This case report describes the successful orthodontic tooth movement through the maxillary sinus in an adult patient. A 41-year-old Asian woman had severe lip protrusion and multiple missing posterior teeth. Her orthodontic treatment included the extraction of 2 teeth, maximum retraction of the incisors using the extraction spaces and the existing spaces from the missing molars, and closure of all remaining spaces. Even though the treatment time was extended because of the anatomic and biologic challenges associated with moving posterior teeth over a long distance through the maxillary sinus, a successful outcome was obtained, with significant bone modeling of the maxillary sinus. The results demonstrate that a carefully selected force system can overcome the anatomic limitations of moving tooth against the cortical bone of the maxillary sinus wall in adult patients.
With increased demand for adult orthodontics, orthodontists are often faced with the challenge of correcting occlusal problems that are related to anatomic limits, such as atrophy of the alveolar process, extension of the maxillary sinus into the alveolar process, and periodontally compromised supporting tissues. These anatomic limitations are attributed to cortical bone. Moving teeth through cortical bone is difficult in adults because it increases treatment complexity and treatment time. However, previous investigators and clinicians have demonstrated successful tooth movement “with bone” into the compromised bone by applying a carefully planned force system that resulted in bodily movement with frontal bone resorption, rather than indirect bone resorption. Among dental professionals, this approach has been well established as a method to generate new bone for implant placement. In addition, a maxillary sinus lift procedure is commonly recommended for implant placement when the maxillary sinus extends into the alveolar process because of the loss of maxillary posterior teeth. Moving teeth through the maxillary sinus is considered one of the most challenging problems in orthodontics, since it requires compensatory new bone apposition, before bone resorption, in the direction of tooth movement to maintain the integrity of the sinus wall. In addition, unknown side effects, such as root resorption, pulp vitality, and perforation of the sinus membrane, can cause additional complications. Thus far, few reports are available in the literature.
This case report presents the possibility of moving teeth over a long distance through the maxillary sinus to close posterior edentulous spaces. In addition, it demonstrates the generation of new bone after tooth movement, which, in turn, contributed to changes in the configuration of the maxillary sinus and the maxillary tuberosity region.
Diagnosis and etiology
A 41-year-old Asian woman came to the graduate orthodontic clinic, Arthur A. Dugoni School of Dentistry, University of the Pacific, in San Francisco, with a chief complaint of lip protrusion and difficulty in lip closure. She had no significant past medical history but had a moderately restored maxillary dentition with several missing molars. She received regular periodontal checkups, and her oral hygiene was well maintained.
The pretreatment facial photographs showed a convex profile and upper and lower lip protrusion with lip incompetence upon closure. Although a slight maxillary occlusal cant and a slight facial asymmetry were observed, the facial midline and dental midlines were coincident ( Fig 1 ). Intraorally, the patient had normal overjet and overbite (4 and 3 mm, respectively), a Class II canine relationship bilaterally, a lingual crossbite, and a significant supraeruption of the maxillary right first molar because of the missing opposing mandibular right first molar ( Fig 2 ). Loss of the mandibular right first molar also resulted in the mandibular right second molar’s being mesially tipped and the mandibular right second premolar’s being distally displaced toward the missing first molar space, which left about 6 mm of space. The loss of the maxillary left first and second molars resulted in a space of 16 mm, into which the maxillary left third molar was slightly mesially tipped. A moderate curve of Spee in the mandibular arch was observed.


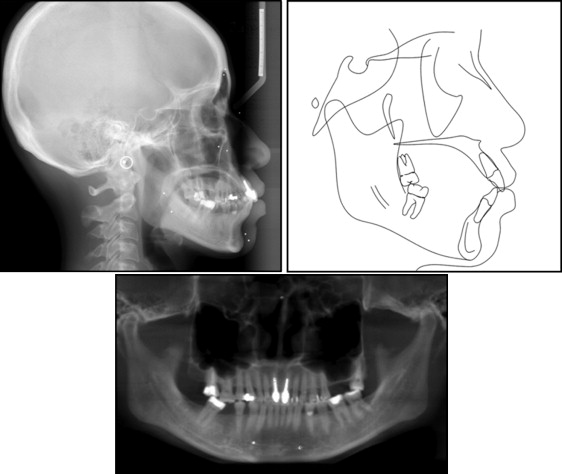
Figure 3 shows the pretreatment lateral cephalometric and panoramic views from the cone-beam computed tomography (CBCT) images. They showed that the dentition was moderately restored, including root canal treatments on the maxillary central incisors and the maxillary right second molar. The lateral cephalometric tracing and analysis ( Table ) demonstrated normal anteroposterior (ANB, 2°) and vertical (normodivergency; MP-SN, 28°; FMA, 21°) relationships relative to the cranial base with severe proclination of the maxillary and the mandibular incisors (U1-NA, 11 mm; U1-SN, 111°; L1-NB, 10 mm; IMPA, 101°) and lip protrusion beyond the E-line (upper lip, 1 mm; lower lip, 4 mm). The interincisal angle was 120°, and the nasolabial angle was less than 90°. Based on the cephalometric measurements, the patient was diagnosed as having a normal skeletal pattern with severe bimaxillary protrusion. Sagittal and coronal slices of the CBCT image showed that the floor of the maxillary sinus on the left side extended significantly toward the top of the alveolar crest, leaving only 1 mm of cortical bone in the edentulous space where the first and second molars were missing ( Fig 4 ). The distal surface of the maxillary second premolar and the mesial surface of the third molar were directly contacting the cortical bone of the maxillary sinus wall. In addition, the maxillary left third molar had 3 roots that were unusually well developed, including a buccolingually wide mesial root that is more typical of mandibular molars ( Fig 4 , C ).
| Pretreatment | Posttreatment | Norm | |
|---|---|---|---|
| Skeletal | |||
| SNA (°) | 87 | 87.6 | 81 ± 4.0 |
| SNB (°) | 84.8 | 83.4 | 77.7 ± 3.4 |
| SNP(°) | 85.1 | 84.7 | 79.8 ± 4.1 |
| ANB (°) | 2.3 | 4.2 | 2.9 ± 2.7 |
| MP-SN (°) | 28.3 | 28.5 | 32.1 ± 5.5 |
| FMA (MP-FH) (°) | 20.8 | 20.1 | 23.9 ± 4.5 |
| Dental | |||
| U1-SN (°) | 111.1 | 89 | 102.8 ± 5.5 |
| U1-NA (°) | 24.1 | 1.4 | 22.8 ± 5.7 |
| U1-NA (mm) | 10.6 | −0.3 | 4.3 ± 2.7 |
| L1-NB (°) | 33.6 | 19.4 | 25.3 ± 6.0 |
| L1-NB (mm) | 10.4 | 2.8 | 4 ± 1.8 |
| IMPA (L1-MP) (°) | 100.5 | 87.6 | 90 ± 7.0 |
| FMIA (L1-FH) (°) | 58.8 | 72.4 | 64.8 ± 8.5 |
| Interincisal angle (U1-L1) (°) | 120.1 | 155 | 130 ± 6.0 |
| Soft tissue | |||
| Upper lip to E-plane (mm) | 0.7 | −2.8 | −6 ± 2.0 |
| Lower lip to E-plane (mm) | 4.2 | −1.4 | −2 ± 2.0 |
| Nasolabial angle (°) | 86 | 104.6 | 102 ± 8.0 |
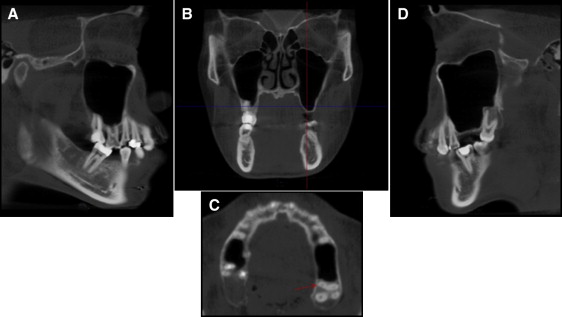
The floor of the maxillary sinus on the right side also extended into the roots of the posterior teeth, especially at the supraerupted first molar ( Fig 4 , A ). The temporomandibular joint was asymptomatic, and radiographic evidence showed no abnormalities.
The patient reported a family history of lip protrusion. The etiology of the bimaxillary protrusion appeared to be primarily hereditary.
Treatment objectives
The treatment objectives for this patient were to (1) improve her facial profile and eliminate her lip incompetence through maximum retraction of the maxillary and mandibular incisors into the existing spaces and the extraction spaces (maxillary right first molar and mandibular left first premolar); (2) close the remaining space with protraction of the maxillary left third molar and the mandibular right second molar after using the spaces needed for incisor retraction; (3) obtain normal overjet and overbite; and (4) achieve ideal Class I canine relationships with good buccal occlusion.
Treatment objectives
The treatment objectives for this patient were to (1) improve her facial profile and eliminate her lip incompetence through maximum retraction of the maxillary and mandibular incisors into the existing spaces and the extraction spaces (maxillary right first molar and mandibular left first premolar); (2) close the remaining space with protraction of the maxillary left third molar and the mandibular right second molar after using the spaces needed for incisor retraction; (3) obtain normal overjet and overbite; and (4) achieve ideal Class I canine relationships with good buccal occlusion.
Treatment alternatives
A combined orthodontic and restorative plan was presented as the preferred treatment option. This involved extracting all first premolars, except the maxillary left premolar because of the 2 missing molars, and retracting the anterior segments to reduce the lip protrusion. The remaining spaces would be restored with dental implants to replace the mandibular right first molar and the maxillary left molar, which would also require a maxillary sinus-floor augmentation. However, the patient declined the maxillary sinus lift procedure and implant option because of the surgical risks and high costs.
An orthodontic-only approach with miniscrews to close all remaining spaces without dental restorations was also discussed. To reduce lip protrusion, maximum distal movement of the maxillary premolars and anterior teeth would be necessary. This option required extractions in the maxillary right and mandibular left quadrants, and also using the existing spaces in the maxillary left and mandibular right quadrants. Although the need for restorations was eliminated, a significantly longer orthodontic treatment time was expected, since the space from the 2 missing molars was about 16 mm. Moreover, because the maxillary sinus extended into the top of the alveolar crest in the missing molar space and the cortical bone of the sinus wall directly contacted the mesial surface of the unusually large mesial root of the third molar, protraction mechanics would require careful planning and accurate execution of force systems to achieve bodily tooth movement with bone ( Fig 4 ).
With mesial movement of the third molar and distal movement of the second premolar, modeling of the maxillary sinus wall (new bone on the wall of the maxillary sinus) must occur before bone resorption. Despite knowing that it would be a long treatment time, the patient still accepted the orthodontic treatment-only option to close all spaces. Therefore, extractions of the first premolars in the maxillary right and the mandibular left quadrants for retraction of the incisors were considered inevitable. A large amalgam filling also provided a practical reason for extracting the maxillary right first premolar. However, extraction of the first molar in the maxillary right quadrant was discussed because the alveolar bone level was above its furcation due to supraeruption ( Fig 4 , A ). After considering the feasibility of intrusion and the prognosis of the periodontal status, we decided to extract the first molar in the maxillary right quadrant.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


