D. Rodriguez, MD, DDS and Paul N. Manson, MD
10.1 Introduction
The face is vitally important for communication, nutrition, perception, and interpersonal relationships. Aesthetic attractiveness and facial expression influence personality and success. Appropriate management of craniofacial trauma is thus crucial to maintaining livelihood and identity. Every facial injury results in damage to soft tissue, with many involving injury to both soft tissue and bone. Craniofacial trauma may present as an isolated injury or may be a component of multiple injuries to several organ systems.1,2 Multidisciplinary cooperation between trauma surgeons, orthopedists, neurosurgeons, and plastic surgeons can facilitate a prompt reconstruction. Although there are a few true facial emergencies, the literature has historically underemphasized the advantages and superior aesthetic results of prompt, definitive anatomic reconstruction of facial bone and soft tissue injuries.3–8 This chapter provides an overview of the evaluation and treatment of the most common craniofacial injuries.
10.2 Evaluation and Initial Treatment
Once the initial trauma evaluation is complete and life-threatening trauma has been adequately addressed, management can focus on clinical examination, computed tomography (CT) imaging, and initial treatment.9–11
10.2.1 Physical examination
Most facial injuries are accurately assessed by thorough clinical inspection; thus, methodical examination of all facial structures is essential. Examination proceeds from top to bottom (or bottom to top), and lateral to medial in each of the following facial regions: forehead, orbits, nose, maxilla, and mandible. Palpation of all bony surfaces should note tenderness and deformity. Discoloration, pain, localized tenderness, numbness or paralysis, malocclusion, crepitus, “step-off” margins of facial bones, double vision, decreased visual acuity, facial asymmetry, gross deformity, facial contour changes, and eye malposition are all symptoms that suggest deeper structural trauma. The search for occult lacerations must include the eyelids, ear canal, mouth, floor of the mouth, pharynx, and nose.
Frontal or basilar skull fractures may lacerate the dura, leading to pneumocephalus or cerebrospinal fluid (CSF) leak. CSF may exit from the nose (rhinorrhea) or ear (otorrhea), implying a communication between the subdural space and the external environment and raising the possibility of meningitis. CSF rhinorrhea or otorrhea is often obscured by the presence of blood mixed with draining CSF, making the confirmation of a CSF leak difficult. A “double ring sign” may be visible when draining blood and CSF are absorbed using a paper towel. In the presence of displaced fractures, intracranial repair of the dura is indicated. Definitive operative treatment is accompanied by the administration of prophylactic antibiotics. Therefore, rhinor-rhea or otorrhea in the setting of craniofacial trauma should be evaluated thoroughly for the presence of CSF, and warrants detailed CT evaluation of the cranial base. Conversely, the presence of pneumocephalus on CT imaging raises high suspicion for a CSF leak.
The eye and visual function must be specifically evaluated. The symmetry of the pupil, speed of pupillary reaction, extraocular motion, and presence of hyphema are all noted. The presence of periorbital or subconjunctival ecchymoses implies the possibility of an orbital fracture or globe injury. In particular, one should palpate the superior and inferior orbital rims, zygomatic arches, and malar prominences. Visual acuity must be promptly evaluated, noting the presence of field defects, diplopia, or decreased light perception. Lacerations of the eyelid suggest the possibility of globe rupture, and the globe must be examined for integrity in these situations. Lacerations occurring in the medial third of the lower or upper eyelids suggest the possibility of lacrimal system injury, and the puncta and lacrimal duct should be thoroughly examined with a lacrimal probe when these lacerations are present.
Nasal examination is greatly facilitated by use of a nasal speculum. Pain and pressure sensation, including complete anesthesia or hypoesthesia, should be documented in the supraorbital, corneal, infraorbital, and mental nerve distributions. A neurologic facial examination must be completed and documented before administration of any local anesthesia or nerve blocks. Lacerations of major sensory or motor nerve branches and lacerations of the parotid duct should be managed in the operating room by direct repair with fine suture under magnification. Lacerations of the parotid duct are almost invariably accompanied by buccal facial nerve-branch laceration because the two structures travel next to one another.
An intraoral examination with direct palpation of the maxillary and mandibular dental arches and teeth is followed by an examination of the horizontal and vertical portions of the mandible. The movement of the jaw, its relation to the maxilla, and the occlusal relation of the maxillary and mandibular dental arches should be noted. If lucid and cooperative, the patient should be asked if the teeth meet together normally. The excursion of the mandible while palpating the temporomandibular joint (TMJ) should also be evaluated. The presence of step-off deformities in the dentition, bleeding, loose teeth, and intraoral lacerations suggest areas of deeper bony involvement.
10.2.2 Radiographic examination
All patients with significant facial injuries must have a CT of the face, cervical spine, and head.12,13 Thin-cut, multiplanar CT imaging is currently the gold standard for bony injury. Plain roentgenograms provide little value. Images should include the frontal bone, frontal sinus, orbital and nasal regions, midface, and mandible, including the TMJs. If there is tooth involvement in any fracture identified on CT, a panoramic (Panorex) image can be obtained to assess tooth and tooth-root injury. In most cases, CT evaluation supplements and confirms the findings of a thorough clinical examination.
10.2.3 Initial soft tissue and fracture management
Lacerations are thoroughly inspected and accessed for depth and direction. Any foreign bodies are identified, the level of wound contamination is assessed, and damage to deeper structures, such as muscles, nerves, and bone, is identified.
Cleansing of soft tissue lacerations is accompanied by sharp debridement of the immediate contused tissue edge if possible, and scrubbing or pressure irrigation of the involved tissue. Thorough tissue irrigation helps to decrease contamination and remove foreign material. Areas where debridement should be conservative or avoided include the vermilion border, lips, eyelids, eyebrow, nostril rims, and distal nose. Scar formation is minimized by irrigation and sharp debridement that achieves a minimally contaminated, flat wound surface. Antibiotic use is required when the wound cannot be made “clean” by surgical debridement or in the presence of high-level contamination, such as animal or human bites. Direct primary closure of facial wounds is generally preferred, although open management is considered in special circumstances.
Any localized facial hematoma should be drained by direct incision over the fullest point. A small suction tip can then be inserted to aspirate the hematoma, or the hematoma cavity can be evacuated with sequential manual pressure. After evacuation, the cavity should be irrigated to remove any remaining clot and assess for recurrent bleeding. A soft, lubricated compression dressing is then applied.
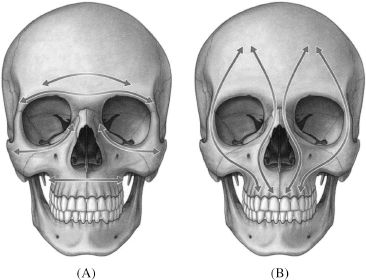
Figure 10.1. (A) Horizontal and (B) vertical facial buttresses. The facial buttresses are the support pillars of the face and overlying soft tissues. Buttresses adjacent to fracture sites serve as anchor points for fixation hardware. Disrupted buttresses must be reduced and reconstructed to achieve optimal results. Reprinted with permission from Elsevier (Guyuron B, Eriksson E, Persing JA. Plastic Surgery: Indications and Practice. Vol. 1. 2009:633). Copyright © 2009 Elsevier.
After complete physical examination, evaluation of CT imaging, and initial soft tissue injury management, grossly displaced tissues and fractures can be manually repositioned. Intermaxillary fixation (IMF) can be applied to the jaws to temporarily stabilize fractures involving occlusal segments. The management of facial fractures therefore first requires identification of fractures in each anatomic region as visualized on CT. The fracture pattern in each anatomic region is then classified, and management options for the regional fracture pattern weighed by anatomic region, complexity, and peripheral facial buttresses (Figure 10.1). Regions are then considered in combination to generate a logical, graded, operative treatment sequence.
10.3 Frontal and Supraorbital Fractures
The frontal sinus generally consists of two asymmetric cavities separated by a bony partition (Figure 10.2). Signs of frontal sinus fractures include nasal bleeding, external lacerations, or contusions in the forehead area.14 In cases with significant displacement, a depression may be visualized in the skin overlying the frontal bone, sinus, or orbital rim. A CSF leak or subcutaneous emphysema may be present. Posterior wall fractures imply the possibility of a dural laceration, especially when the depth of displacement exceeds the thickness of the posterior table. Displaced posterior wall fractures generally require intracranial surgical exploration and dural repair.
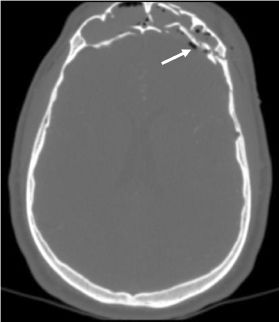
Figure 10.2. Comminuted frontal sinus fracture with compromise of the anterior and posterior walls. Associated pneumocephalus (white arrow).
Any fracture blocking the nasofrontal duct is treated by obliteration or cranialization of the sinus cavity to minimize the possibility of intracranial infection and mucocele development (Figure 10.3).15,16 In these procedures, the frontal sinus mucous lining is stripped in its entirety, and a bur is used to lightly abrade the sinus walls. This eliminates mucosal invaginations (foramina of Breschet) and prevents mucosal regrowth. In sinus obliteration, the nasal frontal ducts are plugged and the remainder of the sinus is obliterated with bone graft. This eventually converts the sinus into a portion of the bony skull. Alternatively, the sinus can be cranialized. After mucosal stripping and abrasion, the posterior wall of the frontal sinus is removed, and the brain and dura are allowed to rest on the remaining sinus floor and anterior wall (Figure 10.4). This effectively incorporates the sinus into the intracranial space.
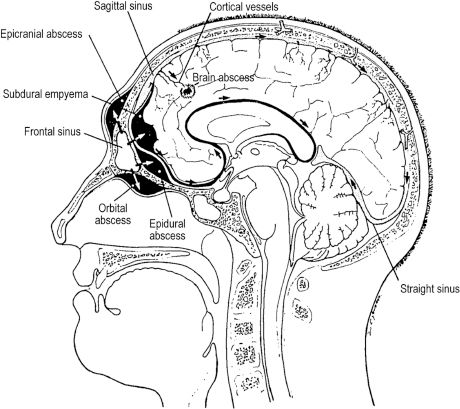
Figure 10.3. Sagittal section through the frontal sinus depicting potential routes for the spread of infection from the frontal sinus throughout the face and cranium. Reprinted with permission from John Wiley and Sons (Mohr RM, Nelson LR. Frontal sinus ablation for frontal osteomyelitis. Laryngoscope 1982;92:1006–1015). Copyright © 1982 John Wiley and Sons.
The supraorbital rim of the frontal bone constitutes a sturdy prominence protecting the eye socket. Lacerations and bruises commonly occur in this area with fractures, which usually produce easily palpable step-off deformities. Numbness may occur in the distribution of the supraorbital or supratrochlear nerves. Supraorbital fractures typically produce smaller, isolated bony segments that are depressed posteriorly and inferiorly. This results in an inferior and forward protrusion of the globe, lid ptosis, and possibly superior orbital fissure/orbital apex syndrome, or a superior gaze paresis that may mimic inferior rectus entrapment. Supraorbital fractures are preferably accessed through a coronal incision, but may be exposed through a suitable laceration overlying the fracture site.17

Figure 10.4. Intraoperative photo of reconstruction/frontal sinus cranialization of the case shown in Figure 10.2. The fracture was approached through a coronal incision.
10.4 Nasal Fractures
Because of its prominence, fractures of the nose are the most common facial bone injury. The nose may be nondisplaced, or dislocated with both lateral and posterior displacement in frontal-impact injuries. The diagnosis of nasal fracture is suggested by epistaxis, bruising, laceration and swelling over the nose, and distortion of the appearance of the nose with lateral deviation or flattening. Intranasal inspection may reveal septal deviation or septal lacerations. Periorbital hematomas accompanying nasal fractures are diffuse and are not confined by the orbital septum to the boundaries of the orbital rim as with internal orbital fractures. At least one-third of nasal injuries have a small laceration over the nasal bridge. CT imaging delineates the exact anatomy of the displacement of all fracture segments, directing efforts at a closed reduction.
Nasal fractures are generally treated by closed reduction of the septum and nasal pyramid. General anesthesia, as opposed to an external nasal field block, facilitates an accurate closed reduction. Nasal fractures are first completed by thoroughly mobilizing the nasal pyramid in both lateral directions with Asch forceps. The septum is then restabilized at the facial midline. After completion and restabilization, the septum should be supported by Doyle splints and the nasal pyramid supported by an external nasal splint. Acute open reductions of the septum are discouraged, as they are associated with a higher incidence of septal perforation.
10.5 Orbital Fractures
Orbital fractures are commonly associated with combined periorbital and subjunctival hematomas.18 Anesthesia is routinely present along the distribution of the infraorbital nerve, producing numbness in the ipsilateral nose, cheek, upper lip, and anterior maxillary teeth. Diplopia may be present with superior and inferior gaze owing to contusion or, less commonly, entrapment of the fascial suspensory system of the inferior rectus and inferior oblique extraocular muscles. A forced duction examination may be performed if extraocular muscle entrapment is suspected. Resistance or total blockage of rotational movement implies frank incarceration of the muscle or ligament system, or hemorrhage adjacent to the extraocular muscle system.
Fractures of the orbit are accompanied by globe injury in 10% of cases.19 Corneal abrasions are most common, but globe laceration and rupture must always be suspected. A visual screening examination is mandatory for every orbital fracture, and consists of visual acuity, pupillary reaction, examination of the anterior and posterior chambers, and intraocular pressure. Injury to the optic nerve must also be evaluated; the most subtle sign is a pupil sluggishly reactive to light (Marcus Gunn pupil).
Classically, orbital floor fractures involve the inferomedial portion of the orbit (Figure 10.5). The pupil is displaced inferiorly, medially, and posteriorly. Orbital emphysema may or may not be present along with palpable crepitus. Ipsilateral epistaxis is almost invariably present. Exophthalmos is a common initial finding and the result of intraorbital swelling or hemorrhage. As swelling and hemorrhage subside, the globe sinks into an orbit that has been enlarged by the fracture, eventually resulting in enophthalmos and globe retrusion. The radiographic examination of orbital fractures consists of axial, coronal, and sagittal CT views with both bone and soft tissue windows.

Figure 10.5. Coronal view of a right orbital fracture involving the medial, inferior, and lateral orbital walls. Note the opacity of the maxillary sinus, inferior displacement of orbital contents into the maxillary sinus, and subcutaneous emphysema.
Absolute indications for surgery are significant enophthalmos or muscle entrapment, as confirmed by forced duction and CT. With gross displacement of floor and medial wall fractures, operative repair is indicated to prevent late enophthalmos.20 Fractures of the inferior orbital rim, especially those involving the infraorbital foramen, are generally reduced to decompress the infraorbital nerve.
Fractures isolated to the orbital floor and medial wall may be approached by a midlid, infraorbital, subciliary, conjunctival, or coronal incision (Figure 10.6).21 Subciliary incisions, while usually providing the best exposure, have the highest incidence of ectropion.22 The exposure afforded with conjunctival incision can be increased with lower lid division or lateral canthotomy. The edges of the orbital floor or medial wall fracture are defined, and a suitably sized bone graft or alloplast (i.e., Medpor) is obtained and curved to the wall diameter (Figure 10.7).23,24 The bone graft or alloplast is then stabilized by fixation to the orbital rim.

Figure 10.6.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


