* DISCLAIMER: The views expressed in this article are those of the author and do not reflect the official policy of the Department of Navy, Department of Defense, or U.S. government.
Armamentarium
|
History of the Procedure
Frontal sinus fractures present a unique challenge in the management and treatment of craniomaxillofacial trauma. The earliest reports of frontal sinus fracture management involved the complete removal of the anterior table and, if involved, the posterior table. The forehead skin was then allowed to collapse down on to the posterior table if it remained, or it collapsed on to the dura if both tables had been removed. Although this effectively sealed the nasal cavity from the frontal sinus, it resulted in undesirable aesthetics and contour deformities. Modifications of this ablative procedure followed as surgeons attempted to improve cosmetic outcomes. In the 1950s, Bergara and Bergara described an approach that required an osteoplastic flap. Their technique involved creating a window into the frontal sinus through the anterior table, which was hinged off an inferiorly based pericranial pedicle flap. After visualizing and removing damaged elements of the sinus, the bone flap was replaced, restoring forehead contour. Goodale and Montgomery later popularized the addition of frontal sinus obliteration with autologous fat, thereby eliminating the functional sinus unit. In 1978, Donald and Bernstein described the cranialization procedure. They advocated complete removal of the posterior sinus table and ablation of the sinus in cases involving significant comminution or displacement of the posterior table with a persistent cerebrospinal fluid (CSF) leak. More recently, authors have emphasized the condition of the nasofrontal outflow tracts as a major factor in management algorithms. Regardless of the treatment modality, the goal of frontal sinus fracture management continues to revolve around the restoration of the anterior table form, nasofrontal outflow tract function, and prevention of complications.
History of the Procedure
Frontal sinus fractures present a unique challenge in the management and treatment of craniomaxillofacial trauma. The earliest reports of frontal sinus fracture management involved the complete removal of the anterior table and, if involved, the posterior table. The forehead skin was then allowed to collapse down on to the posterior table if it remained, or it collapsed on to the dura if both tables had been removed. Although this effectively sealed the nasal cavity from the frontal sinus, it resulted in undesirable aesthetics and contour deformities. Modifications of this ablative procedure followed as surgeons attempted to improve cosmetic outcomes. In the 1950s, Bergara and Bergara described an approach that required an osteoplastic flap. Their technique involved creating a window into the frontal sinus through the anterior table, which was hinged off an inferiorly based pericranial pedicle flap. After visualizing and removing damaged elements of the sinus, the bone flap was replaced, restoring forehead contour. Goodale and Montgomery later popularized the addition of frontal sinus obliteration with autologous fat, thereby eliminating the functional sinus unit. In 1978, Donald and Bernstein described the cranialization procedure. They advocated complete removal of the posterior sinus table and ablation of the sinus in cases involving significant comminution or displacement of the posterior table with a persistent cerebrospinal fluid (CSF) leak. More recently, authors have emphasized the condition of the nasofrontal outflow tracts as a major factor in management algorithms. Regardless of the treatment modality, the goal of frontal sinus fracture management continues to revolve around the restoration of the anterior table form, nasofrontal outflow tract function, and prevention of complications.
Indications for the Use of the Procedure
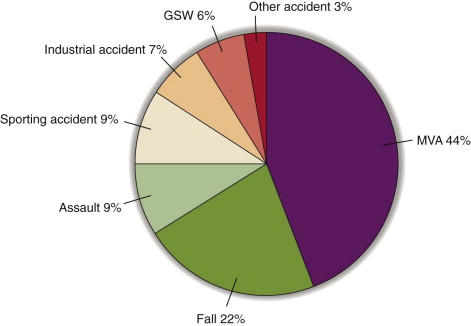
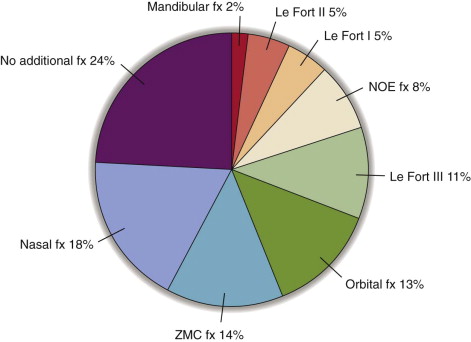
Frontal sinus fractures rarely occur in isolation. Approximately 70% are associated with other maxillofacial injuries. With motor vehicle accidents as the most common mechanism of injury, initial evaluation of the patient with a suspected frontal sinus fracture follows an advanced trauma life support protocol, and life-threatening injuries are addressed first. Patients with multisystem injuries and head trauma are often intubated and sedated. In these cases, a detailed history of the mechanism of injury and incident scene must be obtained from law enforcement officials and emergency medical services personnel, and the patient’s past medical history comes from the patient’s family. In one series, only 24% of patients were conscious, 42% were comatose, and 52% had accompanying shock. A range of 800 to 2200 pounds of force is required to cause a frontal sinus fracture. Bell and colleagues summarized the mechanism of injury and concomitant injuries found with frontal sinus fractures ( Figures 78-1 and 78-2 ). Isolated anterior table injuries account for 43% to 61% of frontal sinus injuries, 0.6% to 6% are isolated posterior table injuries, and 19% to 51% have combined anterior and posterior table injuries. Between 2.5% and 21% of frontal sinus injuries involve the nasofrontal outflow tract. Associated intracranial injuries range from 31% to 76%, and approximately 21% present with an associated ophthalmologic injury ( Table 78-1 ). As a testament to the significant force necessary to fracture the frontal sinus, following initial stabilization and subsequent frontal sinus fracture treatment, 25% of the patients succumbed due to concomitant injuries within 2 weeks of their initial surgery.
| Injury | NFOT Uninjured | NFOT Injured |
|---|---|---|
| Orbital roof | 13% | 40% |
| Orbital wall | 7% | 13% |
| Orbital floor | 2% | 7% |
| NOE | 12% | 31% |
| Zygoma | 8% | 18% |
| Le Fort | 2% | 17% |
| Mandible | 3% | 5% |
| Intercranial | 31% | 76% |
| Cervical spine | 7% | 14% |
| Upper extremity fracture | 15% | 25% |
| Lower extremity fracture | 13% | 23% |
| Pneumothorax | 12% | 24% |
| Abdominal | 7% | 13% |
Evaluation and Diagnosis
When evaluating frontal sinus trauma, specific attention must be paid to potential intracranial injury. Specific clinical findings may include a palpable bony step, a contour deformity, crepitus, and mobility of bone segments. If the patient is conscious, discovery of a paresthesia or anesthesia of the forehead and scalp may be present due to injury of the supraorbital nerves. Close attention should also be paid to the naso-orbito-ethmoid region for injuries that may contribute to sinus outflow tract dysfunction or obstruction. Rhinorrhea or otorrhea, when present, can have multiple causes and may indicate a CSF leak. The “halo” test can be used as a screening tool to detect the presence of CSF. When the fluid is placed on a piece of filter paper, gauze, or linen, a ring of clear CSF will surround a central component of blood. This is due to the differing diffusion rates of blood and CSF. Alternatively, the fluid can be tested for glucose and chloride in an attempt to differentiate among CSF, serum, and nasal secretions. In comparison to blood/serum and nasal secretions, CSF has a higher concentration of glucose and a lower concentration of chloride. This method has a low sensitivity and specificity for accuracy, so false-positive results lead to inconsistency in distinguishing among CSF, blood/serum, and nasal secretions. The most accurate confirmation of CSF is made by testing the fluid for β-2 transferrin. This laboratory test can take up to 4 days to process; therefore, it should not cause an unwanted delay in fracture diagnosis and treatment. Reports exist of β-2 transferrin being contained in aqueous humor and the serum of patients with alcohol-related chronic liver disease. This must be considered, especially in cases of maxillofacial trauma and in the patient with a ruptured globe.
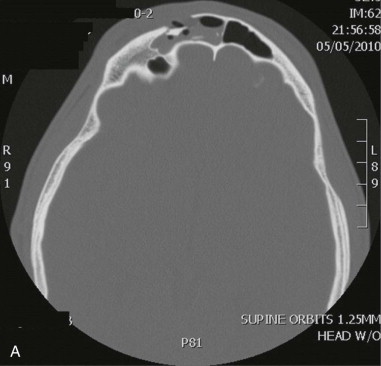
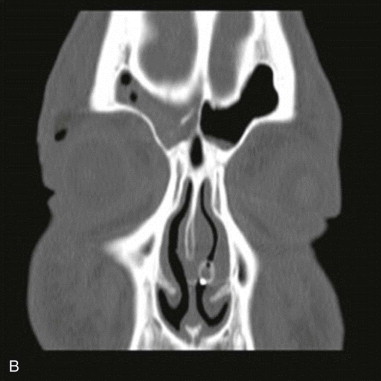
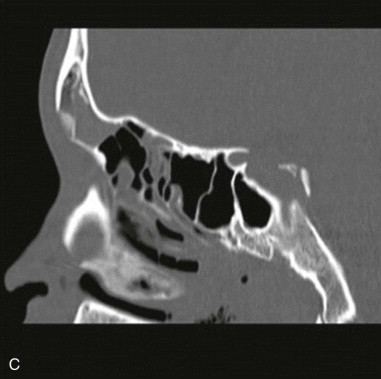
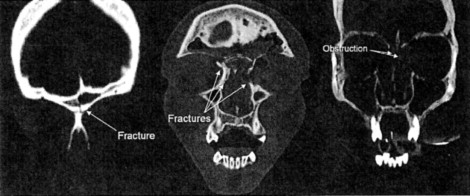
Ultrasound may be used as a screening tool when evaluating for frontal sinus fractures. It is most useful for visualization of the zygomatic arch and the anterior table of the frontal sinus. If a fracture is suspected following ultrasound screening, further imaging is indicated. Imaging via computed tomography (CT) in axial, coronal, and sagittal planes has revolutionized the diagnosis and management of frontal sinus injuries ( Figure 78-3 ). Whenever a frontal sinus injury is suspected, a high-resolution noncontrasted CT scan with 1- to 1.5-mm cuts should be performed. Axial slices will best evaluate the anterior and posterior tables of the sinus. The location of the fractures, amount of displacement, and degree of comminution are readily seen in this plane. Coronal slices are useful for evaluating the sinus floor, orbital roof, and anterior ethmoid cells, whereas sagittal slices provide valuable information about the nasofrontal outflow tract (NFOT). NFOT obstruction has been incorporated into several of the current treatment algorithms for fontal sinus injury. NFOT injury or obstruction is typically assessed intraoperatively under direct visualization, with or without the use of a sterile colored fluid introduced into the NFOT system. However, some authors have correlated CT evidence of NFOT injury findings directly into their treatment algorithm. Stanwix and coworkers defined NFOT injury by at least one of the following criteria found on CT: fracture of the sinus floor, fracture of the medial aspect of the anterior table (anterior ethmoid cells), or outflow tract/duct obstruction ( Figure 78-4 ). Obstruction is defined as a segment of fractured bone lying partially or entirely within the outflow tract.
Limitations and Contraindications
The anatomic proximity of the frontal sinus to the brain, orbit, ethmoid sinus, and nasal cavity increases the potential morbidity and treatment complexity associated with treatment and repair of these injuries. Mismanagement, delayed treatment, or insufficient follow-up can lead to serious, life-threatening complications including meningitis, mucopyocele, pneumocephalus, and brain abscess. To date, there is no consensus on a single management algorithm. This is largely due to the lack of prospective randomized clinical trials addressing different treatment modalities, which are neither feasible nor ethical. Since the early 1900s and despite the lack of consensus, there have been major advances in the treatment of frontal sinus injuries.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


