Armamentarium
|
History of the Procedure
Distraction osteogenesis has become a useful technique in the armamentarium for the correction of skeletal anomalies. In 1992, McCarthy and colleagues described the use of external distraction appliances for mandibular advancement in the management of hemifacial microsomia. Its application in the management of pediatric obstructive apnea appeared a few years later. In 1994, Moore and associates reported the management of obstructive sleep apnea with mandibular lengthening by distraction osteogenesis in a 6-year-old tracheostomy-dependent patient with Treacher Collins syndrome, with successful decannulation. Since then, many reports have documented the use of mandibular distraction for resolving airway obstruction, achieving early decannulation of tracheotomized children, and improving oral feeding.
In 1998, Cohen and colleagues reported on 16 patients who had undergone external mandibular distraction osteogenesis in conjunction with soft tissue procedures to treat medically refractory obstructive sleep apnea. In a group of eight tracheotomy-dependent patients, seven were successfully decannulated and the need for tracheotomy was averted in eight patients.
As experience with the technique increased, the use of distraction osteogenesis evolved from achieving decannulation in tracheotomy-dependent patients to the prevention of long-term airway support with continuous positive airway pressure (CPAP), nasopharyngeal tubes, or tracheotomy placement. Morovic and Monasterio performed mandibular distraction in seven patients, ranging in age from 1 to 18 months, with severe obstructive apnea secondary to mandibular hypoplasia, and two patients had tracheotomies. They reported the avoidance of a tracheotomy in five patients and achieved early decannulation in two tracheotomized patients in a group with congenital craniofacial malformations (five with Pierre Robin sequence and two with Treacher Collins syndrome). Denny and coworkers described their experience with mandibular distraction in neonates; they reported the resolution of upper airway obstruction and noted the importance of careful selection of patients. With time, the appliances were further developed with the introduction of small devices for intraoral pediatric mandibular distraction. In the first decade of the 21st century, a number of pediatric surgeons, such as Denny, Sidman, Smith, Chigurapati, and Monasterio, reported on the outcomes of the use of these appliances in neonates and infants. Mandibular distraction has since become a recognized approach in carefully selected neonatal and infant patients with severe upper airway obstruction secondary to micrognathia.
History of the Procedure
Distraction osteogenesis has become a useful technique in the armamentarium for the correction of skeletal anomalies. In 1992, McCarthy and colleagues described the use of external distraction appliances for mandibular advancement in the management of hemifacial microsomia. Its application in the management of pediatric obstructive apnea appeared a few years later. In 1994, Moore and associates reported the management of obstructive sleep apnea with mandibular lengthening by distraction osteogenesis in a 6-year-old tracheostomy-dependent patient with Treacher Collins syndrome, with successful decannulation. Since then, many reports have documented the use of mandibular distraction for resolving airway obstruction, achieving early decannulation of tracheotomized children, and improving oral feeding.
In 1998, Cohen and colleagues reported on 16 patients who had undergone external mandibular distraction osteogenesis in conjunction with soft tissue procedures to treat medically refractory obstructive sleep apnea. In a group of eight tracheotomy-dependent patients, seven were successfully decannulated and the need for tracheotomy was averted in eight patients.
As experience with the technique increased, the use of distraction osteogenesis evolved from achieving decannulation in tracheotomy-dependent patients to the prevention of long-term airway support with continuous positive airway pressure (CPAP), nasopharyngeal tubes, or tracheotomy placement. Morovic and Monasterio performed mandibular distraction in seven patients, ranging in age from 1 to 18 months, with severe obstructive apnea secondary to mandibular hypoplasia, and two patients had tracheotomies. They reported the avoidance of a tracheotomy in five patients and achieved early decannulation in two tracheotomized patients in a group with congenital craniofacial malformations (five with Pierre Robin sequence and two with Treacher Collins syndrome). Denny and coworkers described their experience with mandibular distraction in neonates; they reported the resolution of upper airway obstruction and noted the importance of careful selection of patients. With time, the appliances were further developed with the introduction of small devices for intraoral pediatric mandibular distraction. In the first decade of the 21st century, a number of pediatric surgeons, such as Denny, Sidman, Smith, Chigurapati, and Monasterio, reported on the outcomes of the use of these appliances in neonates and infants. Mandibular distraction has since become a recognized approach in carefully selected neonatal and infant patients with severe upper airway obstruction secondary to micrognathia.
Indications for the Use of the Procedure
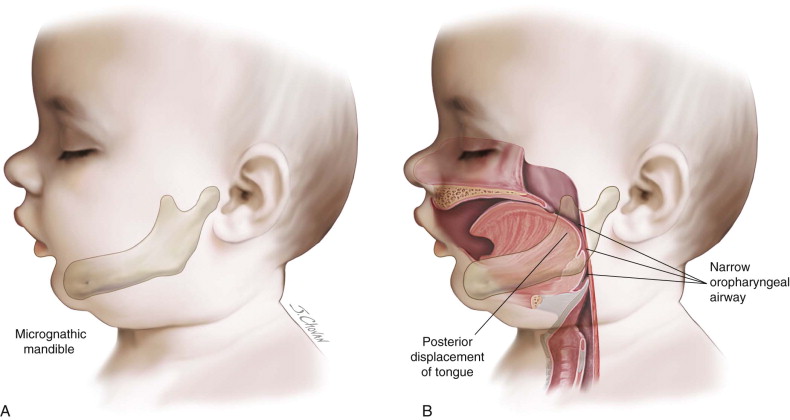
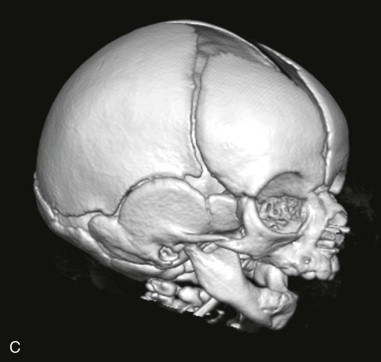
Infants and children with craniofacial syndromes, such as Pierre Robin sequence, Treacher Collins syndrome or craniofacial microsomia, and syndromic craniosynostosis, often present with varying degrees of upper airway obstruction (UAO). In these anomalies the micrognathic mandible is retropositioned, causing the posterior displacement of the tongue and a concomitant reduction of the oropharyngeal airway that leads to upper airway obstruction ( Figure 34-1 ). The degree of respiratory compromise may range from none to significant with potential morbidity and mortality. Abramson and colleagues demonstrated by 3D computerized tomography (CT) that distraction osteogenesis for the management of micrognathia increases airway size, decreases airway length, and alters the airway shape. Upper airway obstruction may result in disturbed sleep, daytime somnolence, and obstructive sleep apnea with the development of cor pulmonale and cardiac failure. An important relationship between airway obstruction and raised intracranial pressure (ICP) is also recognized. Studies have demonstrated that during apnea, elevations in ICP were observed and these elevations in pressure were only observed in relation to the apneic episodes. ICP, central perfusion pressure, and respiratory obstruction appear to interact in a vicious cycle. Obstructive sleep apnea (OSA) is also associated with reduced neurocognitive performance in children; however, the etiology is not fully elucidated. It has been proposed that neurocognitive deficits may be due to chronicity of OSA that is occurring at the time of rapid neurologic development. It has been reported that infants with obstructive apnea, compared to normal infants, have a higher incidence of abnormal neurologic development in the first year of life. In a study on older children (3 to 7 years), a relationship among sleep disordered breathing, increased cerebral blood flow and indices of cognition, and perhaps behavioral function was suggested, but the exact causal relationship has yet to be established.
These infants often have a concomitant failure to thrive, and the relationship among feeding difficulties, failure to thrive, and airway obstruction is now well known. Patients with craniofacial syndromes may present with multiple anomalies of the airway involving different parts of the tract. These abnormalities may include glossoptosis, tonsillar or adenoidal hypertrophy, narrowing of the nasopharynx, septal deviation, choanal atresia or stenosis, macroglossia, laryngotracheomalacia, subglottic stenosis, and tracheal anomalies. In addition, the role of central apnea needs to be carefully delineated. The increased sophistication of polysomnography investigations has been important in distinguishing the role of central apnea in the obstructive sleep apnea for some patients, and they may not be candidates for distraction as the underlying systemic condition will persist despite surgical intervention.
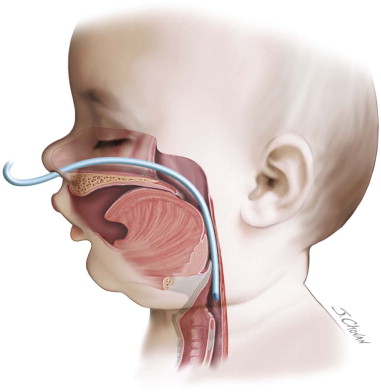
As the respiratory compromise may have multifactorial causes, a multidisciplinary team approach is essential for the comprehensive evaluation of the airway. This usually involves assessment by specialists in the fields of neonatal and pediatric medicine; respiratory and sleep medicine; ear, nose, and throat medicine; and craniomaxillofacial surgery. Potential investigations may include polysomnography, endoscopy or bronchoscopy, plain films, CT scan, reflux studies, and cardiac investigations, as well as electrocardiography (ECG) and echocardiogram. Depending on the severity of the UAO, a nasopharyngeal tube (NPT), which extends past the level of the tongue base in the oropharynx, may be inserted ( Figure 34-2 ). There is usually a trial of extubation of the NPT, and if UAO persists, the infant may be a candidate for mandibular distraction ( Figure 34-3 ).


In a small group of patients with Pierre Robin sequence, upper airway obstruction may develop following the closure of the cleft palate. It is speculated that these are borderline patients who are only able to maintain a patent airway with an unrepaired cleft palate. However, following a palate repair and the resultant change in the airway anatomy, obstructive sleep apnea symptoms develop, with a plateau or reduction in weight gain, and this requires management. Tonsillectomy and adenoidectomy are often first-line interventions, but mandibular distraction may need to be considered to manage UAO in these children.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


