Armamentarium
| The inverted L osteotomy can be performed either extraorally or intraorally. The equipment for these two options is slightly different. For the purpose of this chapter, the instruments for the extraoral approach are listed first and then the separate instruments used for the intraoral procedure. |
| Extraoral Approach |
|
| Intraoral Approach |
|
History of the Procedure
According to Steinhauser, the inverted L osteotomy was first described by Trauner in 1955. In 1957 and 1958, Schuchardt and then Immenkamp suggested the use of an autogenous corticocancellous bone graft between the proximal and distal segments. The extraoral technique described by Speissl in his 1989 textbook is very similar to what is used today.
In 1990, Van Sickels et al discussed the rigid fixation of the intraoral inverted L osteotomy. Although this was not the first report of the intraoral inverted L osteotomy (ILO), it appears to have been the earliest report of the use of rigid fixation with the ILO, which reduced the need for longer periods of maxillary-mandibular fixation. The rigid fixation technique described by Van Sickels et al was used for mandibular setbacks. It used a condylar positioning device to control the proximal segments during surgery. In 1999, McMillan et al published a paper on the intraoral inverted L osteotomy and referenced a 1993 conference in Australia, where the technique was presented. The technique was presented as an option to also advance the mandible.
History of the Procedure
According to Steinhauser, the inverted L osteotomy was first described by Trauner in 1955. In 1957 and 1958, Schuchardt and then Immenkamp suggested the use of an autogenous corticocancellous bone graft between the proximal and distal segments. The extraoral technique described by Speissl in his 1989 textbook is very similar to what is used today.
In 1990, Van Sickels et al discussed the rigid fixation of the intraoral inverted L osteotomy. Although this was not the first report of the intraoral inverted L osteotomy (ILO), it appears to have been the earliest report of the use of rigid fixation with the ILO, which reduced the need for longer periods of maxillary-mandibular fixation. The rigid fixation technique described by Van Sickels et al was used for mandibular setbacks. It used a condylar positioning device to control the proximal segments during surgery. In 1999, McMillan et al published a paper on the intraoral inverted L osteotomy and referenced a 1993 conference in Australia, where the technique was presented. The technique was presented as an option to also advance the mandible.
Indications for the Use of the Procedure
The inverted L osteotomy may be the operation of choice for large advancements (greater than 12 mm) with counterclockwise rotation or for large setbacks (greater than 10 mm). It is also a good choice for reoperations resulting from altered ramal morphology and in patients with masseter hypertrophy with dense underlying cortical bone.
Extraoral Approach
The extraoral inverted L osteotomy (and its near cousin, the arching C osteotomy) can be used for advancements or setbacks. However, today it generally is used for complicated large advancements either because an alternative intraoral procedure is not feasible or because the mandibular anatomy is unusual (e.g., a thin ramus or a severely deficient mandibular posterior body height). Frequently a gap is created between the segments, requiring an autogenous or allogenic graft to fill the void created by the amount of movement. Selective cases of significant mandibular asymmetries may be managed better with an extraoral vertical ramus or inverted L osteotomy than an intraoral osteotomy.
Intraoral Approach
The major advantage of the intraoral approach over the extraoral approach is avoidance of a skin incision; this eliminates facial scarring and greatly reduces the risk of injury to the marginal mandibular branch of the facial nerve. The intraoral inverted L osteotomy involves a number of considerations. These include whether to perform both medial and lateral dissection, deciding how much of a bevel to use between the medical and lateral sides, and choosing the best types of rigid fixation to fix the segments. The intraoral inverted L osteotomy can be used for small mandibular setbacks and for large setbacks in selected cases. As with the extraoral osteotomy, it can be used for mandibular asymmetries and advancements. Several authors have advocated its use for either advancements or setbacks when the risk of damage to the inferior alveolar nerve is a particular concern. It may be equally advantageous for cases in which the preoperative computed tomogram shows a thin ramus.
Limitations and Contraindications
There are only a few limitations and contraindications to the use of an inverted L osteotomy. The extraoral approach includes a skin incision, which may result in an unsightly scar and possible damage to the facial nerve. Injury to the inferior alveolar nerve is much less likely with a vertical ramus procedure than with a bilateral sagittal split osteotomy (BSSO), but it is not eliminated. Kobayashi et al compared neurosensory disturbances in patients undergoing either an inverted L osteotomy or a BSSO. They concluded that the long-term prognosis for resolution of postsurgical neurosensory disturbances was better for the patients who underwent the inverted L osteotomy. They also noted that the width of movement between the segments influenced postsurgical neurosensory disturbances immediately after the inverted L osteotomy but that the relationship diminished with time.
Additional limitations and contraindications may apply for mandibular advancements without bone grafting. This technique may be less stable and may result in nonunion if the bone gap is too large.
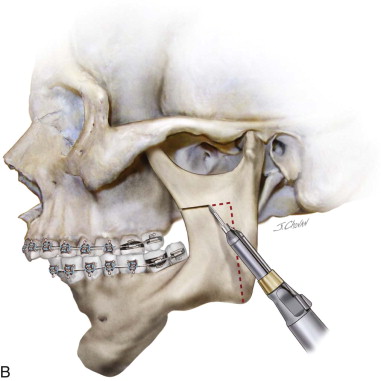
Technique: Extraoral Inverted L Osteotomy
Step 1:
Soft Tissue Incision and Dissection
A standard submandibular incision or Risdon approach is used to gain access to the lateral ramus of the mandible. Once the skin and subcutaneous tissues have been incised, a nerve stimulator is used to prevent injury to the marginal mandibular branch of the facial nerve. The masseter muscle is incised and retracted, and the sigmoid notch, anterior ramus, and posterior border of the mandible are identified ( Figure 32-1, A ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses