Figures 82-1, 82-2, 82-3, 82-4, 85-5, 82-7C and D, 82-9, 82-10, 82-11, 82-12A to E, 82-13, 82-24, 82-25, 82-26 From Fonseca RJ, Marciani RD, Turvey TA: Oral and maxillofacial surgery, vol 3, ed 2, St Louis, Saunders, 2009.
Facial asymmetry can occur in all three planes of space: vertical, transverse, and anteroposterior (AP) and usually in combinations of these. Facial asymmetry can involve one or more of the following four anatomic areas: dentoalveolar, skeletal, soft tissues, and the temporomandibular joint (TMJ). Possible causative factors for facial asymmetry include genetics, birth molding, congenital and developmental deformities, abnormal growth, tumors or other pathology of facial structures and jaws, TMJ pathology, trauma, neurologic or neuromuscular disorders/pathology, and iatrogenic injury, among others. A comprehensive diagnosis, including identification of the causative factors, as well as an inclusive treatment plan that will provide optimal treatment outcomes, can be achieved through a thorough and complete workup including history, clinical, radiographic, and dental model analysis as well as MRI, CT scan, cone beam imaging, and the like when indicated.
Traditionally, facial asymmetry has been classified as either overdevelopment or underdevelopment of the facial structures. Because of the complexities and etiologies of facial asymmetries, a comprehensive classification may be impossible. Hundreds of known syndromes can cause facial asymmetry, so a discussion of all of them is beyond the scope of this chapter. This chapter focuses instead on the most common types of facial asymmetries, the diagnoses, evidence-based treatment, surgical options, and treatment outcomes.
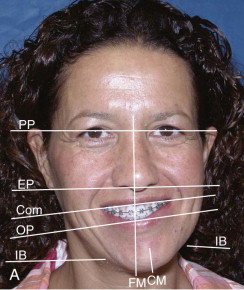
Facial asymmetry is usually the least at the cranial base level and increases at lower levels of the face, with the mandible and chin commonly exhibiting the greatest asymmetry. Exceptions include cranial and craniofacial deformities such as plagiocephaly, unilateral craniosynostosis, orbital dystopia, and tumors involving the cranium and midface. In most facial asymmetry cases, cranial base structures can be used as the base reference for determining the type and extent of the asymmetry affecting the midface and jaw structures ( Fig. 82-1 ). The presence of orbital dystopia, unequal pupillary heights, or unequal ear heights will make the assessment more challenging. Detailed methodology of the author’s comprehensive patient analysis and treatment planning has previously been published, with specifics for facial asymmetry, and will not be reiterated here.

TMJ and Facial Asymmetry
TMJ disorders and pathology are common causative factors for, or the result of, facial asymmetries. Certain TMJ pathologies can produce a progressive worsening of the facial asymmetry and malocclusion, from minimal change to 4 to 5 mm or more per year depending on the nature of the pathology. Other TMJ conditions may only cause pain or dysfunction without worsening facial asymmetry, but may still need to be addressed for optimal pain relief, stability, and good functional and esthetic treatment outcomes. Condylar underdevelopment or condylar resorption can cause the mandible and face to be smaller on one side and shift toward that side. On the other hand, a unilateral condyle enlargement can cause overdevelopment of the mandible and associated structures, causing facial asymmetry. Performing orthognathic surgery only and ignoring the TMJ pathology during treatment or failure to render proper TMJ management for the specific pathology could result in the asymmetry and malocclusion redeveloping with worsening TMJ-associated symptoms including jaw dysfunction and pain. The TMJs should always be evaluated in patients with facial asymmetry to determine if they are the etiologic factor, a problem that has developed because of facial asymmetry, a coexisting pretreatment condition, or normal and healthy joints.
Number and Type of Previous Surgeries
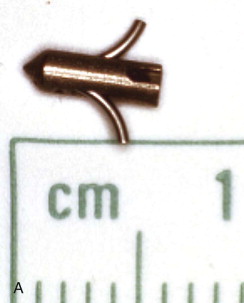
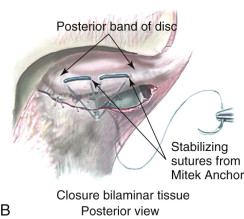
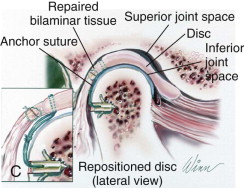
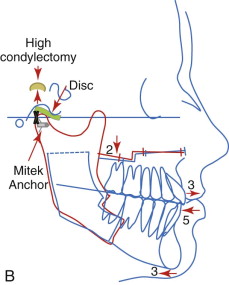
The number of previous surgeries, particularly to the TMJ, may dictate the TMJ surgical procedure options. For example, patients with articular disc dislocation, with 0 to 1 previous TMJ surgeries, and without significant other joint or systemic disease involvement may benefit from articular disc repositioning and ligament repair with Mitek anchors (Mitek Products Inc., Westwood, Mass) to achieve a stable treatment outcome ( Fig. 82-2 ).
A patient with two or more previous TMJ surgeries will have a high failure rate if autogenous tissues are used for the TMJ reconstruction. A patient-fitted TMJ total joint prosthesis, such as the TMJ Concepts system (TMJ Concepts Inc., Ventura, Calif) will have a much higher rate of success (see Fig. 82-13, B ). End-stage TMJ conditions, such as connective tissue/autoimmune diseases, severe arthritis, ankylosis, severe TMJ damage from trauma, and failed TMJ alloplastic implants, will get the most predictable results with patient-fitted total joint prostheses and fat grafts packed around the articulating components of the prostheses.
Age for Surgical Intervention
Some facial asymmetry conditions may get worse with growth and development. Predictability of results and limiting correction of the jaw and TMJ-related deformities to one major operation can usually best be achieved by waiting until growth is relatively complete. Although there are individual variations, females usually have the majority of their facial growth (98%) complete by the age of 15 years and males by the age of 17 to 18 years. Performing surgery at earlier ages may result in the need for additional surgery at a later time to correct asymmetry and malocclusion that may develop during the completion of growth. There are definite indications for early surgery, such as ankylosis, growth center transplants (i.e., sternoclavicular or rib grafts), masticatory dysfunction, tumor removal, and airway obstruction. Wolford et al. have published reports on maxillary and mandibular surgery and the effects on growth, with guidelines for age when considering surgical intervention.
For simplicity, facial asymmetry can be divided into four categories: (1) pseudo-asymmetry, (2) nonpathologic facial asymmetry, (3) unilateral overdevelopment, and (4) unilateral underdevelopment/degeneration.
Pseudo-Asymmetry
Some patients may have pseudo-asymmetry where the mandible is postured asymmetrically toward one side with one condyle displaced forward relative to the centric relation position in the fossa, usually caused by occlusal interferences, neuromuscular dysfunction, habitual posturing, condylar dislocation, and the like ( Fig. 82-3, A, B ). Pseudo-asymmetry can also be caused by temporary unilateral facial swelling as a result of conditions such as facial trauma or infection, where the asymmetry resolves as the swelling dissipates. The most common pseudo-asymmetry conditions are discussed next.




Malocclusion
Malocclusion may be the result of occlusal interferences in a TMJ centric relation position causing the mandible to shift toward one side for a better or more comfortable occlusal fit with one condyle postured forward in the fossa. These patients will exhibit a facial asymmetry with the mandible and chin shifted toward the contralateral side. Intraorally, there will be a class III occlusion on the side where the condyle is postured forward and a crossbite on the contralateral side. The facial, occlusal, and imaging appearance will be similar to the patient in Fig. 82-3, A, B . These patients may be asymptomatic, but some may experience muscle or TMJ pain and headaches. The mandible can usually be shifted into a TMJ centric relation position with elimination of the facial asymmetry, but occlusal interferences may be present. Imaging will demonstrate a unilateral condyle postured forward in the fossa, similar to Fig. 82-4, A . Orthodontics and when indicated orthognathic surgery will usually correct the malocclusion.

Neuromuscular Dysfunction (Dystonia)
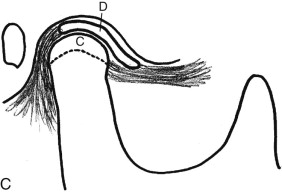
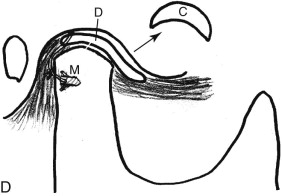
A unilateral neuromuscular hyperfunction commonly involves the lateral pterygoid muscle, although other muscles can be contributory. The stimulus may be derived from malocclusion, neuromuscular disorder, myofascial pain, myositis, muscle spasm, reflex splinting, psychogenic origin, nutritional and electrolyte imbalances, drug induced, and so on. The onset is usually relatively sudden with muscle dysfunction on one side that displaces one condyle forward in the fossa and shifts the mandible off toward the opposite side, creating facial asymmetry (see Figs. 82-3, A , B and 82-4, A ). These patients often experience pain, class III occlusal relation on the involved side, crossbite on the opposite side, and decreased range of motion. The mandible can usually be positioned into a TMJ centric relation position eliminating the facial asymmetry, but it likely won’t stay there until the etiologic factors are resolved and muscles relaxed. Effective treatment methods may include muscle relaxants, ant-seizure medications, physical therapy, psychological intervention, eminoplasty, eminectomy, myotomy, Botox injections, Mitek anchor technique ( Fig. 82-3, C , D ), and so on.
Condylar Dislocation
Condylar dislocation occurs when the ligaments that normally keep the condyle within a normal functional range are ineffective because of laxity (i.e., cutis laxa, Ehlers-Danlos syndrome), stretched, torn, herniated, or degenerated. Condylar hypermobility or muscle dysfunction pulls the condyle anterior to the articular eminence where it may become locked. A unilateral anteriorly dislocated condyle shifts the mandible toward the opposite side. This can be a sudden onset or a chronic occurring condition, creating a significant functional impairment, facial deformity, malocclusion, and pain. The malocclusion will present as a class III relation on the involved side and a crossbite on the opposite side. The clinical appearance will be similar but more exaggerated compared to the patient in Fig. 82-3, A , B . Reduction and placing the condyle in a TMJ centric relation position will eliminate the facial asymmetry.
Radiographic imaging will show a unilateral condyle dislocated anterior to the articular eminence ( Fig. 82-4, B ). The dislocated condyle may reduce spontaneously or require physical manipulation back into the fossa. Medications, myotomy, eminectomy, eminoplasty, augmentation of eminence, sclerosing agents, Botox injection, and Mitek anchor technique are treatments that have been advocated to manage this condition when it is recurrent.
Infection
Unilateral facial swelling can be caused by a bacterial or viral infection of dental structures, bones, soft tissues, glands, spaces, implanted devices, or foreign bodies. A unilateral infection usually presents with facial swelling, relatively quick onset, pain, induration, erythema, febrile, purulence, malaise, and increased white blood cell count.
Radiographic imaging such as MRI, CT scan, cone beam, or other imaging technology usually shows evidence of dental, bone, soft tissue, gland, implant, or foreign body involvement.
Treatment may include incision and drainage; culture and sensitivity; debridement and removal of infected teeth, hard and soft tissue structures, devices, or foreign bodies; irrigation; and antibiotics and other medications or therapy as indicated. With proper treatment, resolution of the infection and asymmetry should be expected.
Pseudo-Asymmetry
Some patients may have pseudo-asymmetry where the mandible is postured asymmetrically toward one side with one condyle displaced forward relative to the centric relation position in the fossa, usually caused by occlusal interferences, neuromuscular dysfunction, habitual posturing, condylar dislocation, and the like ( Fig. 82-3, A, B ). Pseudo-asymmetry can also be caused by temporary unilateral facial swelling as a result of conditions such as facial trauma or infection, where the asymmetry resolves as the swelling dissipates. The most common pseudo-asymmetry conditions are discussed next.




Malocclusion
Malocclusion may be the result of occlusal interferences in a TMJ centric relation position causing the mandible to shift toward one side for a better or more comfortable occlusal fit with one condyle postured forward in the fossa. These patients will exhibit a facial asymmetry with the mandible and chin shifted toward the contralateral side. Intraorally, there will be a class III occlusion on the side where the condyle is postured forward and a crossbite on the contralateral side. The facial, occlusal, and imaging appearance will be similar to the patient in Fig. 82-3, A, B . These patients may be asymptomatic, but some may experience muscle or TMJ pain and headaches. The mandible can usually be shifted into a TMJ centric relation position with elimination of the facial asymmetry, but occlusal interferences may be present. Imaging will demonstrate a unilateral condyle postured forward in the fossa, similar to Fig. 82-4, A . Orthodontics and when indicated orthognathic surgery will usually correct the malocclusion.

Neuromuscular Dysfunction (Dystonia)
A unilateral neuromuscular hyperfunction commonly involves the lateral pterygoid muscle, although other muscles can be contributory. The stimulus may be derived from malocclusion, neuromuscular disorder, myofascial pain, myositis, muscle spasm, reflex splinting, psychogenic origin, nutritional and electrolyte imbalances, drug induced, and so on. The onset is usually relatively sudden with muscle dysfunction on one side that displaces one condyle forward in the fossa and shifts the mandible off toward the opposite side, creating facial asymmetry (see Figs. 82-3, A , B and 82-4, A ). These patients often experience pain, class III occlusal relation on the involved side, crossbite on the opposite side, and decreased range of motion. The mandible can usually be positioned into a TMJ centric relation position eliminating the facial asymmetry, but it likely won’t stay there until the etiologic factors are resolved and muscles relaxed. Effective treatment methods may include muscle relaxants, ant-seizure medications, physical therapy, psychological intervention, eminoplasty, eminectomy, myotomy, Botox injections, Mitek anchor technique ( Fig. 82-3, C , D ), and so on.
Condylar Dislocation
Condylar dislocation occurs when the ligaments that normally keep the condyle within a normal functional range are ineffective because of laxity (i.e., cutis laxa, Ehlers-Danlos syndrome), stretched, torn, herniated, or degenerated. Condylar hypermobility or muscle dysfunction pulls the condyle anterior to the articular eminence where it may become locked. A unilateral anteriorly dislocated condyle shifts the mandible toward the opposite side. This can be a sudden onset or a chronic occurring condition, creating a significant functional impairment, facial deformity, malocclusion, and pain. The malocclusion will present as a class III relation on the involved side and a crossbite on the opposite side. The clinical appearance will be similar but more exaggerated compared to the patient in Fig. 82-3, A , B . Reduction and placing the condyle in a TMJ centric relation position will eliminate the facial asymmetry.
Radiographic imaging will show a unilateral condyle dislocated anterior to the articular eminence ( Fig. 82-4, B ). The dislocated condyle may reduce spontaneously or require physical manipulation back into the fossa. Medications, myotomy, eminectomy, eminoplasty, augmentation of eminence, sclerosing agents, Botox injection, and Mitek anchor technique are treatments that have been advocated to manage this condition when it is recurrent.
Infection
Unilateral facial swelling can be caused by a bacterial or viral infection of dental structures, bones, soft tissues, glands, spaces, implanted devices, or foreign bodies. A unilateral infection usually presents with facial swelling, relatively quick onset, pain, induration, erythema, febrile, purulence, malaise, and increased white blood cell count.
Radiographic imaging such as MRI, CT scan, cone beam, or other imaging technology usually shows evidence of dental, bone, soft tissue, gland, implant, or foreign body involvement.
Treatment may include incision and drainage; culture and sensitivity; debridement and removal of infected teeth, hard and soft tissue structures, devices, or foreign bodies; irrigation; and antibiotics and other medications or therapy as indicated. With proper treatment, resolution of the infection and asymmetry should be expected.
Nonpathologic Facial Asymmetry
Nonpathologic, nonsyndrome developmental facial asymmetry most commonly occurs as a result of genetics, intrauterine molding, or natural growth variance. The asymmetry is usually present at birth, but it may not be identified until later depending on the severity of the deformity. Growth usually maintains the asymmetry and does not get significantly worse. The occlusion (although it can be class I, II, or III) remains relatively constant. The extent of the deformity stops at completion of growth providing no TMJ pathology develops during the growth process. These deformities are usually less severe in degree of asymmetry and symptoms as compared to those that involve TMJ pathology. Some cases may demonstrate an asymmetry involving just the dental alveolus with the rest of the face being relatively symmetric.
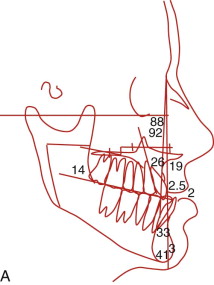
Lateral and AP cephalometric radiographic analysis may show vertical asymmetry at the occlusal plane and mandibular inferior border and ramus. TMJ condyles may be relatively equal in size and shape without evidence of TMJ pathology or one condyle may be somewhat smaller but the proportion between the condyles should remain constant during growth. Orthodontics and orthognathic surgery may be required to correct skeletal and occlusal imbalances. Surgical treatment should be delayed until facial growth is essentially complete, particularly if maxillary surgery is required. Unilateral facial augmentation of hard or soft tissues may be necessary to optimize the treatment results.
Dentoalveolar Asymmetry
Dentoalveolar asymmetry can involve the alveolar bone, teeth, and gingiva. Missing, unerupted, or ankylosed teeth, partial anodontia, unilateral alveolar or palatal clefts, radiation, tumor involvement, and abnormal growth, among other factors, can contribute to asymmetry. Ankylosed teeth can be induced by genetics, trauma, inflammation, excessive orthodontic forces, and so on as the catalyst for the bone to root fusion causing an adverse effect on dentoalveolar growth and development. Unilateral dentoalveolar asymmetry can include unilateral crossbite, buccal or lingual ( Fig. 82-5, A ); unilateral open bite or deep bite; transverse cant in the occlusal plane; AP, vertical, or transverse dental arch asymmetry; and so on.


Orthodontics is usually a necessary part of treatment and in some cases can correct the asymmetry. However, dentoalveolar surgery and orthognathic surgery may also be required, as well as restorative dentistry to obtain the best results ( Fig. 82-5, B ). Ankylosed teeth will act as an anchor, and if the involved tooth is out of alignment and tied into the orthodontic arch wire, the adjacent teeth will be displaced toward the malaligned ankylosed tooth. Treatment options for ankylosed teeth include luxating the ankylosed tooth (teeth) and immediate orthodontics or distraction, crowning, extraction with replacement, or osteotomies with single tooth or multiple teeth segments for repositioning or distraction. Dental implants and restorative dentistry can restore missing, decayed, and deformed teeth.
Overdevelopment
Unilateral overdevelopment of the face can cause significant facial asymmetry, with the most common conditions including (1) condylar hyperplasia, (2) unilateral muscle hyperplasia, (3) tumors, and (4) neurologic and neuromuscular disorders. As each of these pathologic conditions requires specific treatment protocols, it is important to have an accurate diagnosis.
Condylar hyperplasia (CH) refers to enlargement or overgrowth of the mandibular condyle. Several etiologies cause CH. Wolford has developed a simple classification system based on the specific pathology and rate of occurrence. CH type 1 refers to an accelerated and often prolonged overgrowth of the “normal” growth center of the condyle. CH type 1A refers to the bilateral condition, as it is the most commonly occurring form of CH, and CH type 1B refers to the unilateral form of the pathology. CH type 2 refers to the most common benign unilateral tumors, with CH type 2A designating osteochondromas and CH type 2B referring to osteomas. CH type 3 refers to any other pathology that causes condylar enlargement, with CH type 3A being other benign tumors and CH type 3B referring to malignant tumors.
Condylar Hyperplasia (Ch Type 1)
CH type 1 is a pathologic condition affecting the “normal” condylar growth center, causing an accelerated and prolonged overdevelopment of the mandible and creating mandibular prognathism and esthetic deformity ( Fig. 82-6, A-F ). CH type 1 usually begins during the pubertal growth phase, and the mandible can continue to grow at an accelerated rate but the growth is self-limiting and usually stops when affected individuals are in their mid-20s. These patients usually begin with a class I skeletal and occlusal relationship and develop into a class III relationship, or start as class III but develop a worse class III relationship as the mandible grows predominantly in a horizontal direction, although sometimes there can be a vertical growth vector. Asymmetry of the mandible can occur by unilateral (CH type 1B) or bilateral CH (CH type 1A) where one condyle grows faster than the opposite side. In this situation, the mandible becomes deviated toward the contralateral side; there is a class III occlusion on the ipsilateral side and a crossbite on the contralateral side; the mandible, mandibular dental midline, and chin are shifted toward the contralateral side; the mandible continues to grow asymmetrically beyond the normal growth years but usually will complete its development when these individuals are in their mid-20s. Disc displacement may occur on the “normal” contralateral side from increased joint loading created by the ipsilateral CH.


Although the condyle usually retains a relatively normal architecture, there is an increased length of the condylar head, neck, and mandibular body ( Fig. 82-7, A ). The normal pubertal growth rate from condylion to point B in females is a mean of 1.6 mm per year, with 98% of growth complete by the age of 15 years. Males grow at a mean rate of 2.2 mm per year, with 98% of growth complete by the age of 17 to 18 years. The identification of sex hormone receptors in and around the TMJ and the pubertal onset of CH type 1 are strongly suggestive of a hormonal influence in the etiology. However, trauma, infection, heredity, intrauterine factors, and hypervascularity, have also been implicated as causative factors. Approximately one third of bilateral CH cases have a familial history.
Histologic observations of CH type 1 condyles may appear similar to normal bony architecture, but in some cases the proliferative layer may demonstrate greater thickness in some areas and less in others; however cartilage-producing cells may be prevalent at its lower border. In normal condyles, the formation of cartilage from the proliferative layer and the replacement of cartilage by bone cease by approximately 20 years of age. The marrow cavity is entirely occluded from the remaining cartilage by the closure of the bone plate. The inability of this plate to close in the presence of an active proliferative cartilage layer may be a major etiologic factor in CH type 1.
Bone scans may not be of value in diagnosing CH type 1 because the growth rate is slow and continuous so there may not be much differentiation in the amount of isotope uptake compared to a normal joint. MRI may show a displaced articular disc on the contralateral side and sometimes on the ipsilateral side. Serial radiographs (lateral cephalograms, cephalometric TMJ tomograms), dental models, and clinical evaluations are usually the most advantageous methods to determine if the growth process is still active.
Treatment of this deformity varies depending on whether the growth is still active. If jaw growth has stopped, orthognathic surgical procedures can usually be performed to correct the asymmetry and malocclusion. However, if the patient is still a teenager or even in his or her early 20s, the growth process can be active and progressive. If there is confirmed active growth, then there are two predictable treatment options. The most predictable option is to perform a high condylectomy, removing 4 to 5 mm of the top of the condylar head on the involved side (both sides for bilateral CH), reposition the articular disc over the remaining condyle using the Mitek anchor technique ( Fig. 82-7, C , D ), and perform the appropriate orthognathic surgery to correct the associated dentofacial deformity ( Fig. 82-7, B ). This can be done in one operation or divided into two operations, but the TMJ surgery must be performed first. This is a highly predictable treatment that will stop mandibular growth with long-term stable functional and esthetic outcomes ( Fig. 82-6, G-L ). The recommended age for unilateral CH surgery is 15 years for females and 17 years for males. Performing a unilateral high condylectomy earlier will result in arresting the growth on the CH side, but the normal side can continue to grow until normal cessation occurs, with the potential of causing asymmetry by the mandible shifting toward the original CH side.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


