LUCIAN CHIRILĂ
Chapter XIII
DENTAL IMPLANTS PLACED IN THE ESTHETIC ZONE
The esthetic aspect of the treatment is growing in importance, in response to the increasing demands of patients receiving dental implants.
Placement of implants, especially in cases of partial edentation, requires functional tridimensional location identification, which ensures long-term implant survival, at the same time requiring the consolidation of the bone and gum structures, which ensures long-term esthetic results. Esthetics and functionality should go hand in hand in all dental and periodontal zones, not just in some.
From the classical point of view, the esthetic zone is the anterior maxilla, although most of the upper dentoperiodantal structures actually participate in overall facial harmony.
The prosthetic restorations in this area are a challenge for the oral rehabilitation team, especially because of the maximum involvement in the general physiognomic aspect of the patient.
The esthetic aspect requires a correlation of the hard tissue parameters and the soft tissue that need to be harmonized. Both dental and gingival esthetics interlace for a nice smile and a balanced, harmonious facial appearance. The clinician should be well practiced and also consider the gingival factors (morphology, texture, color, shape, and size).2,5
Implicitly, the bony support must be assessed for quantity and quality. The maxillary bone is both the infrastructure on which the gum develops and shapes, and the receiver of the dental implant.
13.2 Establishing the diagnosis and planning the therapeutic sequence
The therapeutic outcome in uni- or multidental upper anterior edentation is a challenge, especially when several teeth are missing. Preserving or reconstructing a gingival morphology that gives the illusion of natural teeth is hard, and very often small technical slips will ruin the esthetic outcome and lead to patient dissatisfaction.1,2
A good esthetic result of prosthetic reconstructions on implants placed in esthetic zones depends on a judicious preoperative diagnosis and adequate therapeutic planning.
Preoperative anamnesis is important both for the patient assessment and for his/her esthetic expectations. The patient should undergo an overall health assessment. Possible medical problems that could contraindicate surgical operations could be evidenced. The patient’s dental state and history of dental and periodontal conditions should be assessed, and an oral and cervicofacial examination should be performed.
The results of the imaging tests (dental radiographs, cone beam computer tomography [CBCT] scans) are analyzed and evaluated in the light of the clinical findings and esthetic expectations. Study models and oral and facial photos will be taken to complete the perioperative documentation. This comprehensive examination may establish a number of esthetic risk factors for the prosthetic restoration supported by dental implants.6,7,8
A number of general pathological states, parafunctions (eg, bruxism), smoking, or poor oral hygiene should also be taken into account as potential risk factors for the functional and esthetic outcome of implants in the esthetic zone.
The ideal placement of implants, and the optimal prosthetic result, requires the evaluation of the edentulous space in relation to the facial, dental and periodontal examination.3 The success of the bone integration involves achieving a balance between functional and esthetic factors, with an asymptomatic interface between bone and implant and permanently healthy peri-implant gingival tissues.9,10
13.3 Criteria of successful implants9
|
Absence of implant mobility. |
|
Radiograph examination does not evidence peri-implant radiotransparency. |
|
Vertical bone lysis is less than 0.2 mm/year after the first year of functional prosthesis. |
|
No signs of gum inflammation, bone infection, pain, neuropathy, or paresthesia. |
|
A success rate of 85% after 5 years and 80% after 10 years are the minimum accepted criteria. |
Another objective of implant treatment is to preserve the bony and gummy structures and fulfill the esthetic purpose in accordance with the patient’s objective and subjective demands.7
The predictability of the esthetic outcome in the anterior maxillary zone depends on a number of factors, among which the most important are the esthetic parameters referring to the smile line, dental position, status, and morphology of the crowns and roots of neighboring teeth, the gingival biotype, the level of gum recession in the edentation, the morphology of the bone support and its spatial position, and the implant position.3,5,11,21
13.3.1 The smile line
The shape of the upper lip and its relation to the dental and periodontal structures are extremely important in the assessment of dental esthetics. This relationship is the starting point for esthetic restorations in the anterior maxillary zone. At the same time, this aspect determines the therapeutic methods for the reconstruction of dentoperiodontal harmony.6
On average, a smile reveals about 75% to 100% of the anterior incisors’ height and adjacent gum. If the upper lip line is lower, less than 75% of the incisors’ height will show (Fig 13-1).12
Clearly, a high smile line calls for more attention to esthetics than one revealing less than 75% of the teeth. In a high upper lip line, the smile will uncover the tooth neck margins and the gum, and the gum-, tooth relation is an important esthetic factor in the maxillary anterior zone.
The line of the lower lip is an element of facial harmony, its relationship with the maxillary incisors allowing the assessment of the curvature and inclination of the incisal plane, the position of the incisal margin, and the vestibular inclination of the anterior teeth.
Fig 13-1 The position of the lower margin of the upper lip generally reveals the dental papillae and 75% to 100% of the anterior teeth. This pattern is considered the “average smile line”, present in about 70% of the population.
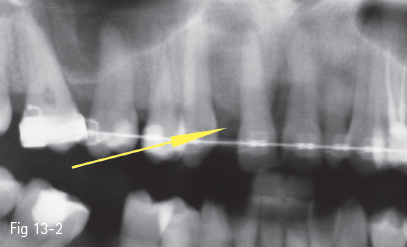
Fig 13-2 The insufficient mesiodistal space is corrected orthodontically, thus preventing the insertion of the implant too close to the interproximal bone in the risk area. The degree of orthodontic modification of this space depends on the size of the analogous tooth and the minimal mesiodistal space necessary to insert an implant (6 to 7 mm).
In the case of a relaxed smile, the incisal margin of the maxillary anterior teeth should follow the line of the lower lip. If the incisal margin is too anterior or posterior in relation to the internal margin of the red lip portion, there is a supposition of abnormality.12
The mucogingival line is also assessed, and a marked pattern is corrected by gingivectomy. The lateral incisor may be at a slightly different level from the central incisor, or have the same level. The patient should be informed of an exaggeration of the uneven level or asymmetries of the gum line. Even if not perceived, the existing gum line will be a reference for the esthetic restoration.
The anterior teeth provide the support for the upper lip. If there are many anterior teeth missing, patients may request a more labial position of the prosthetic reconstruction in order to have more labial support. Besides the fact that the general esthetic effect may be affected, the positioning of the teeth outside the neutral muscular balance zone will cause an abnormal stress on the implant, with repercussions for the bone and gums. The anterior teeth should be situated inside the “functional envelope” determined by the muscular balance between the lip and tongue. Repercussions are felt at the functional, esthetic, and phonetic levels, but also at the morphological level.
13.3.2 The position of the remaining teeth and roots, and the periodontal condition of the teeth that limit the edentulous zone
The remaining teeth should be assessed clinically and radiologically in order to establish their relation with the edentulous space. The position of the roots inclined toward the edentation limit the correct placement of the implant. Distancing the implant from the interproximal space in order to avoid contact with the neighboring root will place it outside the ideal site, and may limit the spontaneous recovery of the dental papillae by provisional crowns. These patients should undergo preoperative orthodontic treatment (Fig 13-2).
An important factor in the prediction of the therapeutic and esthetic outcome is the level of the interproximal bone. Teeth with marked lyses of the proximal bony septum represent an increased risk for the esthetic result, and even for the success of the implant. Local vertical augmentations of the interproximal bone are not too predictable due to the local conditions (avascular root or sepsis due to the impossibility of sealing the periodontal space). More predictable and recommended are augmentations of the soft tissues, by soft tissue grafts (Figs 13-3a and 13-3b).
Fig 13-3 a Good esthetic appearance 3 years after prosthetic restoration on implants at 12 and 22.
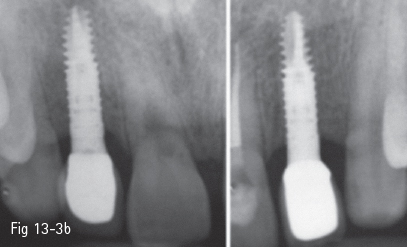
Fig 13-3 b Radiograph showing the preserved septum of the limiting teeth and support of the interdental papillae. The contact point is well placed for the stability of the papillae and the free gum margin.
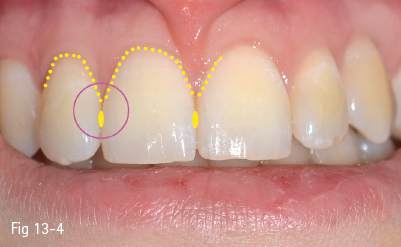
Fig 13-4 Normal shape of the gum line, level and shape of the interdental papillae, and dental contact point in healthy dentoperiodontal structures.
13.3.3 The shape of the gum line and the interdental papillae
The gum line may have a normal, marked, or flat shape, usually following the bone structure. In the case of a normal and healthy periodontium, the underlying bone is situated 2 mm below the cementoenamel junction (CEJ), and at 3.5 mm at the central incisor. Thus, in the case of a markedly high gum line, there will be more gingival tissue interproximally, and more coronary positioned, than in the vestibular tooth neck area. The flat gum line is easier to reproduce as it follows the bone level more closely.11
The interdental papilla is supported by the proximal bone at the level of the teeth, limiting the edentulous space. The height of both the interproximal bone and the edentulous spaces determines the esthetic outcome. The bone in the edentulous area should be at a physiological distance of 2 to 3 mm from the gingival margin (Fig 13-4).4,16,21
13.3.4 The periodontal biotype
This is one of the essential parameters determining the esthetic outcome of dental restorations in the maxillary anterior zone. The periodontal biotype determines the surgical approach and establishes the esthetic limitations. Two main periodontal biotypes are described: thin-scalloped and thick-flat.22
In the case of the thin-scalloped biotype, the periodontal architecture is pronounced and frail. It is characterized by bone fenestrations and minimal gingival attachments. Surgical operations often entail gum recession. Minimal surgical interventions are recommended, and the flaps created should not touch the blood supply in the implanted bone bed.6,11
In a case such as this, the patient should be informed regarding possible gum and bone recessions and the necessity of augmentation procedures. One way to prevent such periodontal reactions is to place the implant more palatally and the implant neck more apically.
In the case of a thick-flat, firm biotype, the periodontal tissue mass is fibrous and dense, with an increased amount of keratinized gum. The periodontal tissue bears trauma better, and gum recession is minimal. This periodontal type reacts to trauma by forming periodontal pockets (Figs 13-5a to 13-5c).6,11,13
Also, postoperative scars are more obvious, which might affect the final esthetic appearance. Nevertheless, long-term tissue stability is predictable, once the esthetic objectives have been achieved.
13.3.5 Bone morphology of the alveolar crest
The bony support is one of the defining factors of the success of implant therapy, as well as its long-term survival and esthetic outcome. The ideal tridimensional configuration of the alveolar ridge ensures a functional and stable placement of dental implants. At the same time, adequate bone morphology represents an infrastructure that helps preserve the soft tissues sufficiently to ensure esthetic success. Thus, besides the bone integration of the implants, there is also the premise of a well-located fibromucosa, which limits the prospect of gum recession.

Fig 13-5 a Coronary restoration on an implant (21). Firm periodontal biotype, with long-term tissue stability (9 years after prosthesis).

Fig 13-5 b Preserved tissue morphology, despite the fact that the neighboring teeth present signs of gum recession.

Fig 13-5 c Correct tridimensional positioning and observance of the biomechanical principles favored the long-term esthetic outcome.
If the bone anatomy and/or volume are inadequate, additional surgical procedures are necessary to restore the lost bone contour and volume. The patient must be informed and understand the therapeutic requirements for bone and soft tissue augmentation before the treatment so as to obtain the expected results (Figs 13-6a to 13-6d).
The bone architecture is analyzed tridimensionally, clinically, and by imaging. Current imaging techniques, such as cone beam scanning, have become accessible, and are very useful in tridimensional bone analysis. Clinical examination should not be dismissed as it plays a major role in establishing diagnosis and therapy.
As the bony substrate is a basis for gum volume and position, often bone augmentation also requires soft tissue augmentation. This aspect is particularly important in vertical bone defects, which are less predictable and more difficult to manage.
The loss of bone volume may also be assessed before extraction. Kois11,13 considers that the level of the anterior cervical bony ridge of the tooth in relation to the free gum margin is defining in the assessment of the bone deficit that will occur after extraction. The greater the distance, the greater the bone deficit will be after invasive procedures. Generally, the vertical distance between the free gum margin and the bone ridge is 3 mm, and a 1 mm bone resorption may be expected after the implant placement immediately after extraction. A distance larger than 3 mm may determine greater resorption. Thus, measurement before the operation may help the decision: a distance of more than 3 mm of the dentogingival complex requires orthodontic extrusion before the extraction.
Fig 13-6 a Lateral incisor 22 has grade II to III mobility, lyses of the vestibular cortical bone, and marked enlargement of the marginal periodontal space, determined by the longitudinal fracture of the root.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses





