Classification
Mechanism of injury
Clinical manifestation
Prognosis
Neurapraxia (Transient block)
Mild injury to the nerve; no loss of continuity of the nerve
Paresthesiaa
Good prognosis; recovery usually within days or up to 1–2 months
Axonotmesis (Lesion in continuity)
Moderate injury to the nerve; nerve is damaged but not completely severed
Initial anesthesiab followed by paresthesiaa as recovery begins
Moderate prognosis; recovery may occur in 2–4 months, but improvement leading to recovery may last up as 12 months
Neurotmesis (Nerve cut)
Severe injury to the nerve; severed nerve
Initial anesthesiab, which may be followed by paresthesiaa, or other neurosensory responses such as allodyniac, hyperalgesiad, or chronic pain
Poor prognosis; sensory recovery is never complete
Etiology
The most routine surgical endodontic procedures, such as anesthetic procedures [8], flap procedures, osteotomy, and apicectomy, may lead to nerve injury during surgical endodontic treatments [14, 15].
The possible causes of nerve injury include both preoperative factors, such as poor flap design, and intraoperative factors, such as traumatic flap reflection, accidental intraneural injection, traction of the mental nerve during flap elevation, penetration of the osteotomy preparation into the nerve canal, and more [19]. In addition, nerve injuries may be caused indirectly by postsurgical complications such as the development of intra-alveolar hematoma or edema inside the mandibular canal applying temporary pressure increase on the nerve bundle or neuritis with prolonged pressure increase that may lead to permanent degeneration of the affected nerve [20].
Prevention
Prevention is the most efficient clinical approach to minimize the risk of nerve injuries during endodontic surgical procedures and ensuing medical and medicolegal consequences. For medicolegal reasons, it is important to include nerve injury as an item in the informed consent document [5, 22–25]. The medicolegal aspects of altered sensation following endodontic surgical procedures are presented in a separate chapter of this book.
Nerve injury preventive measures should be implemented preoperatively, intraoperatively, and postoperatively, as described below.
Preoperative Preventive Measures
“Primum non nocere” (a Latin phrase that means “first, do no harm”) is a fundamental principle that should be implemented in the planning of any treatment procedure. Thus, the practitioner should take into account all possible complications and preventive measures prior to treatment, i.e., during the evaluation and treatment planning phase. In order to apply this principle in endodontic surgery, the practitioner is obligated to perform a thorough clinical and radiographic evaluation, to be aware of possible risk factors, to recognize all necessary anatomical considerations in advance, to plan the treatment adequately, and to verify that the procedure is within his/her skills [5–7, 9, 11, 12, 14, 15].
Table 13.2 presents preventive measures for altered sensation in endodontic surgery.
Table 13.2
Preventive measures for altered sensation during and following endodontic surgery
|
Preoperative measures
|
Thorough clinical and radiographic evaluation (computed tomography when indicated)
|
|
Risk factors evaluation
|
|
|
Anatomical considerations
|
|
|
Adequate treatment planning
|
|
|
The procedure is within the practitioners skills
|
|
|
Medicolegal precautions (informed consent)
|
|
|
Intraoperative measures
|
Anatomical considerations
|
|
Magnification and conservative microsurgical techniques
|
|
|
Adequate surgical procedures (injection, flap design and management, osteotomy, suturing)
|
|
|
Case-specific surgical adjustments
|
|
|
Consideration of early intervention in case a possible nerve injury is suspected
|
|
|
Postoperative measures
|
Postoperative anti-inflammatory adjuncts consideration
|
|
Follow-up
|
|
|
Timely mannered and adequate clinical and medicolegal response in case a nerve injury is suspected
|
Thorough medical history and clinical examination and good-quality radiographs are essential for preoperative diagnosis of teeth scheduled to undergo apical surgery [9, 11, 12, 14, 15]. Periapical (PA) radiography is the principal radiographic modality used for diagnosis and treatment planning prior to endodontic surgery. However, in certain cases, PA radiography alone may be clinically limited by the fact that the information is rendered in only two dimensions [9, 11, 12, 14, 15]. The use of computed tomography (CT) scans and more recently cone-beam CT (CBCT) enables the visualization of the dentition, the maxillofacial skeleton, and the surrounding anatomical structures in three dimensions [26]. In endodontic surgery, CBCT facilitates the evaluation of the true extent of PA lesions and of the relationships between the PA lesions/root apices and anatomical landmarks such as neurosensory structures. Thus, the CBCT enables the planning of a more predictable surgical approach [9, 10, 13, 26–29]. However, the decision whether to use CBCT scan or not must be based on the patient’s history, clinical examination, and an initial PA radiographic evaluation and should be justified on an individual basis [9, 27]. Figure 13.1 presents a case selection algorithm for performing a CBCT scan, aimed at either prevention or management of nerve injuries related to endodontic surgical treatments [27].
Fig. 13.1
Case selection algorithm for CBCT scan aimed for the prevention or management of nerve injuries related to endodontic surgical treatments. (1) Unless, CBCT evaluation may be indicated for clinical demands other than the prevention or management of nerve injuries. (2) Specific indications for CBCT evaluation in order to prevent or manage nerve injuries related to endodontic surgery: determine the exact location of root apex/apices and/or periapical lesion and their anatomical relation to adjacent neurosensory structures; suspected complex tooth morphology or surrounding anatomical structures or anatomical superimposition of roots or areas of the maxillofacial skeleton that might contribute to an increased risk of nerve injury during surgery; patients with nonspecific clinical signs and symptoms that may be related to a nerve injury; and assessment of endodontic treatment complications related to potential nerve injury [27]
Several possible risk factors for nerve injury related to endodontic treatments have been reported, including the patient’s gender [22, 24, 25] and the tooth location [7]; some may be relevant specifically to endodontic surgical procedures. Knowing the possible risk factors for nerve injury may be useful for prevention, screening, and diagnosis of such injuries.
A female predominance was described in several nerve injury studies, such as nerve injury related to local anesthesia injection, third molar surgery, lingual nerve repair, and nerve injury caused by dental treatment and traumatic injuries [18, 22, 24, 25]. The reason for this gender discrepancy may be explained by the fact that relatively more female patients are seeking dental treatment [24, 30]. Gender anatomical variation may be another possible explanation – females have significantly shorter vertical distances from the IAN to the root apices of mandibular molar teeth, which may potentially pose an increased risk of nerve injury during mandibular molar endodontic surgery in female patients compared to male patients [13].
A relative predominance of nerve injuries related to endodontic treatments of the second mandibular molars has been reported (example in Fig. 13.2) [5]. The anatomical structure of the IAN and its relations to the surrounding anatomical structures may have a significant role in this finding: The trabecular pattern of the cancellous bone in the mandibular molar region is characterized by a consistently loose appearance, numerous vacuoles and often without any cortical bone protecting the pedicle [5–7]. In the second mandibular molar, the distance between the apices and the pedicle of the IAN is often less than 1 mm, compared to a more variable distance observed in the first molar teeth (1–4 mm) [7]. The artery usually follows the IAN, running along the superomedial side from the mandibular foramen to the 1st molar and then becoming lateral, up to the mental foramen (Fig. 13.3) [7].
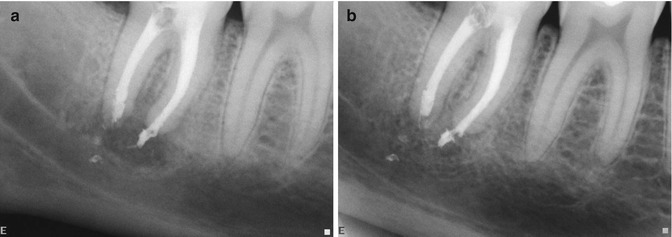
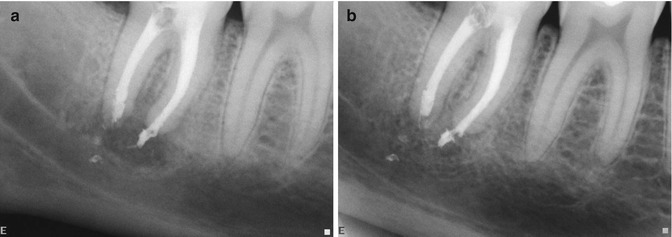
Fig. 13.2
Nerve injury following an endodontic treatment of mandibular second molar. (a) Nonsurgical endodontic treatment in the mandibular second molar. Radiographic evidence of overfilling of the endodontic filling material in the vicinity of the IAN. The patient presented with IAN paresthesia following the treatment, and was treated by corticosteroids for 1 week and then was followed up for several months. (b) At 6 months follow-up, healing process of the periapical lesion was demonstrated. A gradual resolution of the paresthesia symptoms was demonstrated in the months following the endodontic treatment, with return to normal neural function 3 months following the treatment
Fig. 13.3
The inferior alveolar nerve (IAN) anatomy. The artery (in red) usually follows the IAN (in yellow)
The nerve supply of the maxillary sinus membrane is provided by the three superior alveolar nerves, the anterior palatine nerve, and the infraorbital nerve [31]. These nerves pass enclosed within the wall of the sinus and innervate also the related maxillary teeth. Thus, endodontic surgery of maxillary teeth may involve these nerves and induce nerve injuries [31].
Damage to the mental nerve is also a major concern during endodontic surgical procedures of mandibular posterior teeth [5, 7, 14, 15, 32, 33]. The mental nerve exits the body of the mandible through the mental foramen (MF, Fig. 13.3) and innervates the skin of the chin and the skin and mucous membrane of the lower lip [32, 33]. The common location of the MF is inferior to the second premolar, but the MF location may be variable [32, 33]. In addition, small accessory foramina (accessory mental foramina (AMF)) may also exist in the surrounding area of the MF, usually located in the apical area of the first molar and in the posterior or inferior areas of the mental foramen [32, 33]. It is important to know in advance the location of the MF and the innervation map of the mental nerve, in order to avoid damage to the neurovascular bundle during endodontic surgical procedures in this region [14, 15] as well as for an accurate and specific diagnosis of such damage in case it occurs following the procedure.
The clinical and surgical competence of the practitioner to perform the surgical procedure is an important prerequisite to performing surgical procedures. This competence exists when the practitioner has sufficient knowledge and skills such that the procedure can be performed to obtain the intended outcomes with minimal risks of harm to the patient [34, 35]. A practitioner’s clinical competence is a combination of several components, including the following: knowledge, clinical decision-making capability, good judgment, technical skills, clinical attitudes, professional habits, and interpersonal skills. Each of these must be mastered by the practitioner, using a variety of sources of information and skill acquisition prior to performing any surgical procedure, in order to achieve predictable clinical results while minimizing the risk for potential complications, including nerve injuries [5, 24, 34, 35]. Therefore, practitioners should consider whether the procedure is relevant to their practice, recognize the expected outcomes, be familiar with potential risks and complications, and practice self-evaluation [34, 35]. It is prudent to verify that the procedure is within the practitioner’s clinical skills and also that the practitioner is capable to prevent, diagnose, and manage possible complications such as nerve injuries.
Intraoperative Preventive Measures
All surgical procedures should be performed while balancing between two parallel aims: to provide the most favorable conditions for success and to take all measures to prevent potential complications. The preventive measures include the following: implementation of relevant anatomical considerations, the use of magnification and conservative microsurgical techniques, practicing adequate surgical procedures (such as proper and careful injection techniques, adequate flap design and management, cautious osteotomy, and careful suturing), implementation of case-specific surgical adjustments, and considering early intervention in case a possible nerve injury is suspected (Table 13.2) [5–7, 9, 11, 12, 14, 15].
It is prudent to balance between the two aforementioned aims of providing the most favorable conditions for success while preventing possible nerve injury, and it requires knowledge, experience, and awareness from the practitioner. For example, the osteotomy is aimed to provide an adequate surgical approach for proper management of the apical part of the root, thus providing the optimal conditions for success [14], but on the other hand, an excessive osteotomy may cause damage to adjacent anatomical structures such as nerve bundles [7, 14–16, 36]. Thus, the practitioner is required to achieve a complex equilibrium between the clinical demands required for a successful procedure and measures required for preventing damage.
During surgery of mandibular posterior teeth, damage to the mental nerve may occur by direct cutting of the nerve bundle or by stretching or crushing the neurovascular bundle with the retractor [14, 15]. Cutting and stretching may be avoided by an adequate flap design; crush injuries are often caused by impinging the retractor against the base of the flap in which the mental nerve is contained [14, 15]. Kim and Kratchman [14] suggested to first identify the mental foramen, then to carefully cover it with the retractor, and then to make a 15-mm long horizontal groove in the bone just above it and beyond the apex, to allow space for the osteotomy and subsequent apicoectomy. Once the retractor is in position within the groove, there should be no movement or slippage [14]. While it sometimes may be necessary to make such a groove, generally it is desirable to avoid unnecessary manipulations in the vicinity of nerve bundles. It is also advised to be aware of the risk of injury to the nerve when performing surgery of mandibular posterior teeth.
Endodontic surgery of mandibular molars poses even greater technical challenges, attributed to factors as the close proximity of the apices to the mandibular canal [12], the difficult access to the roots as a result of the posterior location [11, 14], and the thickness of the buccal cortical bone plate [9, 14]. This challenging anatomical situation may increase the risk of nerve injury during the endodontic surgical procedure [9, 36].
Therefore, case-specific anatomical challenges may require specific treatment planning and specific surgical adjustments, in order to achieve predictable clinical results safely.
In modern endodontics, the use of magnification and illumination devices has been implemented, enabling the practitioners to magnify the treatment field [37], with the aim of improving the accuracy and quality of treatment [38, 39]. The basic principle of microsurgery is that the surgeon’s hands can execute remarkable micromanipulations as long as the surgeon’s eyes can see a magnified operation field [37, 40]. Therefore, the application of magnification and illumination in surgical endodontic treatments, which allows easier and more precise identification of anatomical and pathological structures [41–45], may facilitate all phases of the surgical treatment to be done with greater accuracy and safety [38]. In this sense, it may allow a more conservative surgical treatment, especially when it is performed in the vicinity of neurovascular bundles, and therefore may reduce nerve injury risks.
Additional intraoperative surgical procedures that may be related to potential nerve injury, such as anesthetic injections, are discussed in other chapters of this book.
Postoperative Preventive Measures
Endodontic surgical procedures are usually performed under local anesthesia. Thus, the clinical symptoms of surgery-related nerve injuries will usually be evident only after the surgical procedure, when the local anesthesia wears out. On the other hand, in many cases, when a nerve injury did occur during the procedure, early intervention is of utmost importance. Thus, following the surgical procedure the practitioner, with the cooperation of the patient, needs to be alert to detect any possible sign of altered sensation [5, 6, 16, 24].
Early symptoms that may suggest a possible nerve injury include acute pain during or after the surgical procedure or neurosensory alterations, such as paresthesia, anesthesia, or hyperesthesia [46].
If a nerve injury is suspected, the clinician should perform a basic neurosensory evaluation, to ascertain whether the patient indeed experiences altered sensation signs, and document the findings [5, 6, 16, 24]. Then, a rigorous follow-up protocol should be followed.
In the absence of a definitive nerve injury diagnosis, a preventive approach of early intervention may be considered [5, 6, 16, 24], consisting the use of corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs). The use of corticosteroids, if administered within a few days of the nerve injury, may minimize neuropathy, inhibit axon sprouting, and prevent neuroma formation [5, 6, 16, 24, 47, 48].
Diagnosis
Prevention is the most efficient way to address a nerve injury. However, when this serious complication occurs, a correct and timely mannered diagnosis is of outmost importance for preventing further damage, enabling appropriate management, and improving the healing prospect [2–4, 6, 8, 23–25, 49, 50].
Neurosensory impairment represents a complex clinical scenario with various clinical and psychological manifestations. Thus, sometimes the clinical manifestation of the nerve injury, such as persistent pain, may be confused with other postoperative symptoms [4, 16, 51–56]. Polycarpou et al. [55] evaluated cases of persistent pain after apparently successful nonsurgical and surgical endodontic treatments and reported the following risk factors: presence of preoperative pain from the tooth site lasting at least 3 months, history of previous chronic pain experience or painful treatment in the orofacial region, and female gender [55
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


