Introduction
The purpose of this retrospective study was to compare the long-term stability of maxillary incisor alignment in patients treated with and without rapid maxillary expansion (RME).
Methods
The sample comprised 48 subjects with Class I and Class II malocclusions, treated without extractions with fixed edgewise appliances, divided into 2 groups according to the treatment protocol: group 1 comprised 25 patients (15 girls, 10 boys) at a mean initial age of 13.53 years (SD, 1.63), who had RME during orthodontic treatment. Group 2 comprised 23 patients (13 girls, 10 boys) at a mean initial age of 13.36 years (SD, 1.81 years), treated with fixed appliances without RME. Maxillary dental cast measurements were obtained at the pretreatment, posttreatment, and long-term posttreatment stages. Variables assessed were the irregularity index and maxillary arch dimensions. Intergroup comparisons were made with independent t tests.
Results
Greater transverse increases were found during treatment in the group treated with RME. However, during the long-term posttreatment period, no significant difference was observed in the amount of incisor crowding relapse between the groups.
Conclusions
RME did not influence long-term maxillary anterior alignment stability.
There are indications that the amount of maxillary incisor irregularity in the long term out of retention is less than before treatment, and that rotational relapse of individual teeth rarely exceeds 20°. Some studies have concluded that rotational relapse is proportional to orthodontic correction, and that there might be an association between crowding and postretention reductions in arch length and width.
Rapid maxillary expansion (RME) with fixed expansion appliances is primarily used to correct maxillary transverse discrepancies, but other applications include increasing arch perimeter to relieve moderate tooth size-arch length discrepancies and facilitate nonextraction edgewise treatment in borderline patients. Expansion through maxillary suture widening with RME has been claimed to promote dimensional stability after retention. This stability was attributed to the skeletal component of arch enlargement from the expansion appliance rather than to dental expansion after edgewise appliance mechanotherapy. However, no previous study has investigated whether long-term maxillary incisor alignment and dimensional arch stabilities are greater in nonextraction patients treated with RME than in those treated without RME.
Studies on the immediate treatment effects of RME have reported increases in maxillary arch width after combined skeletal and dental expansion. Long-term changes in posttreatment maxillary arch dimensions are less well established, particularly in relation to the expected dimensional changes in untreated subjects with normal occlusion. Some long-term follow-ups have indicated a rebound effect of the dental component, yet there is relative dimensional stability of the skeletal aspect of expansion, resulting in maxillary arch dimension net gains. However, there are reports from complete stability to considerable relapse after maxillary arch expansion. Marshall et al found weak indirect evidence for long-term stability of maxillary expansion with either fixed or removable expansion appliances.
Despite favorable arguments about RME effectiveness in correcting maxillary transverse discrepancies and the common use of RME followed by fixed appliances as an option to relieve modest tooth size-arch length discrepancies, a possible influence of this procedure on long-term maxillary incisor alignment stability has not yet been investigated. The purpose of this study was to evaluate the influence of RME on maxillary incisor alignment stability by comparing dental arch measurements from nonextraction patients treated with edgewise appliances, with and without RME.
Material and methods
The sample, obtained from the files of the Department of Orthodontics of Bauru Dental School, University of São Paulo, Bauru, São Paulo, Brazil, included 144 dental casts of 48 patients treated without extractions. Dental casts were obtained at 3 times: pretreatment (T1), immediately after treatment (T2), and a mean of 5.2 years after treatment (T3).
In addition to the availability of dental casts, other inclusion criteria were the clinical records that described sex, ages at T1 and T2, length of treatment, length of retention, and long-term posttreatment time.
After active treatment, all patients wore a modified Hawley retainer in the maxillary arch, full time for the first 6 months and during sleep for the next 6 months. A lingual canine-to-canine mandibular bonded retainer was placed and left for a mean period of 3 years.
The sample was divided into 2 groups according to the treatment protocol (with or without RME).
Group 1 consisted of 75 dental casts of 25 patients (15 girls, 10 boys; initial mean age, 13.53 years; SD, 1.63 years) who had RME during orthodontic treatment. Sixteen patients had Class I molar relationships, 7 had quarter-cusp Class II molar relationships, and 2 had half-cusp Class II molar relationships. All had a combination of orthopedic-orthodontic treatment for a mean period of 2.07 years (SD, 0.55) and finished treatment at a mean age of 15.51 years (SD, 1.74). The mean T3 evaluation was 5.60 years (SD, 1.41).
The patients in this group were treated without extractions and had RME with the Haas or Hyrax appliance and subsequent fixed orthodontic appliances. The decision to use RME therapy was based on at least 1 preexisting criterion: maxillary crowding, posterior crossbite, or esthetics. All patients had some crowding, generally associated with narrow dental arches. Sixteen subjects exhibited posterior crossbites.
The patients underwent a standardized protocol of RME with 2 turns a day (0.25 mm per turn) until overcorrection of the transverse relationship. This overcorrection involved approximation of the palatal cusp tips of the maxillary posterior teeth and the buccal cusp tips of the mandibular posterior teeth in the transverse dimension.
The expander was kept on the teeth as a passive retainer for a mean period of 90 days. After expansion, the patients wore a simple palatal plate with bilateral posterior clasps for stabilization. The plate was worn full time for 6 months; in 9 patients, however, the plate was not used. Immediately after the expanders were removed, fixed edgewise appliances were placed.
Group 2 comprised 69 dental casts of 23 subjects (13 girls, 10 boys; initial mean age, 13.36 years; SD, 1.81 years) who had nonextraction orthodontic treatment without RME. They received full maxillary and mandibular fixed edgewise appliances. Ten patients had Class I, 8 had quarter-cusp Class II, and 5 had half Class II anteroposterior molar relationships. These patients underwent orthodontic treatment for a mean period of 2.18 years (SD, 0.93) and finished at a mean age of 15.54 years (SD, 1.86). The T3 study models were taken after a mean of 4.92 years (SD, 1.11).
T1, T2, and T3 maxillary dental casts were used. All dental cast measurements were made with a precision digital caliper (Mitutoyo America, Aurora, Ill). The assessed variables were Little’s irregularity index; intercanine, interpremolar, and intermolar widths; and arch length and perimeter ( Figs 1 and 2 ).
Maxillary dental casts were measured by 1 investigator (L.F.G.C.) to the nearest 0.01 mm, with the digital caliper. Measurements were made on the cusp tips of the canines and the mesial buccal cusps of the first molars of each patient. When there was a facet, the cusp tip was estimated. Measurements were blindly and randomly made for all patients. All were linear measurements, in millimeters, described as follows.
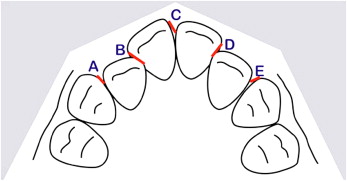
- 1.
Maxillary incisor irregularity: the sum of the 5 distances between the anatomic contacts from the mesial aspect of the right canine through the mesial aspect of the left canine; this is similar to Little’s method for evaluating mandibular incisor irregularity ( Fig 1 ).
- 2.
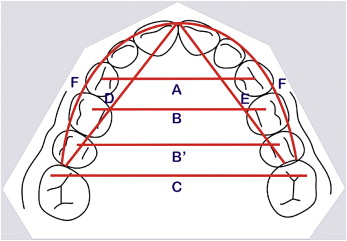
Intercanine width: the linear distance between the cusp tips of the maxillary canines ( Fig 2 ).
- 3.
Interfirst-premolar width: the linear distance between the central fossae of the maxillary first premolars ( Fig 2 ).
- 4.
Intersecond-premolar width: linear distance between the central fossae of the maxillary second premolars ( Fig 2 ).
- 5.
Intermolar width: the linear distance between the mesiobuccal cusps tips of the maxillary first molars ( Fig 2 ).
- 6.
Arch length: the linear distance along the midline from the interincisal midline to the mesial contact of the first molars ( Fig 2 ).
- 7.
Arch perimeter: the sum of the distances from the mesial contacts of the first molars to the distal contact points of the canines plus the mesiodistal widths of the canines plus the distance from the mesial contact point of the canines to the interproximal contact between the central incisors ( Fig 2 ).
Within 3 weeks from the first measurements, 15 dental casts were randomly selected and remeasured by the same examiner (L.F.G.C.). The casual error was calculated according to Dahlberg’s formula (Se 2 = Σd 2 /2n), where Se is the error variance and d is the difference between 2 determinations of the same variable. The systematic error was calculated with dependent t tests at P <0.05.
Statistical analysis
The intergroup compatibility evaluation regarding initial and final ages, treatment time, long-term posttreatment time, and pretreatment incisor irregularity were evaluated with t tests. The sex distribution and the initial malocclusion severity compatibility between the 2 groups were assessed with chi-square tests.
Means and standard deviations were calculated for all variables at T1, T2, and T3 for the whole sample. Treatment changes were also evaluated and calculated by subtracting the initial from the final values (T2 – T1). The amount of relapse was calculated by subtracting the final from the long-term posttreatment values (T3 – T2). The total changes were calculated by subtracting the initial from the long-term posttreatment values (T3 – T1). The intergroup comparisons at the several stages and observation periods were made with t tests.
The percentage of relapse was calculated as the rate between the relapse and the correction amounts.
The results were considered significant at P <0.05. All statistical analyses were performed with Statistica software (release 6.0, Statistica for Windows, Statsoft, Tulsa, Okla).
Results
The casual errors ranged from 0.08 (intersecond-premolar width) to 0.57 mm (Little irregularity). Paired t tests showed no statistically significant systematic errors.
The groups were similar regarding ages at T1 and T2, treatment times, long-term posttreatment times, initial maxillary incisor irregularity, sex, and initial malocclusion severity distributions ( Tables I to III ).
| Group 1 (with RME) n = 25 |
Group 2 (without RME) n = 23 |
||||
|---|---|---|---|---|---|
| Variable | Mean | SD | Mean | SD | P |
| T1 age (y) | 13.53 | 1.63 | 13.36 | 1.81 | 0.729 |
| T2 age (y) | 15.51 | 1.74 | 15.54 | 1.86 | 0.956 |
| Treatment time (y) | 2.07 | 0.55 | 2.18 | 0.93 | 0.625 |
| Long-term posttreatment time (y) | 5.60 | 1.41 | 4.92 | 1.11 | 0.072 |
| Initial irregularity (mm) | 7.65 | 2.96 | 6.56 | 2.84 | 0.201 |
| Girls | Boys | Total | |
|---|---|---|---|
| Group 1 (with RME) | 15 | 10 | 25 |
| Group 2 (without RME) | 13 | 10 | 23 |
| Total | 28 | 20 | 48 |
| Severity | Group 1 (with RME) |
Group 2 (without RME) |
Total |
|---|---|---|---|
| Class I | 16 | 10 | 26 |
| 1/4 Class II | 7 | 8 | 15 |
| 1/2 Class II | 2 | 5 | 7 |
| Total | 25 | 23 | 48 |
Group 2 (without RME) had greater first and second interpremolar widths at T1 ( Table IV ).
| Group 1 (with RME) n = 25 |
Group 2 (without RME) n = 23 |
||||
|---|---|---|---|---|---|
| Measurement (mm) |
Mean | SD | Mean | SD | P |
| T1 | |||||
| Little’s index | 7.65 | 2.96 | 6.56 | 2.84 | 0.201 |
| 3-3 width | 34.16 | 2.41 | 34.08 | 3.08 | 0.914 |
| 4-4 width | 33.26 | 2.12 | 34.71 | 1.86 | 0.015 ∗ |
| 5-5 width | 38.39 | 2.98 | 40.20 | 2.31 | 0.024 ∗ |
| 6-6 width | 49.46 | 4.15 | 51.13 | 2.62 | 0.106 |
| Arch length | 70.97 | 4.35 | 72.09 | 4.08 | 0.362 |
| Arch perimeter | 74.41 | 3.54 | 75.18 | 3.77 | 0.471 |
| T2 | |||||
| Little’s index | 1.42 | 1.05 | 1.60 | 0.73 | 0.497 |
| 3-3 width | 35.04 | 1.41 | 34.66 | 1.44 | 0.351 |
| 4-4 width | 36.90 | 1.64 | 36.34 | 1.81 | 0.260 |
| 5-5 width | 42.20 | 2.04 | 41.35 | 2.15 | 0.166 |
| 6-6 width | 52.43 | 2.55 | 51.52 | 2.50 | 0.219 |
| Arch length | 73.47 | 2.91 | 73.76 | 2.49 | 0.709 |
| Arch perimeter | 77.10 | 2.77 | 76.52 | 2.66 | 0.459 |
| T3 | |||||
| Little’s index | 2.93 | 1.97 | 3.12 | 1.42 | 0.713 |
| 3-3 width | 34.46 | 1.70 | 34.55 | 1.87 | 0.876 |
| 4-4 width | 35.76 | 1.82 | 35.76 | 1.81 | 0.990 |
| 5-5 width | 41.43 | 2.24 | 41.09 | 2.16 | 0.587 |
| 6-6 width | 52.24 | 2.92 | 51.94 | 2.51 | 0.709 |
| Arch length | 71.90 | 3.12 | 72.07 | 2.58 | 0.838 |
| Arch perimeter | 75.45 | 2.79 | 75.32 | 2.55 | 0.868 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


