure
Using a wax candle as a light source, in 1806, Bozzini used a combination of an angled speculum with a mirror insert to examine multiple cavities of the body, including the larynx. In 1829, Babbington reported on the use of the glottiscope, a three-blade device consisting of a stainless steel mirror and tongue retractors. In 1853, the “father of endoscopy,” Desmoreaux, improved upon Bozzini’s endoscope by attaching a gaslight and condenser to project a beam of light down the tube.
At around the same time, Garcia developed a separate device consisting of a dental mirror, a hand mirror, and sunlight to visualize his own pharynx. Turck, Czermak, and then MacKenzie are all credited for refining techniques in endoscopy. Killian developed an apparatus for suspending the laryngoscope using a headlight. In1897, he used a rigid endoscope to examine the airways and reported the first incidence of removing a foreign body from the bronchial tree without performing tracheostomy. Chevalier Jackson made major refinements to endoscopy in the early 1900s by inventing distal lighting for endoscopic equipment, developing a variety of endoscopic instruments and, along with Brunings of Germany, advocating the use of magnification in endoscopy. The Zeiss operating microscope, developed in the 1950s along with laryngoscope development by Jako, led to increased quality of binocular magnification.
Interestingly, optimal patient positioning in endoscopy was actually derived from physicians’ work with sword swallowers. Desmoreaux, after assessing the technique of sword swallowers, was able to look into the stomach using a 47-cm tube; this technique, however was never published. Leiter, an instrument maker, in collaboration with Kussmaul and Johann von Mikulicz-Radecki, fabricated a light source for straight tube esophagoscopy. As von Mikulicz described it in his 1881 publication, Zur Technik der Gastroskopie und Oesophagoskopie, the two crucial moments during sword swallowing occur during passage of the sword through the upper and lower esophageal sphincters. Sword swallowers cannot change position (as is the case for patients undergoing esophagoscopy) and therefore must optimize the position of the proximal esophagus by displacing the lower jaw, hyoid bone, and tongue base anteriorly.
The flexible fiberoptic bronchoscope was introduced by Shigeto Ikeda in the 1960s. At approximately the same time, Hopkins developed a rod lens telescope that modified the ridged endoscope by adding angled and wide-angled lens. More modern endoscopic instruments are able to capture pictures and video.
History of the Procedure
Using a wax candle as a light source, in 1806, Bozzini used a combination of an angled speculum with a mirror insert to examine multiple cavities of the body, including the larynx. In 1829, Babbington reported on the use of the glottiscope, a three-blade device consisting of a stainless steel mirror and tongue retractors. In 1853, the “father of endoscopy,” Desmoreaux, improved upon Bozzini’s endoscope by attaching a gaslight and condenser to project a beam of light down the tube.
At around the same time, Garcia developed a separate device consisting of a dental mirror, a hand mirror, and sunlight to visualize his own pharynx. Turck, Czermak, and then MacKenzie are all credited for refining techniques in endoscopy. Killian developed an apparatus for suspending the laryngoscope using a headlight. In1897, he used a rigid endoscope to examine the airways and reported the first incidence of removing a foreign body from the bronchial tree without performing tracheostomy. Chevalier Jackson made major refinements to endoscopy in the early 1900s by inventing distal lighting for endoscopic equipment, developing a variety of endoscopic instruments and, along with Brunings of Germany, advocating the use of magnification in endoscopy. The Zeiss operating microscope, developed in the 1950s along with laryngoscope development by Jako, led to increased quality of binocular magnification.
Interestingly, optimal patient positioning in endoscopy was actually derived from physicians’ work with sword swallowers. Desmoreaux, after assessing the technique of sword swallowers, was able to look into the stomach using a 47-cm tube; this technique, however was never published. Leiter, an instrument maker, in collaboration with Kussmaul and Johann von Mikulicz-Radecki, fabricated a light source for straight tube esophagoscopy. As von Mikulicz described it in his 1881 publication, Zur Technik der Gastroskopie und Oesophagoskopie, the two crucial moments during sword swallowing occur during passage of the sword through the upper and lower esophageal sphincters. Sword swallowers cannot change position (as is the case for patients undergoing esophagoscopy) and therefore must optimize the position of the proximal esophagus by displacing the lower jaw, hyoid bone, and tongue base anteriorly.
The flexible fiberoptic bronchoscope was introduced by Shigeto Ikeda in the 1960s. At approximately the same time, Hopkins developed a rod lens telescope that modified the ridged endoscope by adding angled and wide-angled lens. More modern endoscopic instruments are able to capture pictures and video.
Indications for the Use of the Procedure
Panendoscopy for head and neck surgery, which includes direct laryngoscopy, esophagoscopy, and bronchoscopy, was classically considered an essential part of the workup for malignancies of the head and neck region. The theory behind panendoscopy in the initial evaluation or follow-up for malignancies of the head and neck is that if a patient develops malignancy in those regions, he or she is at increased risk for lesions of other areas of the aerodigestive tract. Lesions that are identified as a second malignancy, are distinct and geographically separated by normal nonneoplastic mucosa, and are not of metastatic origin are defined as synchronous tumors. These lesions must be identified at the time of initial tumor evaluation. Lesions discovered at some point in the future, after discovery of the primary lesion, are defined as metachronous tumors. The reported rate of synchronous cancers varies from 1.5% to 18%. Although panendoscopy has been the gold standard, some have questioned its economic and therapeutic effectiveness compared to contemporary techniques such as standard computed tomography (CT) and F-FDG PET/CT. Davidson et al. reported that the rate of synchronous tumors found in patients undergoing direct laryngoscopy, bronchoscopy, and esophagoscopy was 2.6% for pulmonary lesions, 1.3% for head and neck mucosal lesions, and 0% for esophageal lesions. Newer technologies, such as virtual three-dimensional F-FDG PET/CT 18 , have been reported as an alternative to bronchoscopy for evaluating pharyngeal and laryngeal malignancies. In a study comparing panendoscopy to 18 F-FDG PET/CT, the prevalence of tumors detected was 4.5% by panendoscopy versus 6.1% by 18 F-FDG PET/CT. However, given the lower specificity and the cost of 18 F-FDG PET/CT, panendoscopy is endorsed by many as a reliable method of investigation for secondary primary tumors and for follow-up screening.
Attempts at direct laryngoscopy should be performed to obtain a general sense of the aerodigestive tract. If available, preoperative imaging should be reviewed to examine the precise location of any radiographically appreciable lesions. Consent for tracheostomy should be considered in patients with a tenuous airway. Although it may be performed under local anesthesia, endoscopy is usually performed under general anesthesia. Chevalier Jackson noted: “Endoscopic ability cannot be bought with the instruments. As with all mechanical procedures, facility can be obtained only by educating the eye and the fingers in repeated exercise of a particular series of maneuvers. As with learning to play a musical instrument, a fundamental knowledge of technique, positions, and landmarks is necessary, after which only continued manual practice makes for proficiency.” Panendoscopy should be methodical, effective, and efficient, and all three skills are brought about by repetition.
Direct Laryngoscopy
In the patient with head and neck tumors, direct laryngoscopy may be used to identify and biopsy lesions of the pharynx and larynx. Suspicion of malignancy combined with symptoms such as chronic hoarseness, dyspnea, dysarthria, globus sensation, chronic dysphagia, pharyngitis, odynophagia, odynophonia, chronic choking episodes, chronic cough, and voice changes should be further investigated with direct laryngoscopy. (Other uses for direct laryngoscopy, such as drainage or removal of laryngeal scars, strictures, synechiae, or webs; procedures on the vocal cords; and exploration in patients with neurologic disease, are not discussed here.) Limited laryngoscopy can be performed in the office. For more accurate visualization of the airway and biopsy, the examination should be performed under general anesthesia in the operating room.
In the office, laryngoscopy can be performed using a 70- or 90-degree rigid telescope. Patient positioning is similar to that for indirect mirror laryngoscopy. However, this technique limits the speech sounds that can be elicited, especially in children. The stroboscope, initially developed by Oertel in 1878, emits rapid pulses of light at a preset rate. This rate is usually synchronized with the vocal frequency of the patient during phonation. The stroboscope usually is used along with a rigid or fiberoptic endoscope and video recording device and a microphone, which is placed over the lateral neck to measure the acoustics of the patient’s voice. The frequency of the light pulse is compared with the patient’s vocal frequency; when they are synchronized, the image appears static. Deviations from this and changes in the true vocal cord vibratory pattern may reveal vocal cord pathology that could not otherwise be visualized. Another examination performed by speech pathologists is fiberoptic endoscopic evaluation of swallowing (FEES). This may be used along with videofluoroscopic examination for patients with dysphagia or aspiration.
Bronchoscopy
In the patient with head and neck cancer, bronchoscopy is most commonly used for staging of malignancy and follow-up. Bronchoscopy can also be therapeutic, as in the case of obstruction by retained secretions (the details of this are not discussed here). The literature suggests an additional yield of bronchoscopy over chest radiography of less than 1% in identifying synchronous tumors. However, the role of bronchoscopy in the presence of a normal thoracic CT scan has been questioned. Bronchoscopes are either rigid or flexible. In general, the large, open lumen of a rigid bronchoscope is useful for retrieving foreign bodies or for performing therapeutic maneuvers such as electrocautery. Flexible bronchoscopes contain a fiberoptic lighting and viewing system that can display images on an attached eyepiece or external monitor. Flexible bronchoscopy also offers the advantage of digital photography. Fiberoptic bronchoscopes can be inserted farther toward the periphery of the bronchial tree than can rigid bronchoscopes, especially in the upper lobes. Davidson et al. found no difference in the ability to find synchronous lesions between patients undergoing rigid bronchoscopy and those undergoing flexible bronchoscopy.
Esophagoscopy
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


