Over the past 3 decades, successful application of dental endosseous implants has been well established in oral and maxillofacial surgery. Since the late 1980s to early 1990s, the use of endosseous implants has expanded to the treatment of orthodontic patients. The principle of placing implants as anchorage devices to facilitate orthodontic movement of teeth, as well as to affect skeletal growth, has broadened the clinical applications of dental implants. Conventional orthodontics for the treatment of dental and facial skeletal discrepancies often involves cumbersome intraoral appliances, such as full arch braces, interarch elastics, and Nance appliances, in addition to extraoral appliances such as headgear. In situations in which patients are partially edentulous or have oligodontia, the lack of teeth can often pose challenges for the orthodontist in devising a treatment plan with the existing dentition to provide sufficient anchorage. Implants placed into the maxillo-mandibular skeleton enable the orthodontist to provide additional anchorage and exert predictable force in all three spatial planes: transverse, vertical, and sagittal. There is a vast amount of literature on the use of implants in orthodontics to treat malaligned teeth by uprighting, extrusion, intrusion, mesialization, and distalization.
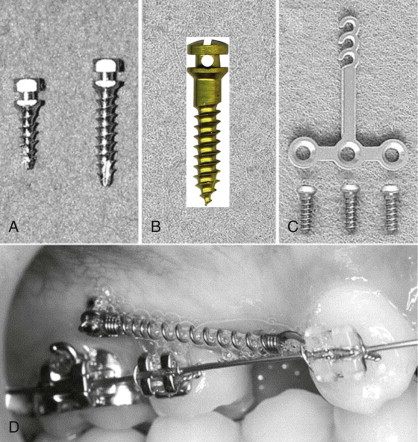
Early after their introduction, the literature has been filled with descriptions of different types and designs of anchorage devices for orthodontic purposes that have various shapes and sizes of screws, plates, cylinders, and other components. Some of these implants required a healing period for osseointegration before orthodontic forces could be applied, whereas others were designed to be left and restored with a prosthetic crown on completion of the orthodontic treatment. Several different classifications of osseous anchorage devices have been described by Creekmore and Eklund, Kanomi and Costa, and Cope. Devices with different designs that served the same purpose of assisting in orthodontic treatment lacked uniformity and thus made the nomenclature extremely confusing. In 2005, a meta-analysis conducted by attempted to clarify and further classify these implant devices according to their shape and size (cylindrical, screws, miniplates, and disk shaped), fixation of the implant to the surface of the bone (osseointegrated versus mechanical locking), and clinical applications (orthodontic, orthodontic and restorative/prosthetic, and orthopedic). In a more contemporary approach, the definition of these implants has been narrowed so that it refers specifically to titanium alloy miniscrews or miniplates that are placed as removable temporary anchorage devices (TADs) in the maxilla and mandible to facilitate orthodontic movement. For the purpose of this chapter, we will discuss the type of implants placed solely for the purpose of temporary orthodontic anchorage.
Unlike its predecessor, the conventional endosseous osseointegrated implant, a TAD differs from it in many ways. A TAD is designed to be placed for orthodontic anchorage purposes, and on completion of treatment the implant device is always removed. In addition, the success criteria for TADs are defined differently. The capacity to withstand orthodontic forces throughout treatment, lack of clinically detectable mobility, presence of soft tissue health, and lack of painful symptoms are defined as success. In other words, these anchorage devices do not need to be osseointegrated.
One of the early implant devices on the market for orthodontic anchorage was the palatal implant. In 1995, Block and Hoffman designed a disk-shaped subperiosteal implant with a roughened hydroxyapatite undersurface that could be placed in the hard palate for orthodontic anchorage. This implant required surgical placement through a palatal tunneling technique and a latency period for osseointegration before loading. Although studies documented its success in providing anchorage, this implant did not gain broad application because of multiple disadvantages, including cost, lengthy osseointegration period, and need for a surgical procedure to place and remove the implant. Similarly, devised a cylindrical palatal implant in 1996 for the same purpose. Without doubt, these devices have achieved success and safety in providing anchorage for the placement of implants in the palatal area.
Anatomic Considerations
Since 2006, the U.S. Food and Drug Administration has approved the use of TADs in patients who are 12 years and older. Pretreatment planning for these patients includes serial lateral cephalograms or hand-wrist films to assess growth cessation. Placement of anchorage implants in the mid-palatal suture may affect skeletal growth of the maxilla. Recently, cone beam computed tomography (CT) technology has drastically reduced the cost and increased the accessibility and ease of obtaining a three-dimensional volumetric study of areas where bone volume, quality, and proximity to vital structures may be questionable for the placement of palatal implants. CT analysis has revealed that bone density is thickest at the level between the first and second premolars and the first and second molars, thus making these areas ideal for placement. If a situation warrants placement of the anchorage more anteriorly, paramedian placement in the area of the premolars may be more suitable because this will avoid potential injury to the incisive neurovascular bundle. Generally, the incisive canal should be kept at a minimum distance of 1 cm from placement of the implant. Although classified as a temporary orthodontic anchorage device, the early generation of palatal implants required osseointegration and indeed differed from the more recent TAD miniscrews and miniplates.
TAD miniscrews are not osseointegrated. Instead, they rely on mechanical engagement of the screw threads to the cortical alveolar bone. Because of this very crucial difference, loading can be performed immediately at orthodontic forces of less than 2 N. An increase in length and hence surface area of TADs does not add to their stability since they do not engage by the principles of osseointegration. Any screw length greater than 5 to 6 mm and up to 12 mm appears to be sufficient. Unlike screw length, screw diameter is significant in determining the stability of TADs. Miyawaki and co-authors, in an article on the optimal screw dimensions and design of TAD miniscrews, reported that a diameter of no less than 1.2 to 1.4 mm in the maxilla and no greater than 1.4 to 1.8 mm in the mandible provides adequate stability. The recommended difference in screw diameter in the maxilla versus the mandible is due to differences in corticocancellous bone composition. The amount of cortical bone and its density are crucial factors in providing stability to TADs. The thickest portion of the alveolar bone is located between the lateral incisors and canines anteriorly and adjacent to the first molars posteriorly. These sites are ideal for the placement of TADs. Although placement of TADs is possible in areas where there is a high cancellous-to-cortical bone ratio, the hard palate, the infranasal spine, and the maxillary buttress, symphysis, parasymphysis, and retromolar region tend to be more optimal sites given their higher cortical bone content. The TAD miniplate carried over the traditional principles of plating for trauma and osteotomy fixation in oral and maxillofacial surgery. These plates are low profile with one end fixed to bone via screws while the other end emerges transmucosally and has tubes, buttons, notches, and grooves to allow orthodontic attachments ( Fig. 17-1 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses