Chapter 8
Non-surgical and Surgical Re-treatment
Introduction
Endodontic treatment has a high success rate (Ng et al, 2011); however, on occasion treatment may fail. Several factors have been reported to contribute to the failure of endodontically treated teeth (Siqueira, 2001; Ng et al, 2007; Azim et al, 2015).
The management of failed root canal treatment is dependant on the mode of failure, which may be multi-factorial (Fig 8-1). Treatment options commonly include non-surgical endodontic re-treatment, surgical re-treatment, extraction, and no treatment. Other less-frequent treatment options include root amputation and intentional implantation.
An effective treatment plan can only be devised when firstly, the diagnosis, and secondly the reason behind treatment failure have been determined. This chapter will explore how the data obtained by cone beam computed tomography (CBCT) may influence clinical decision making and the overall treatment planning in managing failed endodontically treated teeth (Fig 8-1).
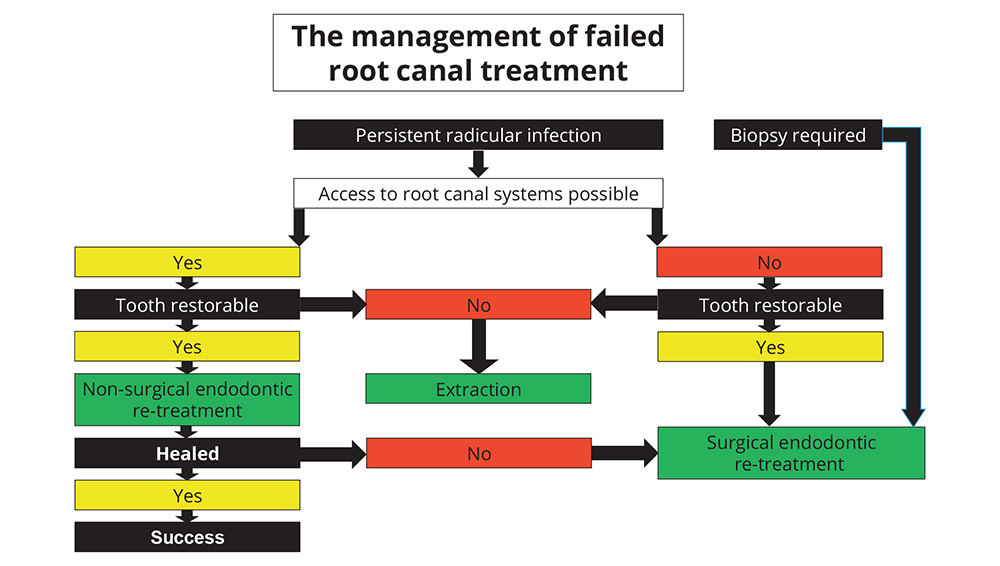
Fig 8-1 Factors involved in clinical decision making in relation to the management of failed root canal treatment. Green boxes indicate the treatment plan. Note that the ability of the clinician to gain access to the root canal systems is at the heart of the decision tree and non-surgical endodontic re-treatment should be attempted first where possible. Occasionally, however, surgical endodontic re-treatment may be indicated as the first line of therapy if a periapical biopsy is required, or in cases where retrieval of extruded endodontic material is necessary.
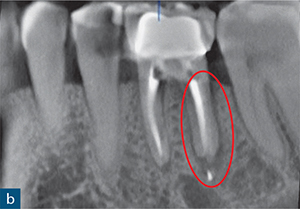

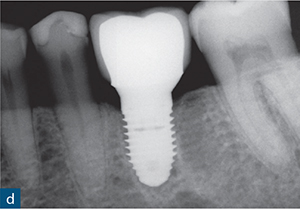
Fig 8-2 (a) A periapical radiograph of a root-treated symptomatic mandibular left first molar showing no sign of periapical or periradicular radiolucency. (b) The sagittal CBCT slice reveals subtle bone loss along the distal aspect of the distal root extending towards the root apex (red outline), indicating a vertical root fracture. (c) The extracted mandibular left first molar confirming the vertical fracture line (yellow arrow). (d) The extracted tooth was replaced with a dental implant (implant placement by Dr Andrew Dawood).
Non-surgical endodontic re-treatment
CBCT has been shown to be useful in the management of failed root canal treatments (Davies et al, 2015b) and may provide information regarding the presence, exact location (root) and nature of periapical lesions that may not be readily detected on conventional radiographs (Simon et al, 2006; Patel et al, 2012; Cheung et al, 2013).
Furthermore, additional root canals (Blattner et al, 2010; Neelakantan et al, 2010) and complications, such as vertical root fractures (Fig 8-2), perforations (Figs 8-3 and 8-4), and the nature and position of resorption defects (Figs 8-5 and 8-6) may be readily identified with CBCT (D’Addazio et al, 2011; Shemesh et al, 2011).
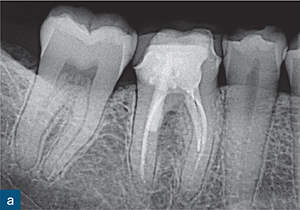
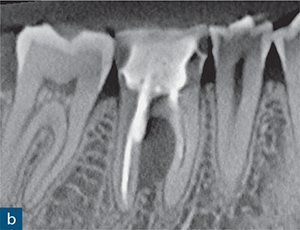
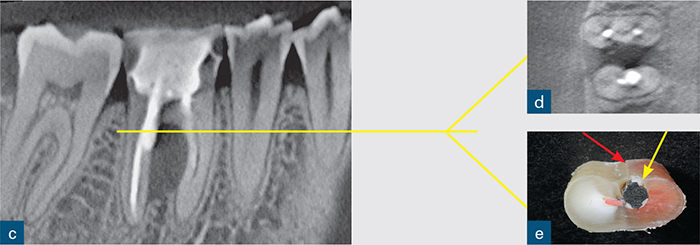
Fig 8-3 (a) A periapical radiograph of a symptomatic root-treated mandibular first molar with slight tenderness to percussion but no other obvious signs of endodontic or periodontal disease and no sign of periapical or periradicular radiolucency. The treatment plan included non-surgical endodontic re-treatment. The post space may have perforatedthe mesial aspect of the distal root. However, this radiographic appearance could also be due to the relationship of the X-ray beam to the digital sensor. (b and c) The CBCT scan changed the treatment plan; the sagittal CBCT slice revealed a large inter-radicular radiolucency, suggesting a perforation. (d) Axial CBCT slice revealing the extent of the perforation and inter-radicular bone loss. (e) The unsalvageable tooth was extracted, confirming the presence not only of the perforation (yellow arrow) but also of a vertical root fracture (red arrow).
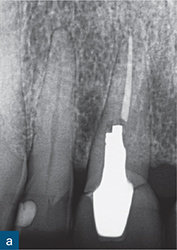
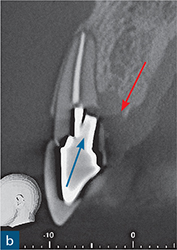
Fig 8-4 (a) A periapical radiograph of a root-treated maxillary right central incisor restored with a post-retained crown. Clinical examination revealed a 4 mm periodontal probing depth palatally, but the examination was otherwise unremarkable. On the periapical radiograph, the post appears to have deviated distally but the lamina dura is intact and there is no sign of widening of the periodontal ligament space or of an obvious periapical or periradicular radiolucency. In addition, the root filling looks acceptable in terms of length and density. (b) Sagittal CBCT slice revealed the palatal angulation of the post preparation (blue arrow) and a coronal third root perforation. The associated palatal bone loss is clearly evident (red arrow).
Presence of a periapical lesion
It is well established that conventional radiographs may not detect periapical lesions, especially on molar teeth (Cheung et al, 2013; Liang et al, 2014; Venskutonis et al, 2014a). The presence of a periapical radiolucency, not detected on a conventional radiograph, may have an effect on whether an existing root canal treatment should be left alone or re-treated prior to providing a new coronal restoration (Figs 8-2 and 8-3). Davies et al (2015b) assessed the outcome of non-surgical root canal re-treatment radiographically and found a lower number of favourable outcomes with CBCT compared to periapical radiographs. The assessment with CBCT affected the management of the reviewed cases. The ability of CBCT to diagnose periapical disease is further discussed in Chapter 7.

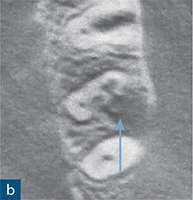
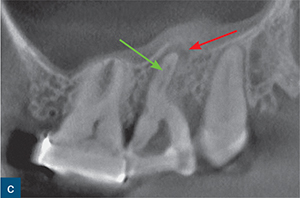
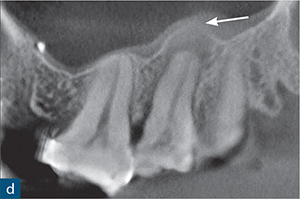
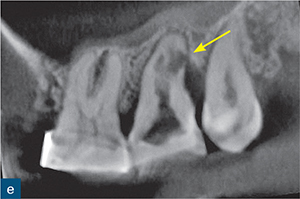
Fig 8-5 (a) A periapical radiograph of a maxillary left second molar, in which endodontic treatment was aborted due to failed anaesthesia. The patient was referred to a specialist endodontist. (b) The axial CBCT slice revealed the presence of internal root resorption, which had perforated the distobuccal, mesiobuccal and palatal root canal walls (blue arrow). (c to e) Sagittal CBCT reconstructed images: (c) the mesiobuccal root; (d) the palatal root; and (e) the distobuccal root. The CBCT images reveal the true size and nature of the resorptive lesion in the mesiobuccal and palatal roots (c and d), which are associated with periapical radiolucencies (red and white arrows); there are also signs of internal resorption associated with the mesiobuccal canal (green arrow) and the distobuccal root (e), which is associated with a very large perforating internal root resorption lesion (yellow arrow). Note the amount of root surface loss due to resorption in (e) and the associated distal bone loss. Without prior knowledge about the presence and nature of the resorptive lesion, there would be a very high risk of causing a hypochlorite accident during chemomechanical root canal treatment. This unsalvageable tooth was extracted.

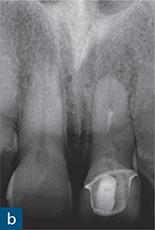
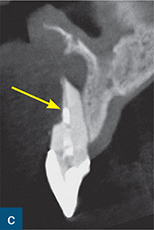
Fig 8-6 (a) A photograph and (b) periapical radiograph of the maxillary left central incisor tooth. The symptomatic tooth has been root-treated and there is an associated persistent round and well-circumscribed periapical radiolucency. The root filling lacks adequate length and density. During non-surgical endodontic re-treatment, the apex locator reading was erratic and the zero reading and working length could not be reliably established. (c) Sagittal CBCT reconstructed image through the same tooth revealed significant loss of labial root structure from the coronal third to the apex (yellow arrow) and associated periapical bone loss. Root canal re-treatment was not possible and the tooth was extracted.
The differential diagnosis of a cyst from a periapical granuloma using CBCT has also been investigated (Simon et al, 2006; Rosenberg et al, 2010; Guo et al, 2013). In a clinical study, Bornstein et al (2015) concluded that CBCT could not reliably differentiate between a granuloma and a cyst. At present, the only reliable diagnosis can be made by in-toto excision and subsequent serial sectioning of the lesion (Nair et al, 1996).
CBCT has been shown to be beneficial in the diagnosis of vertical root fractures (VRFs). Subtle periradicular signs of bone loss indicating a VRF associated with a root-treated tooth (Fig 8-2), which may be challenging to diagnose by other means, may be evident on CBCT examination (Bernades et al, 2009; Wang et al, 2011; Kajan and Taromsari, 2012). The presence or absence of a VRF will have an impact on treatment planning and is described in more detail in Chapter 11.
Quality of existing root canal treatment
Clinical and population studies have shown a strong correlation between the quality of root canal fillings and the outcome of treatment (Liang et al, 2012a; Kirkevang et al, 2014). The quality of the root canal filling is usually assessed by periapical radiographs and is focused on the length and density of the filling (Fig 8-7). A root canal filling that terminates 0 to 2 mm from the radiographic apex has been shown to be more likely to result in a favourable outcome, compared to long or short fillings (European Society of Endodontology, quality guidelines, 2006; Liang et al, 2012a). A void-free root canal filling also results in a higher success rate (Sjögren et al, 1990; Song et al, 2011; Ng et al, 2011).
Liang et al (2012a) demonstrated an overestimation of root canal filling quality by radiographs compared to CBCT. On conventional radiographs when the root filling was flush at the radiographic apex, it was actually long on CBCT. Furthermore, CBCT was also found to be superior to conventional radiography in detecting root filling voids, especially in the buccolingual plane of the root filling (Liang et al, 2012a).
The additional information from a CBCT scan may influence whether the clinician decides to carry outnon-surgical or surgical endodontic re-treatment in refractory cases. In some instances, extraction may be the only viable treatment option (D’Addazio et al, 2011; Shemesh et al, 2011; Eskandarloo et al, 2012).
Missed root canals and anatomical features
Inadequate disinfection of the root canal system may lead to failure of root canal treatment. (Ng et al, 2008). One of the reasons for persistent intra-radicular infection is failure to identify and treat all canals during treatment. The ability of CBCT to detect supplemental canals (Figs 8-8 and 8-9) and anatomic aberrations is well established (Tu et al, 2007, 2009; Abella et al, 2012; Davies et al, 2015a). Nevertheless, incorrect interpretations of images resulting in false positive diagnoses of supplemental canals may occur from scatter caused by filling materials in an adjacent root filled canal (Krithikadatta et al, 2010).
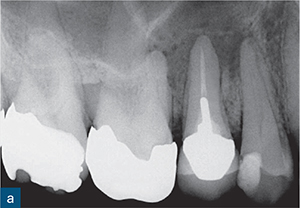

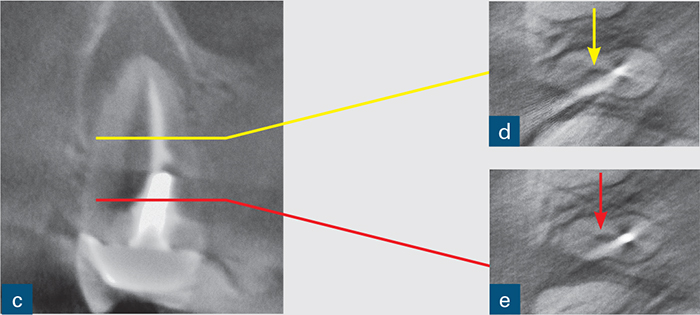
Fig 8-7 (a) A periapical radiograph of a root-treated maxillary right second premolar revealing a large, well-circumscribed periapical radiolucency associated with this tooth. The density and length of the root filling appear to be satisfactory. (b) Sagittal CBCT slice confirms the findings on the periapical radiograph. However, (c) a coronal CBCT slice through the same tooth shows that the palatal canal has not been identified, and around 75% of the canal system has not been obturated. Axial CBCT slices through the middle (d) and coronal (e) thirds of the same tooth also reveal the untreated palatal canal (arrows). The diagnosis of apical periodontitis was confirmed with the aid of a periapical radiograph. However, the presence of the palatal canal could not be confirmed from the periapical radiograph. This knowledge is essential to allow for thorough and predictable instrumentation.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



