Armamentarium
|
History of the Procedure
Craniofacial surgeons use a variety of reconstructive approaches to correct the upper midface deformities observed in craniosynostosis syndromes, frontonasal dysplasias, midline cranio-orbital clefting, and isolated orbital hypertelorism. In 1971 Tessier described a single-stage frontofacial advancement in which the fronto-orbital band was advanced as a separate element in conjunction with the Le Fort III complex below and the frontal bones above. Seven years later, Ortiz-Monasterio et al. developed the monobloc osteotomy to advance the orbits and midface as one unit, combined with forehead repositioning to correct the deformity of Crouzon syndrome. In 1979 van der Meulen described the “median fasciotomy” for the correction of midline facial clefting. Van der Meulen split the monobloc osteotomy vertically in the midline, removed central nasal and ethmoid bone, and then moved the two halves of the face together for correction of orbital hypertelorism. To correct the midface dysplasia and associated orbital hypertelorism in patients with Apert syndrome, Tessier refined the vertical splitting and reshaping of the monobloc segment, thus correcting the midline deformity in three dimensions, in a procedure now known as facial bipartition.
History of the Procedure
Craniofacial surgeons use a variety of reconstructive approaches to correct the upper midface deformities observed in craniosynostosis syndromes, frontonasal dysplasias, midline cranio-orbital clefting, and isolated orbital hypertelorism. In 1971 Tessier described a single-stage frontofacial advancement in which the fronto-orbital band was advanced as a separate element in conjunction with the Le Fort III complex below and the frontal bones above. Seven years later, Ortiz-Monasterio et al. developed the monobloc osteotomy to advance the orbits and midface as one unit, combined with forehead repositioning to correct the deformity of Crouzon syndrome. In 1979 van der Meulen described the “median fasciotomy” for the correction of midline facial clefting. Van der Meulen split the monobloc osteotomy vertically in the midline, removed central nasal and ethmoid bone, and then moved the two halves of the face together for correction of orbital hypertelorism. To correct the midface dysplasia and associated orbital hypertelorism in patients with Apert syndrome, Tessier refined the vertical splitting and reshaping of the monobloc segment, thus correcting the midline deformity in three dimensions, in a procedure now known as facial bipartition.
Indications for the Use of the Procedure
Craniosynostosis, or premature fusion of cranial sutures, affects approximately 1 in 2500 children. Patients may present with a wide range of phenotypic and functional deformities that are etiologically heterogeneous and pathogenetically variable. Complex craniosynostosis, defined as the fusion of multiple cranial sutures, occurs in about 5% of nonsyndromic cases. Cloverleaf skulls, representing the extremes of phenotypic severity, are pathogenetically variable. Synostosis may involve the coronal, lambdoid, and metopic sutures, marked by bulging of the cerebrum through an open sagittal suture or, in some cases, through patent squamosal sutures. Isolated cloverleaf skull occurs in about 20% of cases. Apert syndrome is characterized by craniosynostosis, midface deficiency, symmetric syndactyly of the hands and feet, and other abnormalities. Crouzon syndrome is characterized by craniosynostosis, maxillary hypoplasia, shallow orbits, and ocular proptosis. Pfeiffer syndrome is characterized by craniosynostosis, midface deficiency, broad thumbs and/or great toes, brachydactyly, variable soft tissue syndactyly, and other anomalies. Saethre-Chotzen syndrome is characterized by a heterogeneous phenotypic presentation involving craniosynostosis, a low-set frontal hairline, facial asymmetry, ptosis of the eyelids, deviated nasal septum, brachydactyly, partial soft tissue syndactyly of the second and third fingers, and various skeletal anomalies.
Morphologic Considerations
Examination of the patient’s entire craniofacial region should be meticulous and systematic. The skeleton and soft tissues are assessed in a standard way to identify all normal and abnormal anatomy. Specific findings tend to occur in particular malformations, but each patient is unique. The achievement of symmetry and normal proportions and the reconstruction of specific esthetic units are essential to forming an unobtrusive face in a child born with one of the craniosynostosis syndromes.
Frontoforehead Esthetic Unit
The frontoforehead region is dysmorphic in an infant with a craniosynostosis syndrome. Establishing a normal position of the forehead is critical for overall facial symmetry and balance. The forehead may be considered as two separate esthetic components: the supraorbital ridge–lateral orbital rim region and the superior forehead. The supraorbital ridge–lateral orbital rim unit includes the nasofrontal process and supraorbital rims extending inferiorly down each frontozygomatic suture toward the infraorbital rim and posteriorly along each temporoparietal region. The shape and position of the supraorbital ridge–lateral orbital rim region are key elements of upper facial esthetics. In a normal forehead, at the level of the nasofrontal suture, an angle ranging from 90 to 110 degrees is formed by the supraorbital ridge and the nasal bones when viewed in profile. Additionally, the eyebrows, overlying the supraorbital ridge, should be anterior to the cornea. When the supraorbital ridge is viewed from above, the rim should arc posteriorly to achieve a gentle 90-degree angle at the temporal fossa with a center point of the arc at the level of each frontozygomatic suture. The superior forehead component, about 1 to 1.5 cm up the supraorbital rim, should have a gentle posterior curve of about 60 degrees, leveling out at the coronal suture region when seen in profile.
Orbito-Naso-Zygomatic Esthetic Unit
In the craniosynostosis syndromes, the orbito-naso-zygomatic regional dysmorphology is a reflection of the cranial base malformation. In Crouzon syndrome, in which bilateral coronal suture synostosis is combined with skull base and midface deficiency, the orbito-naso-zygomatic region is dysmorphic and consistent with a short (anterior-posterior) and wide (transverse) anterior cranial base. In Apert syndrome, the nasal bones, orbits, and zygomas, like the anterior cranial base, are transversely wide from anterolateral bulging of the temporal lobes of the brain and horizontally short (retruded), resulting in a shallow, hyperteloric, “reverse curved” upper midface. Surgically advancing the midface without simultaneously addressing the increased transverse width and reverse curve will not adequately correct the dysmorphology.
Maxillary–Nasal Base Esthetic Unit
In the patient with a craniosynostosis syndrome and midface deficiency, the upper anterior face is vertically short (nasion to maxillary incisor), and there is a lack of horizontal (A-P) projection. These findings may be confirmed through cephalometric analysis, which indicates a deficient SNA angle and a short upper anterior facial height (nasion to anterior nasal spine). The width of the maxilla in the dentoalveolar region is generally constricted, with a highly arched palate. To normalize the maxillary–nasal base region, multidirectional surgical expansion and reshaping are generally required. The abnormal maxillary lip-to-tooth relationship and Class III occlusion are improved through Le Fort I segmental osteotomies and orthodontic treatment as part of the staged reconstruction. The mandible and chin are frequently secondarily involved and benefit from surgical repositioning as part of the orthognathic correction.
Considerations in the Timing of Reconstruction
In considering both the timing and type of intervention, the experienced surgeon takes several biologic realities into account, including the natural course of the malformation (i.e., progressively worsening dysmorphology or a nonprogressive craniofacial abnormality); the tendency for growth restriction in operated skeletally immature bones (i.e., akin to the maxillary hypoplasia that occurs after cleft palate repair); the relationship between the underlying developing viscera (i.e., the brain) and the congenitally affected and/or surgically altered skeleton (i.e., brain compression if the cranial vault is not expanded); and the child’s airway needs (i.e., midface deficiency resulting in obstructive sleep apnea [OSA]).
To limit impairment while simultaneously achieving long-term preferred facial esthetics and head and neck function, the surgeon must ask an essential question: During the course of craniofacial development, does the operated-on facial skeleton of a child with a craniosynostosis syndrome tend to grow abnormally, resulting in further distortions and dysmorphology, or are the initial positive skeletal changes achieved (at surgery) maintained during ongoing growth? Unfortunately, the proposed theory that craniofacial procedures carried out in early infancy “unlock growth” has not been documented through the scientific method.
Limitations, Contraindications, and Alternatives
Management of the Upper Midface Deformity
Upper Midface Reconstruction Options
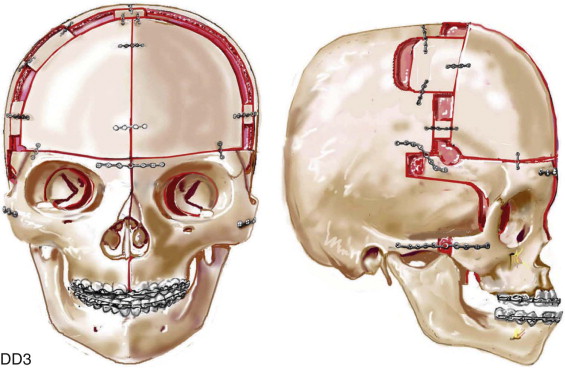
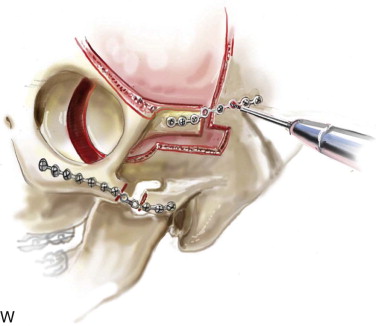
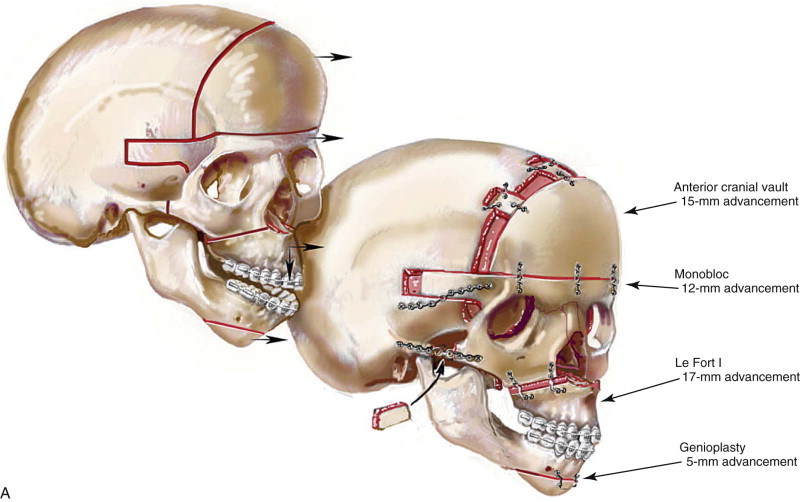
The approach selected to manage the “upper midface” deficiency/anomalies and residual cranial vault dysplasia in the child with a craniosynostosis syndrome should offer definitive corrections. A main objective of this phase of reconstruction is to “normalize” the orbits, zygomas, and cranial vault. Correction of the maxillomandibular deformity requires orthognathic surgery, including a separate Le Fort I osteotomy. The selection of a monobloc (with or without additional orbital segmentation), a facial bipartition (with or without additional orbital segmentation), or an extracranial Le Fort III osteotomy to manage the basic horizontal, transverse, and vertical upper and midface deficiencies/anomalies should depend on the patient’s specific morphology. The presenting dysmorphology is determined by the original malformation, the previous procedures carried out, and the effects of those procedures on growth ( Figures 48-1 to 48-3 ).




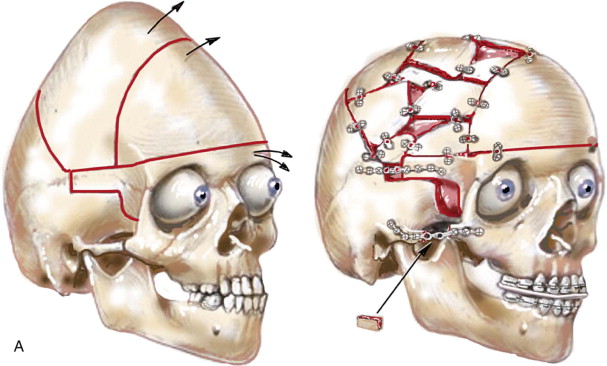


When evaluating the upper and midface morphology in the mixed dentition child or young adult born with Crouzon syndrome, the surgeon should note (1) whether the supraorbital ridge is in good position when viewed from the sagittal plane (is the depth of the upper orbits adequate?); (2) whether the midface and forehead have an acceptable arc of rotation in the transverse plane (is the midface arc concave?); and (3) whether the root of the nose and orbits are of normal width (is there orbital hypertelorism?). If these structures are confirmed to have acceptable morphology, there is no need to further reconstruct the forehead and upper orbits. In those few patients with a craniosynostosis syndrome in whom the residual deformity is only in the lower half of the orbits, the zygomatic buttress, and the maxilla, an extracranial Le Fort III is likely to be effective treatment.
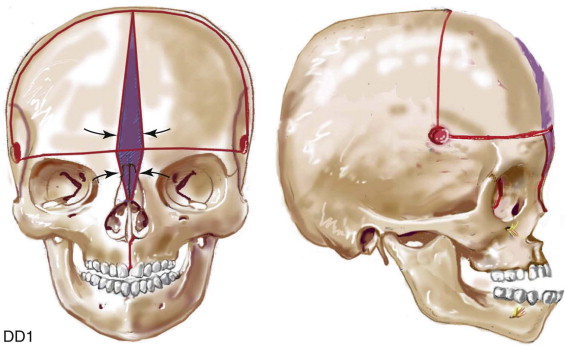
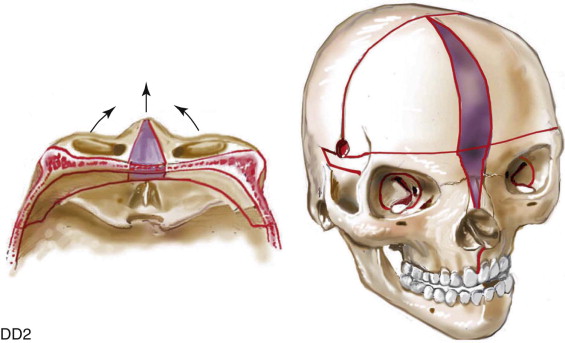
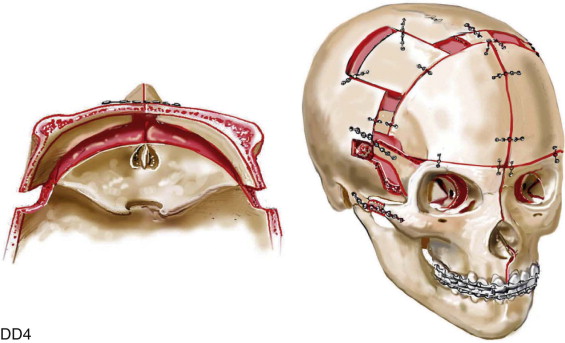
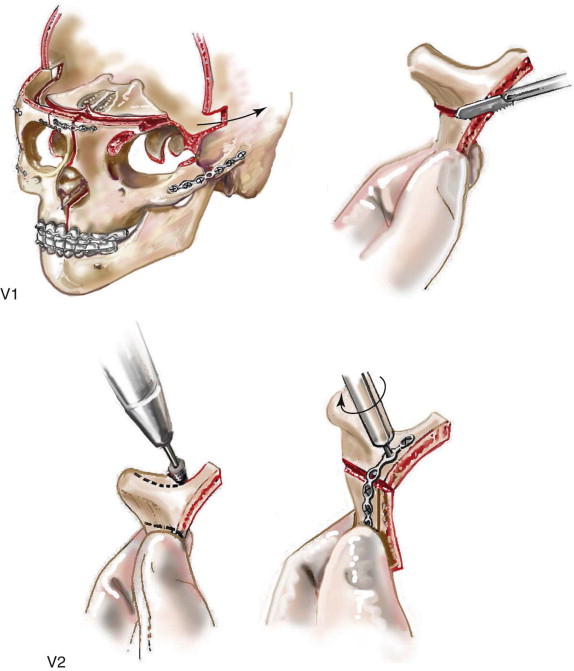
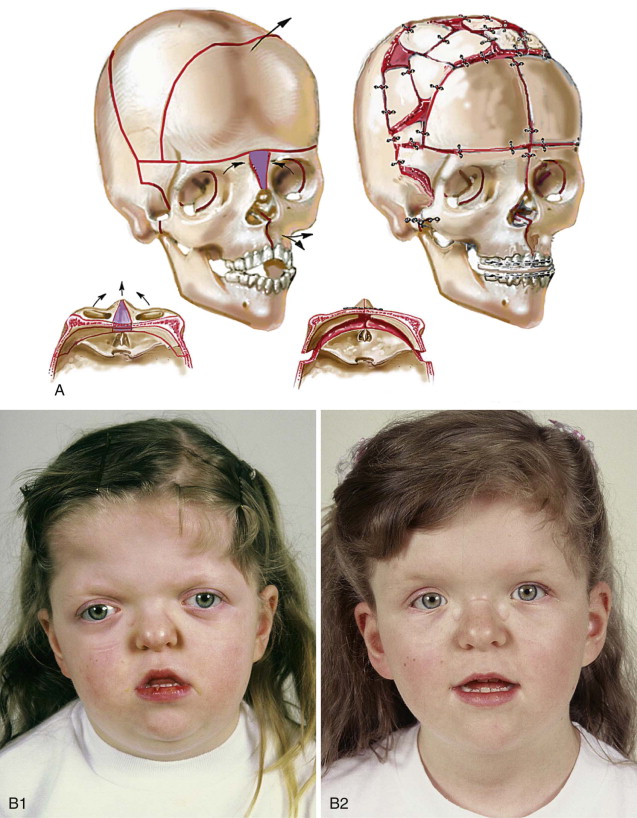
If the supraorbital region, anterior cranial base, zygomas, and root of the nose, in addition to the lower orbits, and the maxilla all remain deficient in the sagittal plane (horizontal retrusion), a monobloc is indicated. In these patients, the forehead is also generally flat and retruded and requires reshaping and advancement. If upper midface hypertelorism (increased transverse width) with midface flattening (horizontal retrusion) and a concave facial curvature (reverse facial arc) also is present, the monobloc unit is split vertically in the midline (facial bipartition). A wedge of interorbital (nasal and ethmoidal) bone is removed, and the orbits and zygomas are repositioned medially while the maxillary arch is widened. A facial bipartition (FB) is rarely required in Crouzon syndrome, but the monobloc (MB) is. When an MB or FB osteotomy is carried out as the upper midface procedure, additional segmentation of the upper and lateral orbits may also be required to normalize the morphology of the orbital esthetic units.
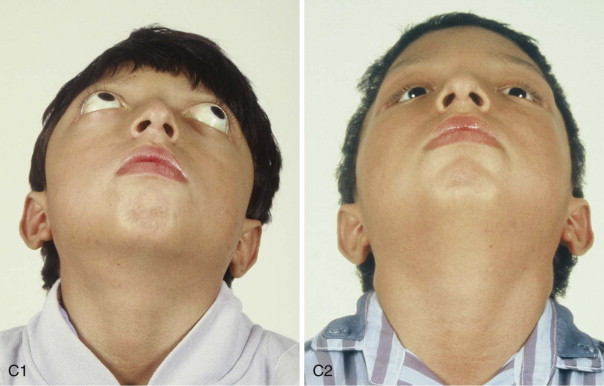
For almost all patients with Apert syndrome, facial bipartition osteotomies combined with further cranial vault reshaping permit a better correction of the dysmorphology than can be achieved through any other upper midface procedure (i.e., monobloc or Le Fort III). When FB osteotomies are used, correction of the concave midface arc of rotation is also possible. This further reduces the stigma of the Apert flat, wide, and retrusive facial appearance. The FB procedure allows the orbits and zygomas to shift to the midline (correction of hypertelorism) as units while the maxilla is simultaneously widened (i.e., relief of the V -shaped face). Horizontal advancement of the reassembled upper midface complex is then possible to improve orbital depth and zygomatic length. The forehead is generally flat, tall, and retruded, with a constricting band just above the supraorbital ridge. Reshaping of the anterior cranial vault is also simultaneously carried out. A Le Fort III osteotomy is virtually never adequate for an ideal correction of the residual upper midface anomalies documented in Apert syndrome.
A study by McCarthy confirms that the Le Fort III osteotomy is not effective as an esthetic option to manage the upper midface deformity in the majority of patients with craniosynostosis syndrome. By anatomic design, the Le Fort III procedure prevents management of the whole orbital esthetic unit during one operative setting. Therefore, a major esthetic shortcoming of the Le Fort III osteotomy, when its indications do not fit the presenting dysmorphology, is the creation of irregular stepoffs in the lateral orbital rims. This occurs even when only a moderate Le Fort III advancement is carried out. These lateral orbital stepoffs are visible to the casual observer as unattractive at conversational distance, and surgical attempts at modification performed later produce suboptimal results. Another problem with the Le Fort III osteotomy is the difficulty in judging an ideal orbital depth. This frequently results in either residual proptosis or enophthalmos. In addition, simultaneous correction of upper face (orbital) hypertelorism and the concave midface arc of rotation typical in Apert syndrome is not possible with the Le Fort III procedure. Excessive lengthening of the nose, accompanied by flattening of the nasofrontal angle, occurs if the Le Fort III osteotomy is selected when the skeletal dysmorphology favors an MB or FB procedure. Unfortunately, it is not possible to later correct the elongated nose or the flattened nasofrontal angle. Avoiding these shortcomings is not a matter of becoming more proficient at the Le Fort III osteotomy or simply managing the overlying soft tissues in a different way (i.e., canthopexies or midface lift). The Le Fort III osteotomy is not consistent with the presenting dysmorphology in most patients with craniosynostosis syndrome and therefore does not provide the opportunity to achieve the desired esthetic result. Nevertheless, the Le Fort III procedure often is considered the go-to approach by surgeons because (1) it is an extracranial procedure; (2) it requires less surgical skill and experience; (3) it is less likely to result in significant blood loss; and (4) it is less likely to result in perioperative complications (i.e., cranionasal fistula, intracranial abscess, bone resorption).
The osteotomy selected to manage the upper midface dysmorphology in the individual with a craniosynostosis syndrome (i.e., Le Fort III, MB, FB) should reflect the presenting skeletal deformities and provide a realistic opportunity for long-term esthetic enhancement of the upper midface (naso-orbito-malar) region.
In most patients with a craniosynostosis syndrome, a suboptimal esthetic result occurs if the surgeon attempts to simultaneously adjust the orbits and idealize the occlusion using the Le Fort III, monobloc, or facial bipartition osteotomy without completing a separate Le Fort I osteotomy. The degree of horizontal deficiency observed at the orbits and at the maxillary dentition are rarely uniform. If a Le Fort I osteotomy to separate the lower midface from the upper midface complex is not carried out, excess advancement at the orbits, with enophthalmos, is likely to occur as the surgeon attempts to achieve a positive overjet at the incisors. The Le Fort I osteotomy is generally not performed at the time of the upper midface procedure; it awaits skeletal maturity and is combined with orthodontic treatment. Until then, a degree of an angle class III anterior open bite negative overjet malocclusion remains. When the mature teenage or adult patient presents for surgical correction and requires both upper midface (i.e., naso-orbito-zygomatic) and lower midface (i.e., maxilla) management, the procedures may be carried out simultaneously.
Final reconstruction of the upper midface deformities in those born with a craniosynostosis syndrome can be managed as early as 7 to 10 years of age. By this age, the cranial vault and orbits normally attain approximately 85% to 90% of their adult size. Whenever feasible, waiting until the maxillary first molars have erupted is also preferred. When the upper midface reconstruction is carried out after approximately 7 years of age, the objective is to attain adult morphology in the cranio-orbito-zygomatic region with the expectation of a stable result (no longer influenced by growth) once healing has occurred. Psychosocial considerations also support the age range of 7 to 10 years for the upper midface procedure. When a successful reconstruction is achieved at this age, the child may progress through school with an opportunity for a healthy body image and self-esteem.
Monobloc and Facial Bipartition Osteotomies
The lack of consensus about the ideal timing and techniques for the management of complex upper midface malformations and deformities in craniosynostosis syndromes reflects not only uncertainty about the potential results with any one approach to treatment, but also confusion about how to perform these technically sensitive procedures.
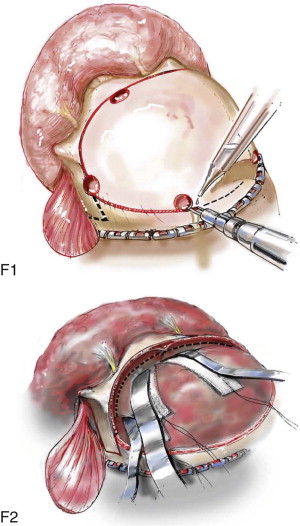
The following section provides the surgeon with a step-by-step technical description of the monobloc and facial bipartition osteotomies.
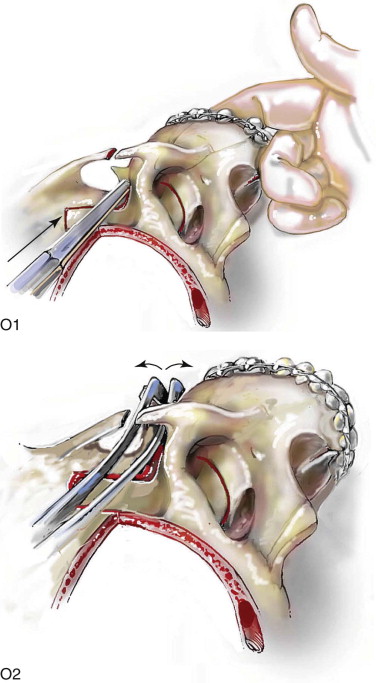
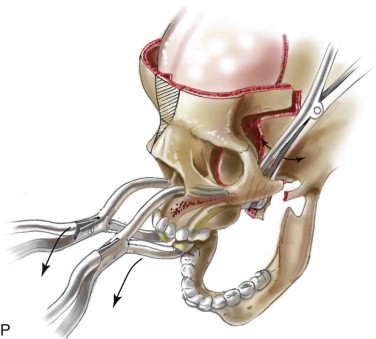
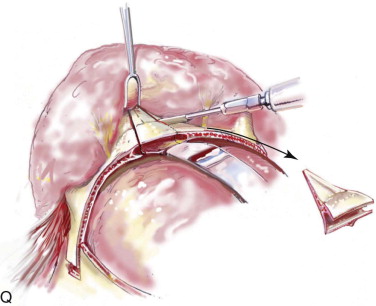
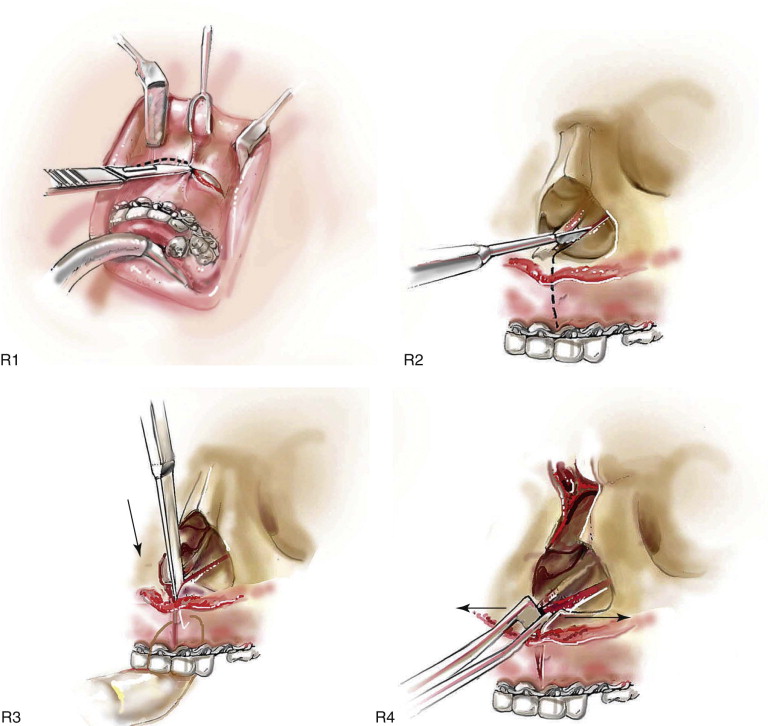
Technique: Monobloc and Facial Bipartition Osteotomies
Step 1:
Airway Management
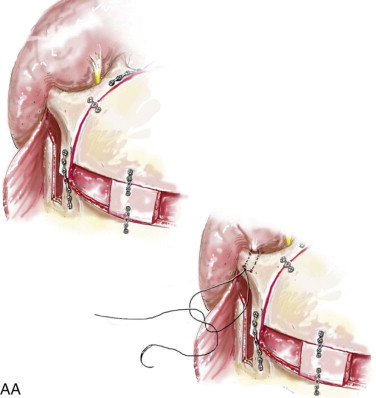
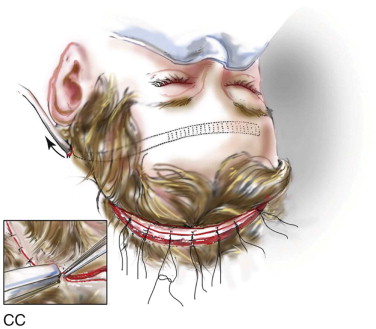
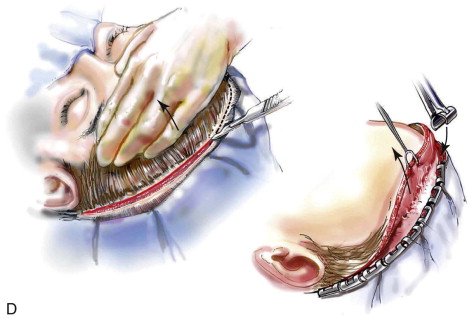
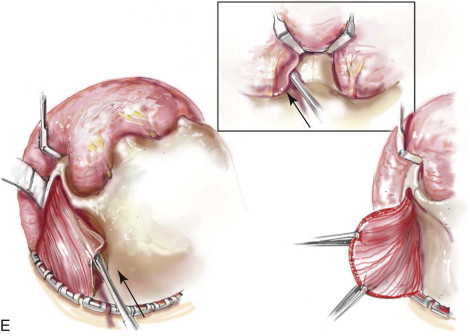
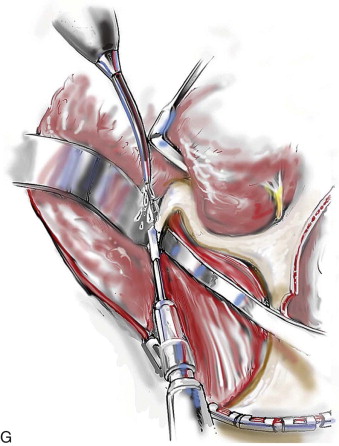
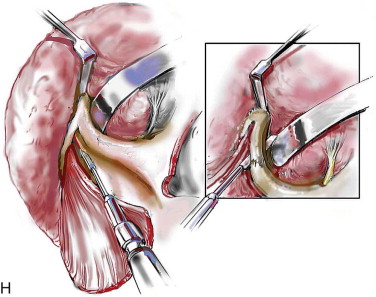
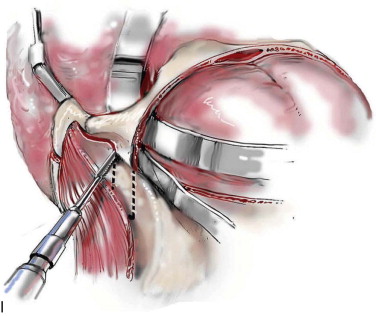
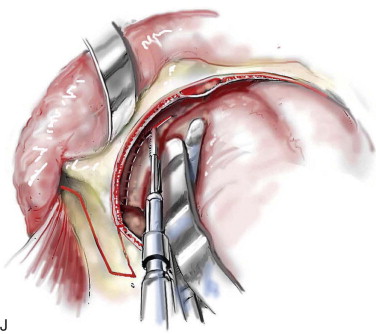
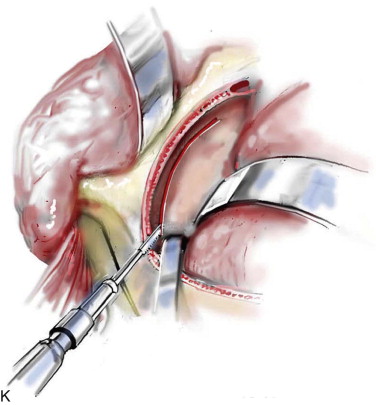
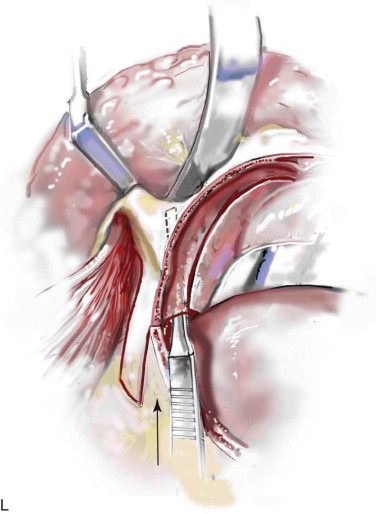
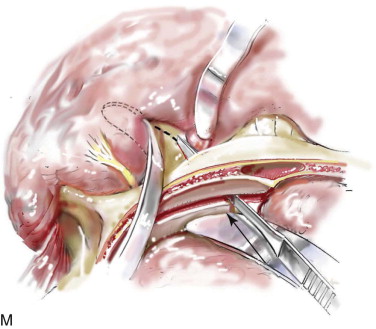
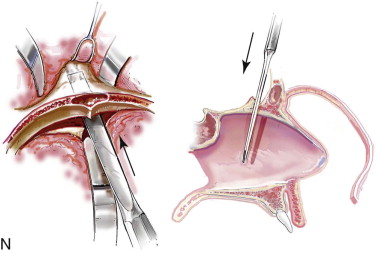
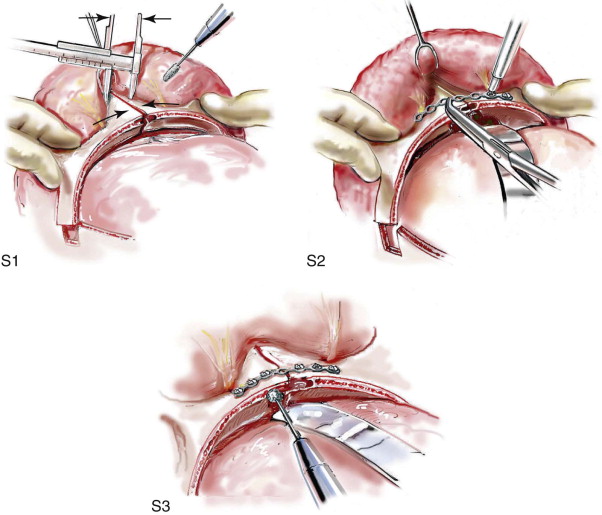
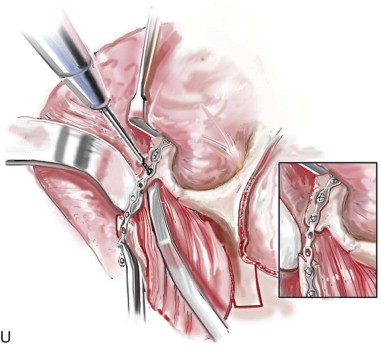
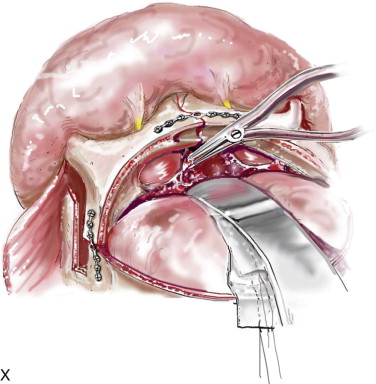
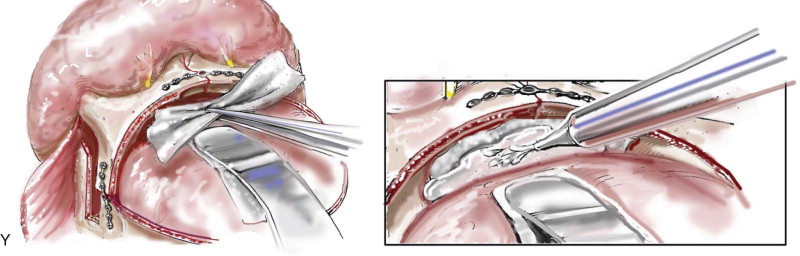
Satisfactory airway management in a patient undergoing an MB/FB osteotomy is essential. The method the authors’ use is an orotracheal tube secured adjacent to the cusp edge of the mandibular central incisors with a circummandibular wire. After the MB/FB osteotomies and disimpaction are complete, a nasotracheal tube is placed, and the orotracheal tube is removed. Through this controlled approach, endotracheal tube injury (at completion of the osteotomies) and/or dislodgment (during disimpaction) are prevented. Also, direct contact between the maxillary and mandibular teeth can be achieved for improved control of the occlusion. The nasotracheal tube remains in place at the end of the procedure to allow for nasal mucosal stenting during the initial postoperative phase. Other approaches to managing the airway have been described and used effectively (i.e., tracheostomy, submental intubation, and orotracheal intubation without exchange) ( Figure 48-4, A ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses