(1)
Department of Endodontics, New York University College of Dentistry, New York, NY, USA
Abstract
The incidence of exacerbations (flare-ups) has been estimated to range from 2 to 20 %. This wide variation is due to differences in definitions of exacerbations and differences in research methodologies. This chapter describes causes of exacerbations and their treatment. Factors predisposing patients to exacerbation are reviewed. The presence of preoperative pain or mechanical allodynia (reduced mechanical pain threshold or percussion sensitivity) was found to be a positive predictor of postoperative pain in more than 15 studies.
Also noted as evidence-based predictors of postoperative pain are specific iatrogenic factors. Pulpectomy or as an alternative, pulpotomy are described as predictable means of treating endodontic emergencies. The significance and tracing of sinus tracts are also described.
The goal of an emergency visit is limited to making an accurate diagnosis and bringing the case under control symptomatically. Depending on clinical factors, incision and drainage is an important therapy in appropriate cases. Pulpectomy, pulpotomy, trephination, and occlusal reduction are reviewed as potential treatment modalities during an emergency visit.
Studies have determined that the most favorable response of periapical tissues occurred when both instrumentation and filling were short of the periapical constriction. This chapter also reviews the management of gross overfilling on the maxillary sinus and mandibular canal.
7.1 Introduction
Endodontic emergencies are a challenging part of clinical practice. The clinician must have an understanding of inflammatory and infectious processes, pain mechanisms, local anesthesia, the use of therapeutics, and patient management. This chapter will focus on emergencies occurring prior to, during, and after treatment.
As a broad generalization the necrotic tooth (non-vital) represents a microbiological host/parasite challenge, while the vital case represents a problem of managing an inflammatory process in a well-innervated vascular tissue. The unique environment of the pulp is another factor to consider. In both situations, when time permits, removal of the pulp is the initial goal. Swelling, in non-vital cases, may be localized or diffuse. Some swellings may extend through facial plains and be seen as a cellulitis. Each situation requires a somewhat different clinical and pharmacologic strategy based on biological considerations.
The etiology of a flare-up is multifactorial and dependent on interactions between the host’s immunological response, infection, and physical damage [5, 28, 36]. An exacerbation (flare-up) has been defined in a number of ways. Some definitions emphasize swelling as being a characteristic symptom while others emphasize the need for an emergency visit. The American Association of Endodontists Endodontic Glossary of Terms 2012 defines a flare-up as, “an acute exacerbation of an asymptomatic pulpal and or periradicular pathosis following the initiation or continuation of root canal treatment.”
There are a variety of techniques and therapeutic agents available to treat emergencies. Depending on the circumstances of the emergency, and what we have learned from the best available evidence, clinicians must select the appropriate treatment strategies on a case-by-case basis. Factors such as tooth vitality, the severity of pain and/or swelling, and medical history all have an effect on the strategy and selection of medications.
Prior to determining the course of treatment, the clinician should understand the pathogenesis of the problem. Regardless of when the exacerbation occurs, the goal of treatment is to relieve pain and swelling as quickly as possible.
7.2 Incidence of Flare-Ups
As noted earlier, the reported incidence of flare-up varies across studies and ranges from approximately 2 to 20 % of patients, with the higher prevalence generally reported in older studies using classic cleaning and shaping techniques [3, 33, 36]. With such a wide gap in findings, it is likely that differences in research methodologies have had a critical affect on their outcomes.
Investigators examined associations between flare-ups and specific pretreatment factors. Unfortunately, different methodologies and criteria have led to variations in reports of the incidence of flare-ups and significant pretreatment indicators. Using the current American Association of Endodontists (AAE) definition of flare-up, several studies found that a common predisposing clinical condition for the occurrence of a flare-up is a history of preoperative pain. Others noted that an asymptomatic pulp with a periapical lesion was an important factor [3, 5, 32, 33].
Patients with a flare-up usually describe severe pain, swelling, or pressure immediately after anesthesia has dissipated or 1–2 days following treatment. A consistently high incidence of flare-ups should serve as a signal for the clinician to evaluate basic clinical procedures such as accuracy of measurement control and instrumentation. Breakdowns in either of those procedures could account for high rates of exacerbation.
In a prospective clinical study, the level of pain experienced by patients varied from no pain or slight pain up to severe pain. Fifty-seven percent of patients reported no pain after debridement and shaping of the root canal system, although 21 % had slight pain, 15 % had moderate pain, and 7 % had severe pain. Relatively few patients experienced a flare-up or a postoperative problem requiring an unscheduled visit with unplanned treatment intervention to manage the patient’s symptoms [36].
7.2.1 Meta-analysis
Meta-analysis is a statistical procedure that integrates the results of several independent studies considered to be combinable. Pooled data from multiple studies increases the sample size and power, thus providing a more precise estimate of a treatment’s effect. The decision about whether or not results of individual studies are similar enough to be included in a meta-analysis is a critical issue.
7.2.2 Incidence of Flare-Up
A meta-analysis of the results of previous studies, concerning the incidence of endodontic flare-ups, reviewed all relevant articles published in dental journals in English from 1966 to May 2007. Only six studies met all inclusion criteria. Prospective case series and clinical trials were included in the meta-analysis [34]. The average percentage of incidence of flare-ups for 982 patients was found to be 8.4 %.
Differences in experimental design do not allow for a direct comparison of studies; however, the presence of preoperative pain or mechanical allodynia (defined as a reduced mechanical pain threshold or percussion sensitivity) was a positive predictor of postoperative pain in more than 15 studies involving more than 6,600 patients [6].
7.3 Predisposing Conditions
When symptomatic pretreatment patients have been included in the study cohort, predisposing conditions include periapical abscess, acute apical periodontitis [31, 32], preoperative pain [21], and swelling. Studies have found that the lowest incidence of flare-ups occurred in patients without periapical pathosis and when a sinus tract is present [32]. It is reasonable to hypothesize that a sinus tract allows drainage and prevents an increase in periapical tissue pressure.
Studies evaluated factors related to postoperative endodontic pain and flare-up. The presence of preoperative pain or mechanical allodynia (reduced mechanical pain threshold or percussion sensitivity) was a significant predictor of postoperative pain in more than 15 studies with a large number of patients [6].
Clinical Tips
-
Patients presenting with sensitivity to percussion should be considered at risk for postoperative pain.
-
Occlusal reduction in such cases when restorative factors permit can be considered a predictable pain-preventive strategy.
The etiology of a flare-up is multifactorial and dependent on interactions between the host’s immunological response, infection, and physical damage. The major causative factor has been described as microbial in origin [32].
There are additional factors that may also predispose a patient to pain. They include genetics, gender, and anxiety. These non-dental factors are being evaluated, and at this time it seems likely that in the future their significance will be more fully understood.
Although no single factor completely predicts the occurrence and severity of postoperative pain, an astute clinician should recognize that the presence of preoperative pain or mechanical allodynia (sensitivity to percussion) is a warning sign that postoperative pain is likely. That warning sign is an indication that pain-preventive steps should be taken. They include preemptive analgesics and occlusal reduction when there is evidence of mechanical allodynia.
7.3.1 Research
A retrospective study analyzed the records of 2,000 patients who had root canal therapy for necrotic teeth. One half of the patients had inter-appointment pain or swelling which required an emergency visit. The other half were patients who reported no complications after cleaning and shaping of their root canals. It was determined that some factors, such as age, sex, tooth type, presence of preoperative pain, presence of allergies, absence of periapical lesions, sinus tract stomas, retreated cases, as well as those receiving prescribed analgesics, had significant effects on the incidence of endodontic inter-appointment emergencies. In contrast, presence of systemic diseases, use of intra-canal medications, and penetration of the foramen with small instruments during length determination had no significant effect on the frequency of these emergencies [32]. The highest incidence of flare-ups was associated with mandibular teeth, retreatment procedures, females over the age of 40, and patients with a history of allergies [32].
7.4 Classic Narratives
At an emergency visit there are classic patient narratives that provide critical information.
Narrative 1
-
An example of a classic narrative concerns the patient who describes having had no pain until he/she bit down on something hard which resulted in an immediate sharp lancinating pain and left a tooth tender to even finger pressure. Those few words are a powerful clue as to causation and indicate the need for investigation into a possible vertical or other type of fracture.
Narrative 2
-
A patient may report having been awakened at night by pain but feels better as the next day progresses. However, the pain awakens the patient again during the following night but disappears after awakening. This description does not fit the most common profile of irreversible pulpitis. Usually, pulpal pain does not improve as the day goes on.
-
This patient would require a differential diagnosis for bruxism, sinusitis, TMD, as well as pain of endodontic origin. Sensibility tests and percussion tests would be important part of the diagnostic process. Normal responses to those tests would prompt the clinician to investigate a non-odontogenic cause of pain (Figs. 7.1 and 7.2).
 Fig. 7.1At the emergency visit the initial radiograph indicated that the cause of the patient’s pain originated from the mandibular right first molar. However, an additional radiograph including teeth anterior to the molar demonstrated a complicating factor (Courtesy of Dr. Joshua Most)
Fig. 7.1At the emergency visit the initial radiograph indicated that the cause of the patient’s pain originated from the mandibular right first molar. However, an additional radiograph including teeth anterior to the molar demonstrated a complicating factor (Courtesy of Dr. Joshua Most)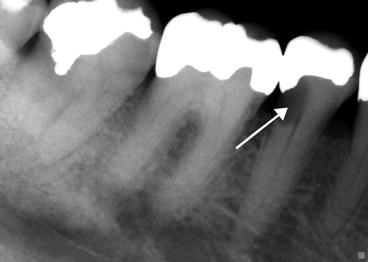 Fig. 7.2An additional radiograph indicated significant decay under the mandibular right second premolar. Arrow points to extensive decay. It was actually this tooth that was the cause of the patient’s pain (Courtesy of Dr. Joshua Most)
Fig. 7.2An additional radiograph indicated significant decay under the mandibular right second premolar. Arrow points to extensive decay. It was actually this tooth that was the cause of the patient’s pain (Courtesy of Dr. Joshua Most)
Clinical Tips
At the emergency visit:
-
Patients with a history of long-term low-level pain may pose a problem in achieving profound anesthesia.
-
It has been hypothesized that long-term inflammation can sensitize nociceptors resulting in a problem achieving profound anesthesia.
-
In these cases clinicians should be prepared to use supplemental anesthetic techniques.
7.5 Prognosis
At an emergency visit, when the need for endodontic treatment is established, the next consideration is the prognosis and treatment plan. Are there obstacles to satisfactory completion of proposed endodontic therapy? Has root canal therapy been done before? Are there restorative issues? Is there a periodontal component to the case?
Important factors include the following: systemic health of the patient, tooth anatomy, periodontal status, and the ultimate restoration. Is the proposed treatment appropriate for the patient? For example, a patient with poorly maintained dentition may not be a good candidate for root canal treatment, a post and crown.
Economic factors must also be considered. In some countries expenses are paid for by insurance but this is not universal. The goal must be to select the treatment that best serves the patient’s overall health needs (Figs 7.3, 7.4, and 7.5).




Fig. 7.3
Note difference in color between the central incisors

Fig. 7.4
The maxillary left central incisor has extensive diffuse calcification complicating endodontic treatment

Fig. 7.5
This radiograph taken during an attempt to achieve access indicates that the preparation is not in the canal space and is approaching perforation
7.6 Flare-Up and Outcome
The occurrence of an endodontic flare-up does not appear to influence the long-term prognosis of the tooth. It was reported that the occurrence of flare-ups had no significant influence on the outcome of endodontic treatment when reviewed 8–10 years later [31].
7.7 Causes of Exacerbations During Treatment
Iatrogenic factors associated with exacerbations include incomplete access, inaccurate measurement control, failure to maintain an accurate measurement, failure to completely remove all tissue from the canal, over-instrumentation, and failure to reduce occlusion when it is appropriate.
Clinical Tips
-
Establishment of an accurate measurement control is essential in avoiding over-instrumentation and postoperative pain.
-
Estimation of measurement increases the likelihood of postoperative pain.
-
Use of a rubber stop on instruments is helpful in maintaining measurement.
-
During irrigation the needle should not be wedged into the canal or placed close to the apical foramen.
-
Irrigate slowly to avoid pushing debris through the periapical foramen.
Non-vital cases differ from vital flare-ups in that even if all iatrogenic factors are addressed, a flare-up may still occur. Necrotic tissue is an ideal site for bacterial colonization and non-vital teeth should be considered to have infected pulps. Pathologic reactions in non-vital cases occur in the periapical tissues due to the extrusion of bacteria and their toxins.
The introduction of oxygen into the canal system upon opening the tooth can upset what may have been a balance between host defensive mechanisms and pathogens. Some anaerobic bacteria may die on exposure to aerobic conditions while other aerobic microbes may proliferate. This may change a chronic asymptomatic case into an acutely painful situation.
Clinical Tips
-
Deprived of vascular and neural supply, necrotic pulp tissue provides an excellent culture medium for bacteria.
-
Necrotic tissue has neither vascular nor neural supply and is not the source pain during an exacerbation.
-
Pain originates from an inflammatory response in the periapical tissues of a tooth with a necrotic pulp.
Pericementitis (inflammation of the periodontal ligament) is a specific symptom often associated with over-instrumentation and/or failure to reduce occlusion when indicated. Pericementitis presents as pain on occlusion and in severe cases pain even on gentle finger pressure against the tooth. When restorative conditions permit, occlusal reduction has been shown to be an effective method of preventing pain due to pericementitis in vital teeth, with any or all of the following indicators: a history of pain, absence of a periapical lesion, and sensitivity to percussion.
In the necrotic case instrumenting significantly short (more than 1–2 mm) of the periapical foramen leaves infected tissue behind that is a focus of bacterial colonization. Instrumenting beyond the foramen results in pushing debris into periapical tissues and causes a marked inflammatory reaction that results in severe pain and swelling. It must be remembered that the painful reaction and/or swelling that occurs in the periapical tissues is caused by bacteria and debris from the canal space being pushed through the periapical foramen. Thus the focus of treatment is eliminating or reducing the bacterial flora in the canal.
7.8 Goal of the Emergency Visit
The goal of an emergency visit is limited to making an accurate diagnosis and bringing the case under control symptomatically. Definitions of what constitutes an endodontic emergency vary but severe pain/swelling is the hallmark of endodontic emergencies.
Traumatic injuries may also be the cause of an emergency visit, but they represent a subset of cases with different considerations than purely endodontic emergencies. It must be noted that some dental traumatic injuries have concomitant injuries to the head and neck that require referral to a physician for evaluation. When doubt exists concerning the need for medical referral, it is wise to favor the referral.
The reader should review textbooks focused on dental trauma for a complete discussion of the subject. A helpful online site providing an extensive source of information concerning trauma is http://www.dentaltraumaguide.org/.
7.9 Managing Emergencies Due to Odontogenic Pain
7.9.1 Emergency Pulpectomy
Definitive non-pharmacologic endodontic treatment includes instrumentation, irrigation, occlusal reduction, and incision for drainage procedures. Numerous studies indicate that definitive treatment alone provides predictable and substantial relief from odontogenic pain. An example of effective treatment is a pulpotomy for patients with irreversible pulpitis. Regardless of the coronal medicament used, it has been reported that a pulpotomy abolished pain in 88 % of patients evaluated 1 day after treatment [7].
When time permits, the most predictable clinical strategy for the treatment of pain of endodontic origin is pulpectomy. Pulpotomy is usually reserved for multi-rooted vital cases when there is insufficient time for a pulpectomy.
7.9.2 Classic Research: Effectiveness of Pulpotomies
Seventy-three teeth with acute irreversible pulpitis had emergency pulpotomies. After removal of the coronal portion of the pulp, sterile cotton pellet or zinc oxide-eugenol cement was placed against the remaining pulp tissue. The cotton pellet was either dry or moistened with camphorated phenol, Cresatin, eugenol, or isotonic saline. This established six different treatment groups following the pulpotomy. All teeth were sealed with zinc oxide-eugenol cement. By means of questionnaires, symptoms were recorded after the anesthetic effect was eliminated and also at 1, 7, and 30 days after treatment. A total of 70 patients (96 %) reported pain relief. Three patients did not experience relief and returned for pulpectomy.
After the first postoperative day, no pain was reported by any of the patients. The frequency of discomfort decreased from 11 % 1 day postoperatively to 1 % 30 days after the emergency treatment. There was no difference in recorded symptoms among the six treatment groups. Thus, removal of caries, pulpotomy, and sealing of the cavity apparently were reliable means to relieve pain. The use of the various dressings did not contribute to the relief of pain [7].
A common question:
-
When instrumenting, should I use 21 or 25 mm hand files instruments?As a general statement, use the instrument closest in length to the measurement. This facilitates maintaining measurement since the handle can serve as a measurement guide. If the measurement is 19, 20, or 21 mm (or shorter), use 21 mm instruments. If the measurement is 23, 24, or 25 mm, use 25 mm instruments. An exception, in some cases, proximity of the file’s handle to the occlusal surface, could interfere with electronic apex locators.
7.9.3 Diagnostic Questions and Exacerbations
There are specific questions that a clinician must consider in order to determine the cause of a patient’s postoperative pain/swelling and/or pericementitis. Answers to the following questions provide critical information for the clinician enabling him/her to determine the appropriate course of treatment.
-
Was the measurement control accurate?
-
Was it maintained during instrumentation?
-
Was the canal completely instrumented?
-
Was the occlusion appropriately reduced if the case fit the prerequisites?
-
If there is swelling, is it circumscribed or extensive and spreading through facial planes resulting in cellulitis?
-
Is the swelling fluctuant?
7.9.4 Cleaning/Shaping and Irrigation
Cleaning/shaping and irrigation (with sodium hypochlorite) are the basic means of reversing inflammatory and/or infectious processes in the root canal system. Whether or not the pulp is inflamed or infected, it is damaged pulp tissue that is the driving force of endodontic pathosis. As the inflammatory and infectious process progresses, the ultimate end point is devitalization (necrosis) of the pulp and periapical pathosis.
Clinical Tips
-
The pathologic process leading to periapical pathosis may occur with or without pain and can be a rapid or insidious process.
-
Radiographs give no indication of the patient’s symptoms or what is happening at a cellular level.
-
In vital cases the goal is to totally remove inflamed well-innervated tissue without causing additional pain. In non-vital cases the focus is on removing microbes and their products from the canal system.
7.9.5 Occlusal Reduction
A number of clinical studies have evaluated the pain-preventive value of occlusal reduction. It is difficult to compare their results of the trials due to different methodologies, inclusion and exclusion requirements, and specific purposes of the study.
A large clinical study investigated the following questions: “Are there specific clinical findings that indicate a need for occlusal reduction? Can a reliable clinical profile be developed of patients most likely to benefit from occlusal reduction?” [27].
The research hypothesized that there may be specific preoperative conditions that are statistically significant indicators for occlusal reduction following instrumentation. This approach varied from previous research that placed all endodontic cases together in a single group without accounting for the importance of clinical variables. The earlier studies also had a smaller sample size.
Among the conditions evaluated were the presence or absence of pulp vitality, preoperative pain, and percussion sensitivity; presence of a periapical radiolucency, a stoma, and swelling; and a history of bruxism. The purpose of the study was to evaluate specific clinical factors as indicators for occlusal reduction following endodontic instrumentation.
A statistically valid profile of patients most likely to benefit from occlusal reduction was developed. In that study of 117 patients [27], approximately twice as many patients (80 %) with a diagnosis of irreversible pulpitis, who underwent occlusal reduction, reported no posttreatment pain when compared to no occlusal reduction control subjects.
Research Findings
Occlusal reduction was found to result in the prevention of postoperative pain when any or all of the following indicators were present:
-
Sensitivity to percussion
-
Vital tooth
-
History of pain
-
Absence of a periapical radiographic lesion
Interestingly, even when all of those pain predictors were present, occlusal reduction resulted in the complete absence of postoperative pain. This remarkable result is likely due to relieving occlusal stress from the periodontal ligament [27].
Biology: Occlusal Reduction
-
A possible biological explanation for the effect of occlusal reduction came from a study that examined pulp and periodontal ligament samples taken from 28 healthy premolars to be extracted for orthodontic reasons. One half of the teeth had a resin block over their occlusal surfaces and patients chewed gum for 30 min. The remaining patients had no occlusal interference and also chewed gum for 30 min. They found that occlusal trauma, experimentally induced, markedly increased expression of substance P, a pro-inflammatory mediator, in the pulp and periodontal ligament [4].
-
That research finding represents a possible biological explanation for what happens to the periodontal ligament when a tooth is either high in occlusion or taken out of occlusion. Occlusal reduction represents an important pain-preventive strategy in the presence of specific indicators [4].
Recent Research
A recent prospective clinical examination investigated the probability of the incidence, intensity, duration, and triggering of post-endodontic pain. The study considered factors related to the patient (age, gender medical evaluation) and to the affected tooth’s location, number of canals, pulp vitality, preoperative pain, periapical radiolucency, previous emergency access, and presence of opposing occlusal contacts [2].
A total of 500 single-visit root canal treatments were performed on patients referred to an endodontist. Shaping of root canals was performed manually, and apical patency was maintained with a size 10 K file. A 5 % sodium hypochlorite (NaOCl) solution was used for irrigation. Canals were filled using gutta-percha and AH-Plus sealer with lateral compaction. Independent factors were recorded during treatment, and characteristics of post-endodontic pain (incidence, intensity, type, and duration) were later surveyed through questionnaires.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


