Introduction
Light cure of resin-based adhesives is the mainstay of orthodontic bonding. In recent years, alternatives to conventional halogen lights offering reduced curing time and the potential for lower attachment failure rates have emerged. The relative merits of curing lights in current use, including halogen-based lamps, light-emitting diodes (LEDs), and plasma arc lights, have not been analyzed systematically. In this study, we reviewed randomized controlled trials and controlled clinical trials to assess the risks of attachment failure and bonding time in orthodontic patients in whom brackets were cured with halogen lights, LEDs, or plasma arc systems.
Methods
Multiple electronic database searches were undertaken, including MEDLINE, EMBASE, and the Cochrane Oral Health Group’s Trials Register, CENTRAL. Language restrictions were not applied. Unpublished literature was searched on ClinicalTrials.gov , the National Research Register, Pro-Quest Dissertation Abstracts, and Thesis database. Search terms included randomized controlled trial, controlled clinical trial, random allocation, double blind method, single blind method, orthodontics, LED, halogen, bond, and bracket. Authors of primary studies were contacted as required, and reference lists of the included studies were screened.
Results
Randomized controlled trials and clinical controlled trials directly comparing conventional halogen lights, LEDs, or plasma arc systems involving patients with full arch, fixed, or bonded orthodontic appliances (not banded) with follow-up periods of a minimum of 6 months were included. Using predefined forms, 2 authors undertook independent extraction of articles; disagreements were resolved by discussion. The assessment of the risk of bias of the randomized controlled trials was based on the Cochrane Risk of Bias tool. Ten studies met the inclusion criteria; 2 were excluded because of high risk of bias. In the comparison of bond failure risk with halogen lights and plasma arc lights, 1851 brackets were included in both groups. Little statistical heterogeneity was observed in this analysis (I 2 = 4.8%; P = 0.379). There was no statistical difference in bond failure risk between the groups (OR, 0.92; 95% CI, 0.68-1.23; prediction intervals, 0.54, 1.56). Similarly, no statistical difference in bond failure risk was observed in the meta-analysis comparing halogen lights and LEDs (OR, 0.96; 95% CI, 0.64-1.44; prediction intervals, 0.07, 13.32). The pooled estimates from both comparisons were OR, 0.93; 95% CI, 0.74-1.17; and prediction intervals, 0.69, 1.17.
Conclusions
There is no evidence to support the use of 1 light cure type over another based on risk of attachment failure.
The advent of dental bonding procedures has streamlined the placement of orthodontic appliances to a significant extent, with appliances becoming more discreet, easier to maintain, and less arduous to place. Bonding necessitates the use of orthodontic adhesives, which set by either chemical or light curing. Light cure systems are easy to use and versatile, with extended working time where necessary. Consequently, light cure allows sufficient time for careful bracket placement, removal of excess material, and consistent handling properties, and, by virtue of command set, permits seamless engagement of archwires.
Conventional blue halogen curing lights have been the mainstay of light cure systems for decades. However, these systems are inefficient; a small fraction (as little as 1%) of the total energy released is converted into light with an intensity of approximately 300 to 400 mW; the remainder is released as heat energy, which might be harmful to dental tissues. Inefficiency also stems from the initial production of white light with energy across the entire electromagnetic spectrum, which is later filtered to deliver useful blue light. In addition, these light curing systems are prone to output degradation. Furthermore, curing times of 20 to 40 seconds per tooth are recommended by manufacturers to permit adequate setting. Shorter curing times would save time for clinicians and patients and might also be associated with less likelihood of attachment failures by reducing moisture contamination.
In recent years, alternatives to halogen lights, including light emitting diodes (LEDs) and plasma lights, have been developed. LEDs incorporate 2 connected solid semiconductors, with an electric charge supplied from a battery. Energy is released almost exclusively as light energy, generating minimal heat. LEDs have longevity superior to that of halogen systems, little attenuation in intensity over time, and high emission intensity of up to 1600 mW. Plasma arc lamps, initially introduced in restorative dentistry, are a further option. They incorporate a xenon gas source ionized by 2 electrodes with a large voltage potential to produce plasma. Plasma arc lamps have a high peak energy level of up to 2000 mW and a narrower emission spectrum of 450 to 500 nm, making them more efficient and less susceptible to degradation than halogen lights. Consequently, these systems result in shorter curing times of 6 seconds for stainless steel brackets and 3 seconds for ceramic brackets. Plasma arc lamps, however, have a higher purchase cost, although this disadvantage is counterbalanced by an increased lifespan of 5000 hours compared with 40 to 100 hours for halogen lamps.
The limitations of halogen lamps are accepted and understood, and the relative merits of differing light curing systems have been compared in prospective research; however, these studies have not been evaluated systematically. It is hoped that by doing so, clinicians’ choice of curing lights will be informed by a robust evidence base. The aims of this study were therefore to compare bracket failure risks and times taken to place attachments with 3 light curing systems (halogen, LED, and plasma) during bonding of orthodontic brackets.
Material and methods
The protocol for a systematic review concerning light curing systems was registered on the National Institute of Health Research Database ( www.crd.york.ac.uk/prospero , Protocol: CRD42012002286). The following selection criteria were applied:
- 1.
Study design: randomized and controlled clinical trials, with split-mouth designs included.
- 2.
Participants: patients with complete arch, fixed, or bonded orthodontic appliances.
- 3.
Interventions: all attachments in the intervention group were cured with either an LED or a plasma arc light. Teeth in the control group had brackets that were set by using conventional halogen lamps.
- 4.
Exclusion criteria: studies with banded attachments and those involving follow-up periods less than 6 months were omitted from the review.
- 5.
Outcome measures: the initial bond failure was the main outcome measure with both light curing systems. The time required to place each attachment was a secondary outcome measure. When available, the time taken for failures to occur was also considered.
Comprehensive electronic database searches were undertaken without language restriction as follows: MEDLINE (1966 to April 2012), EMBASE (1980 to April 2012), Cochrane Oral Health Group’s Trials Register (April 2012), and Cochrane Central Register of Controlled Trials (CENTRAL, Cochrane Library Issue 2, 2012). Unpublished literature was accessed electronically by using ClinicalTrials.gov ( www.clinicaltrials.gov ) and the National Research Register ( www.controlled-trials.com ) with the term “orthodontic.” In addition, Pro-Quest Dissertation Abstracts and Thesis database was searched ( www.lib.umi.com./dissertations ) with “orthodontic*”. Efforts were made to obtain conference proceedings and abstracts when possible. Authors were contacted to identify unpublished or ongoing clinical trials and to clarify methodology and data as necessary. Reference lists of included studies were also screened for additional relevant research.
All assessments including analysis of research for inclusion in the review, assessment of risk of bias, and extraction of data were performed independently and in duplicate by 2 investigators (P.S.F. and N.P.). The investigators were not blinded to the authors or the results of the research. Disagreements were resolved by discussion. Seven criteria were analyzed to grade the risk of bias inherent in the studies: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of assessors, incomplete outcome data, selective reporting of outcomes, and other potential sources of bias. An overall assessment of risk of bias (high, unclear, low) was made for each included trial by using the Cochrane Collaboration risk of bias tool. Studies with at least 1 criterion at high risk of bias were considered to be at high risk of bias overall and excluded from the meta-analysis.
A data extraction form was developed for recording study design, observation period, participants, interventions, outcomes, and outcome data of interest including risk of failure of attachments and time taken to place attachments. Clinical heterogeneity of included trials was gauged by assessing the participants and methodology of primary studies, particularly setting, materials used, timing of data collection, and measurement techniques. Statistical heterogeneity was assessed by inspecting a graphic display of the estimated treatment effects from the trials with emphasis on the overlap of 95% confidence intervals. The chi-square test was used to assess for heterogeneity, with a P value below 0.1 signifying significant heterogeneity. I 2 tests for homogeneity were undertaken to quantify the extent of heterogeneity before each meta-analysis. I 2 values above 50% would signify moderate to high heterogeneity, which might preclude meta-analysis. Weighted treatment effects by using the DerSimonian and Laird method were calculated, and the results for attachment failure expressed as odds ratios (OR). For time required to place attachments, mean differences with 95% confidence intervals were calculated for individual trials and combined by using a random-effects model; a random-effects model was considered more appropriate because of the variations in population groups and settings. If more than 10 studies were included in the meta-analysis, standard funnel plots and contoured enhanced funnel plots would be drawn to assess publication bias.
Sensitivity analyses were planned at the outset to address studies at higher risk of bias, publication bias, and other potential sources of heterogeneity, including overriding effects of large studies and differences in outcome related to specific combinations of curing lights and adhesives to clarify their influence on the overall outcome. Meta-analyses and sensitivity analyses were undertaken (version 12.1TM; StataCorp, College Station, Tex) using “metan” and “metareg” commands.
The quality of evidence was assessed by using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system with GRADE evidence profile tables produced. The GRADE system was used to assess the overall body of evidence, initially assuming a high level of evidence from randomized controlled trials but downgrading as appropriate based on the following domains: (1) study limitations (risk of bias), (2) inconsistency of results, (3) indirectness of evidence, (4) imprecision of results, and (5) publication bias. The quality of evidence can be classified as follows :
High: further research is unlikely to change our confidence in the estimate of effect.
Moderate: further research is likely to have an important impact on our confidence in the estimate of effect and might change the estimate.
Low: further research is likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low: any estimate of effect is uncertain.
Results
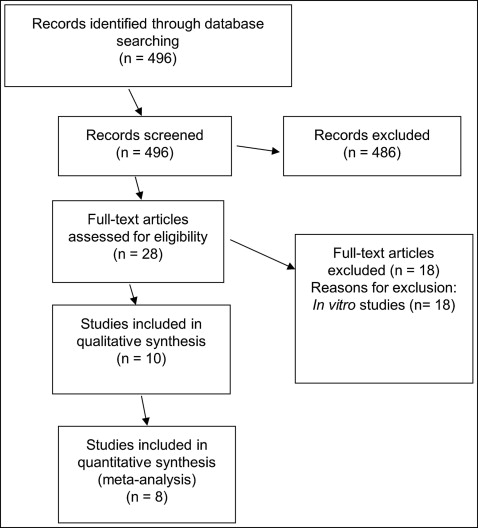
Twenty-eight trials were initially deemed potentially relevant to this review ( Fig 1 ). After we reviewed the abstracts, 10 trials satisfied the inclusion criteria. All 10 studies included in the qualitative analysis were prospective clinical trials with split-mouth designs ( Table I ). One study was described as a controlled clinical trial ; the rest were described as randomized controlled trials. A further study involved an alternate assignment; this approach was nonrandom, risking bias and preventing allocation concealment.
| Study | Methods | Observation period | Participants | Interventions | Outcomes |
|---|---|---|---|---|---|
| Manzo et al (2004) | Parallel group Split mouth RCT |
11 (±3.2) mo | 45 patients 28 female, 17 male Mean age, 14.8 y (range, 10-35 y) |
304 brackets bonded with plasma arc PACL Apollo 95E for 6 sec 304 bonded with conventional halogen HCL Ortholux XL 3000 for 20 sec Transbond XT |
Bond failure risk Time to event Bonding time |
| Sfondrini et al (2004) | Parallel group Split mouth RCT |
12 months | 83 patients 48 female, 35 male Mean age, 17.3 ± 4.5 y |
717 brackets bonded with plasma arc (PAC System) for 5 seconds 717 bonded with conventional halogen (Ortholux XT) for 20 sec Transbond XT |
Bond failure risk Time to event Indirectly bonding time |
| Cacciafesta et al (2004) | Parallel group Split-mouth RCT |
12 months | 30 patients 18 female, 12 male Mean age, 16.7 ± 3.2 y |
300 brackets bonded with plasma arc (PAC system) for 5 sec 300 bonded with conventional halogen (Ortholux XT) for 20 sec APC (Transbond XT) |
Bond failure risk Time to event Indirectly bonding time |
| Pettemerides et al (2004) | Split mouth 2 × 2 factorial |
6 mo | 20 patients Sex and age unspecified |
176 brackets bonded with plasma arc (Apollo 5E) for 3 sec 176 bonded with Ortholux XT for 20 sec Transbond XT (176 brackets per light) Fuji Ortho LC (176 brackets per light) |
Bond failure risk |
| Signorelli et al (2006) | Parallel group Split mouth RCT |
13 months (386 days) |
25 patients 14 female, 11 male |
222 brackets bonded with plasma arc (3M Ortholite) for 6 sec 223 conventional halogen (Ortholux XT) for 20 sec APC (Transbond XT) |
Bond failure risk Time to event Indirectly bonding time |
| Pandis et al (2007) | Parallel group Split mouth CCT |
15 mo (range,13-18 mo) |
25 patients 15 female, 10 male Mean age, 15 y (range, 12-16 y) |
247 brackets bonded with plasma arc (3M ortholite) for 9 sec 247 bonded with LED (Satelec mini LED) light for 9 sec Orthosolo-Enlight |
Bond failure risk Indirectly bonding time |
| Krishnaswamy and Sunitha (2007) | Parallel group Split mouth RCT |
15 mo | 30 patients Age range, 15-20 y |
271 brackets bonded with LED (LED Max 4) for 10 sec 273 bonded with halogen (Astralis 3) for 20 sec Transbond XT |
Bond failure Time to event Bonding time |
| Mirabella et al (2008) | Parallel group Split mouth RCT |
8.9 mo | 65 patients 34 female, 31 male Mean age, 16.2 ± 3.4 y |
575 brackets bonded with LED (Ortholux LED) for 10 sec 577 bonded with halogen light (Ortholux XT) for 20 sec APC (Transbond XT) |
Bond failure Time to event Bonding time |
| Russell et al (2008) | Split mouth RCT | Full course of treatment | 43 patients 29 female, 14 male Ages, 11-28 y 4 lost to follow-up |
354 brackets bonded with plasma arc (Ortho Lite) for 6 sec 354 bonded with halogen light (Visilux 2) for 20 sec APC (Transbond XT) |
Bond failure Bonding time Rebond time Sensitivity or discomfort |
| Koupis et al (2008) | Splitmouth RCT | 9 mo | 30 patients 19 female, 11 male |
300 brackets bonded with Ortholux LED for 10 sec 300 bonded with conventional halogen light (Ortholux XT) for 20 sec Transbond XT |
Bond failure risk Time to event Indirectly bonding time |
After the assessment of risk of bias ( Table II ), 8 of the 10 studies were included in the quantitative synthesis. Five involved comparison of plasma arc and halogen lights ; the remaining 3 focused on LEDs and conventional light curing systems. The durations of the studies ranged from 6 months in 1 study to 15 months and extended over the complete course of treatment in 1 trial. The brackets analyzed were precoated in 3 excluded studies, with Transbond XT used in all included studies.
| Study | Random sequence generation | Allocation concealment | Blinding participants and personnel | Blinding assessor | Free from incomplete outcome data | Free from selective reporting | Free from other sources of bias |
|---|---|---|---|---|---|---|---|
| Manzo et al (2004) | Unclear | Unclear | Low | Low | Low No losses described |
Low | Low |
| Sfondrini et al (2004) | Low: random table | Unclear | Low | Low | Low No losses described |
Low | Low |
| Cacciafesta et al (2004) | Low: random table | Unclear | Low: patients blind | Low | Low No losses described |
Low | Low |
| Pettemerides et al (2004) | Low: random table | Unclear | Low | Low | Low No losses described |
Low | Low |
| Signorelli et al (2006) | High: alternate | Unclear | Low | Low | Low No losses described |
Low | Low |
| Pandis et al (2007) | High | High: not done | Low | Low | Low No losses described |
Low | Low |
| Krishnaswamy and Sunitha (2007) | Unclear | Unclear | Low | Low | Low No losses described |
Low | Low |
| Mirabella et al (2008) | Unclear | Unclear | Low | Low | Low No losses described |
Low | Low |
| Russell et al (2008) | Low: computer | Low: sequentially numbered opaque sealed envelopes | Low | Low | Low 4 losses to follow-up |
Low | Low |
| Koupis et al (2008) | Unclear | Unclear | Low | Low | Low for failures No losses described |
Low | Low |
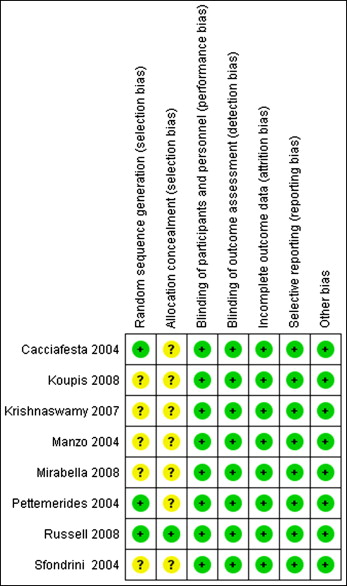
Risk of bias assessment was carried out in accordance with the Cochrane risk of bias tool ( Table II , Fig 2 ). One study did not involve random allocation ; another study involved a determinate allocation system with alternation between patients. Both of these studies were therefore considered to be at high risk of bias and omitted from the statistical analyses. The method used to generate the unpredictable sequence was clear in 4 studies, which used random number tables or computer systems ; these studies were therefore regarded as having a low risk of bias for this criterion. However, of these studies, only 1 referred to subsequent allocation concealment. Unsuccessful attempts were made to clarify the randomization procedure, concealment of allocation, and the potential for measurement bias by contacting authors, as appropriate. However, risk of bias for allocation concealment was regarded as “unclear” in most studies because it could not subsequently be elucidated. Data reporting appeared to be complete in all studies, with losses to follow-up explained. Further threats to bias were not identified. Therefore, overall, 1 study was judged to be at low risk of bias, and 7 studies had unclear risks of bias. All 8 were therefore included in the quantitative synthesis.
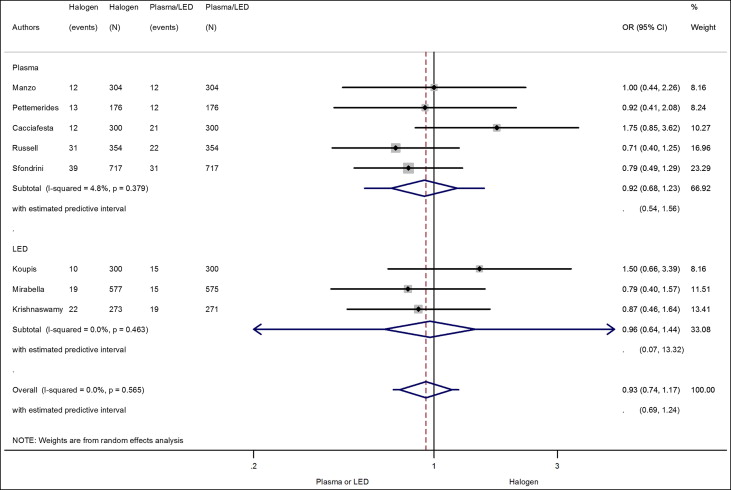
Five studies encompassing 3702 attachments were analyzed; 205 failures (5.54%) were recorded ( Tables III and IV , Fig 3 ). A slightly higher failure risk of 5.8% was found with the halogen light (107 failures) than with the plasma arc light (5.3%; 98 failures). A random-effects meta-analysis comparing failure risk with the 2 curing lights did not show a significant difference in the odds for failure with either curing light ( Fig 3 : OR, 0.92; 95% CI, 0.68-1.23). Little statistical heterogeneity was observed in the meta-analysis (I 2 = 4.8%; P = 0.379), confirming that statistical comparisons were appropriate. The prediction intervals indicated that the intervention effect in a future trial is likely to range from 0.54 to 1.56, confirming the lack of association between light cure system on bracket failures.
| Study | Intervention (number of attachments) | Bond failure numbers (%) | Time per tooth (sec) | ||
|---|---|---|---|---|---|
| Halogen | Plasma arc | Halogen | Plasma arc | ||
| Manzo et al (2004) | Plasma arc (304) Halogen (304) |
12 (3.9%) | 12 (3.9%) | 82 ± 32 | 65 ± 19 |
| Sfondrini et al (2004) | Plasma arc (717) Halogen (717) |
39 (5.4%) | 31 (4.3%) | ||
| Cacciafesta et al (2004) | Plasma arc (300) Halogen (300) |
12 (4%) | 21 (7%) | ||
| Pettemerides et al (2004) | Plasma arc (176) Halogen (176) |
13 (7.4%) 10 (11.4%) with Fuji Ortho LC; 3 (3.4%) with Transbond XT Overall 7.4% |
12 (6.8%) 9 (10.2%) with Fuji Ortho LC; 3 (3.4%) with Transbond XT Overall 6.8% |
||
| Russell et al (2008) | Plasma arc (354) Halogen (354) |
31 (9.5%; 95% CI, 6.8-13.1) | 22 (6.7%; 95% CI, 4.5-10) | 123 | 99 |
| Study | Intervention (number of attachments) | Bond failure numbers (%) | |
|---|---|---|---|
| Halogen | LED | ||
| Krishnaswamy and Sunitha (2007) | LED (271) Halogen (273) | 22 (8.06%) | 19 (7.01%) |
| Mirabella et al (2008) | LED (575) Halogen (577) | 19 (3.29%) | 15 (2.61%) |
| Koupis et al (2008) | LED (300) Halogen (300) | 10 (3.33%) | 15 (5%) |
Few data were forthcoming in relation to time to place attachments, with time differences per attachment alluded to in just 2 studies, precluding meaningful meta-analysis. However, the results from both studies were consistent in demonstrating a slight reduction in bonding time with the plasma arc light vs the halogen light; the difference was about 24 to 27 seconds per tooth. Bonding time differences can also be inferred, since halogen light curing required 20 seconds, plasma arc 5 to 6 seconds, and LED 9 to 10 seconds per bracket.
Three studies were included in this meta-analysis ( Table IV , Fig 3 ). Slightly fewer failures were reported in these 3 studies, with failure risks of 4.4% with halogen lamps and 4.3% with LEDs. The random-effects meta-analysis, however, indicated no significant difference between the systems regarding failure risk (OR, 0.96; 95% CI, 0.64-1.44). The prediction interval in this meta-analysis was extremely wide, since only 3 studies were included in this meta-analysis.
The degree of heterogeneity between studies in both analyses was found to be low (I 2 = 0%-4.8%). Sensitivity analysis in terms of subgroup and overall comparisons were undertaken, with little difference in estimates ( Fig 3 ). Additionally, meta-regression analysis was undertaken using the 2 types of light source (plasma arc or LED) and the number of months of follow-up as covariates. No covariate showed evidence of association with the risk of failure ( Table V ). However, only 1 study followed patients over the entire course of treatment. Statistical analysis of publication bias was also not indicated, because fewer than 10 studies were included in the quantitative synthesis. The assessment of the quality of the collected evidence, according to GRADE, regarding the effect of the light curing systems indicated that the level of evidence contributing to the conclusions was high ( Tables VI and VII ). This suggests that further research is unlikely to have an important impact on confidence in the effect estimates.



