Fig. 18.1
Patient with mandible fractures treated with MMF
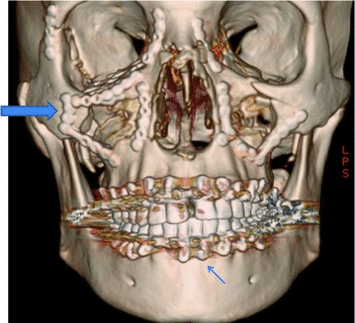
Fig. 18.2
Patient with extensive panfacial fractures. Titanium plates and screws (large arrow) and MMF (small arrow) can be appreciated
Orthognathic Surgery and Nutrition
Orthognathic surgery is usually electively performed to establish optimal form and function in patients presenting with dental and skeletal deformities resulting in facial distortions and dental malocclusions. As a result of their malocclusion, patients often have severe difficulty biting and chewing (Fig. 18.3). In conjunction with orthodontic therapy, maxillary and mandibular osteotomies can address these facial anomalies. Surgery is typically performed in an operating room setting under general anesthesia, requiring 2–6 hours of operative treatment and may result in substantial blood loss. In addition to a possible period of postoperative MMF ranging from 2–6 weeks, significant discomfort and swelling may impede dietary intake for a prolonged period.


Fig. 18.3
Patient with severe dentofacial deformity and anterior open bite. This type of malocclusion is associated with difficulty masticating
Following surgery, a clear liquid diet for one meal is followed by progression to a full liquid diet that can be consumed through a straw for the first several days postoperatively. The progression of the diet consistency from liquid to solids is determined by the oral surgeon [6]. Adequate calories and nutrients are critical for wound healing and to maintain nutritional well-being. Oral nutritional supplements addressed in Section “Oral Diets and Nutrition Supplementation” and Table 18.2 of this chapter can be used to help patients meet energy and nutrient needs while on a consistency modified diet (the Appendix has a sample consistency modified diet). Within a week, patients usually progress to a mechanical soft diet using foods of a puree-like or finely chopped consistency such as mashed potatoes, soft pastas, chopped and moistened grains, meats, fish, poultry, beans along dairy products, and peeled and chopped or pureed fruits and vegetables [6].
Kendell reviewed patients’ (aged 4–14 years old) nutritional status and conducted dietary analyses following orthognathic surgery accompanied by 6 weeks of MMF [7]. Patients taking a liquid nutritional supplement (Ensure Plus®, Abbott Laboratories, Chicago, IL) in addition to a blenderized diet were able to maintain a caloric intake similar to preoperative levels as opposed to the control group. In addition, the oral supplementation resulted in decreased weight loss postoperatively [7]. Patients undergoing orthognathic surgery and a prolonged course of MMF (6 weeks) also lost approximately 9.7% of their body weight [8]. Similar results were noted in a 2009 study by Kim, and all that showed an average body postoperative weight loss of 6.4% (5–10 lbs.) [9]. Kim et al. found that it took 5–10 weeks postoperatively for patients’ weight to return to preoperative levels; the postoperative weight gain was facilitated by the improved masticatory function that the majority of patients experienced (84.1%). The application of titanium miniplates and screws to fixate osteotomies or fractures has shown to reduce the dependence on MMF to provide proper immobilization for bone healing. This technique may allow for an earlier return to the patient’s regular diet which helps decrease postoperative weight loss [10].
Feeding Issues in Patients with Cleft Lip and Palate
Patients with cleft lip and palate may have difficulties feeding due to their inability to efficiently seal the oropharynx during sucking [11] (Figs. 18.4 and 18.5). This usually results in nasopharyngeal regurgitation and air ingestion, which can lead to inefficient feedings [12] and significant growth disturbances during the first 12 months. In newborns with these craniofacial anomalies, proper nutrition is critical as cleft lip surgical repair is usually delayed until the infant is at least 10 weeks old, 10 lbs., and have a hemoglobin of 10 g/dL (“rule of 10”). Modified nipples (i.e., Haberman Feeder®) and a compressible bottle have been recommended to facilitate feedings. In addition, holding the infant more erect may decrease nasal regurgitation [12]. Following cleft lip repair, the infant is encouraged to suckle as much as possible to strengthen the newly reapproximated orbicularis oris muscle of the lip (Fig. 18.6). Following cleft palate, palate repair at the age of 10–12 months is usually recommended to feed the toddler with a spoon or a syringe for approximately 4-weeks to decrease trauma to the sutures (Figs. 18.6 and 18.7).

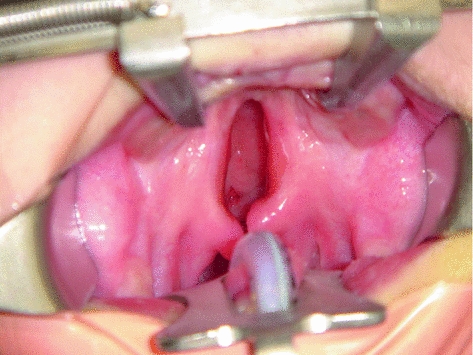

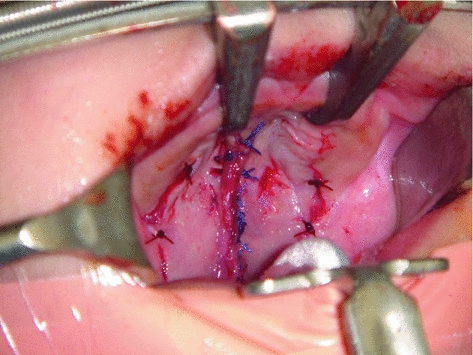

Fig. 18.4
Infant with unrepaired bilateral cleft lip
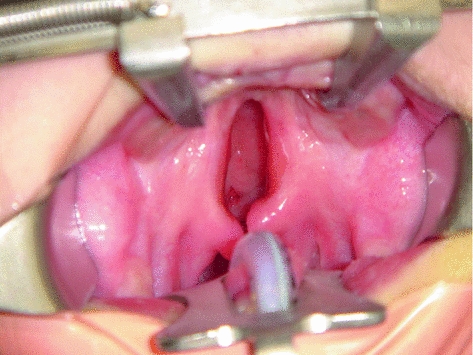
Fig. 18.5
Toddler with large hard and soft palate cleft. The nasal cavity can be seen through the cleft

Fig. 18.6
Patient in Fig. 18.4, following repair of the cleft lip
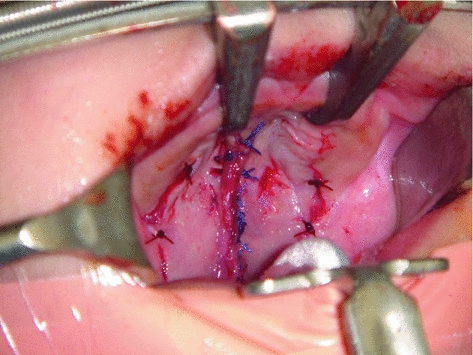
Fig. 18.7
Patient in Fig. 18.5 following cleft palate repair
Nutrition Support
Nutrition is an important component of the healing process. The National Institute for Health and Care Excellence (NICE) guidelines recommend implementation of nutrition support for individuals with malnutrition, as defined by a BMI of less than 18.5, weight loss of at least 10% in the last 3–6 months, or a BMI of less than 20 with a 5% unintentional weight loss in the last 3–6 months [13]. General indications for nutrition support are addressed in Table 18.1. Nutrition support therapies include diet with oral nutritional supplements, enteral nutrition (tube feedings), and parenteral nutrition (PN). In individuals undergoing oral maxillofacial surgery, the oral and tube feeding routes are most often used for nutrition support when needed. Tube feedings should be reserved for those individuals who cannot meet energy and nutrient needs by diet alone with or without malnutrition. Oral nutrition supplements either as a liquid or a powder that must be reconstituted are defined as medical foods [14]. Most of these products are available to consumers in pharmacies and supermarkets without a Licensed Independent Practitioner (LIP) prescription. Selection of the appropriate formula for either oral or tube feeding use though should be done under the direction of a RD and LIP who will help ensure that the patient receives appropriate, cost-effective, and practical nutrition support.
|
Little to no nutrition × 5 days or more and expected to not eat well for 5 or more days
|
|
Unintentional weight loss >10% in <6 months
|
|
BMI < 18.5
|
|
BMI < 20 and unintentional weight loss of >5% in <6 months
|
|
Not expected to meet nutritional needs orally due to high nutrient losses, hypermetabolism, or hypercatabolism
|
Figure 18.8 is a decision tree that can be used to determine whether patients need nutrition support and the ideal route of administration. A tube feeding is indicated in individuals following oral or dental surgery who cannot meet their energy and nutrient needs orally to promote wound healing and prevent malnutrition and in those with malnutrition to promote healing and restore nutritional well-being. Preoperative nutrition support may be indicated in patients with preexisting malnutrition; during the immediate postoperative period, these patients may also need oral supplementation and/or enteral tube feeding to maintain their nutrition status [15, 16]. OHCPs can refer patients who are unable to meet their nutrient needs orally to a RD for medical nutrition therapy (MNT). As part of the MNT, the RD will conduct a comprehensive nutrition assessment, determine nutrition diagnoses, energy and nutrient needs along with a route of feeding. In consultation with the oral healthcare professional and patient, the RD will set diet and nutrition goals. Feeding progression is determined by the oral surgeon.
Fig. 18.8
Route of feeding decision tree [20]
The gastrointestinal (GI) tract is the preferred site for nutrient delivery. An oral diet with or without oral nutrition supplements is the preferred route of feeding. PN is only indicated when the GI tract cannot be used [15, 16]. This may be due to a bowel obstruction, prolonged ileus, inability to achieve enteral access [17]. Referral to an RD and physician with nutrition support expertise is recommended to ensure clinically appropriate, safe, cost-effective methods of nutrition support are delivered.
Oral Diets and Nutrition Supplementation
Oral surgery may impact motor and sensory functions of the oral cavity. The location and extent of surgery tend to dictate the individual’s ability to open their mouth, bite, chew, and swallow and subsequent diet form (whole, cut, chopped, puree or liquid) and nutrient intake. Individuals with limited oral opening or difficulty biting and chewing should first try a consistency modified diet. Depending on the extent of the limitations, cut or chopped fruits (and peeled) and vegetables, moistened and cut/chopped protein foods, and other harder to bite/chew foods may be tolerated. When necessary, broths, gravies, and sauces can be used to moisten foods. Use of mechanically chopped or pureed foods should be reserved for those who cannot tolerate any of the previously mentioned approaches. Visual appeal as well as taste and smell are important components of food preparation and presentation that can influence appetite and subsequently intake. Small, frequent meals and consistency modified diets can be helpful to maintain adequate calorie, protein, and total nutrient intake. When nutrition supplementation or support is warranted based on the algorithm in Fig. 18.7, liquid oral nutrition supplements should be considered in patients who can safely swallow [13]. The goal for supplementation should include a balanced mixture of protein, energy, fiber, electrolytes, vitamins and minerals to meet individual energy and nutrient needs and maximize wound healing.
Table 18.2 describes oral supplements and tube feeding products available commercially. Choice of formula usually depends on the patient’s taste preferences, cost, and whether a complete meal replacement is needed. Most oral liquid nutritional supplements are meal replacement formulas, meaning their energy and nutrient composition mimics that of a meal; the volume of formula however depends on the individual’s nutritional needs. Many of these products are available in several forms, typically regular (1 kcal/mL), high protein and high calorie (1.5–2.0 kcal/mL). They can be used to supplement total calories and protein for patients who are otherwise eating a variety of foods and/or can be considered total meal replacements for those who are unable to meet 100% of energy and nutrient needs without supplementation. Specialized liquid oral supplements marketed toward patients with diabetes or other health conditions are available, but consultation should be made with a RD prior to recommending these supplements.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


