It has been 50 years since the landmark presentation by Hugo Obwegeser at Walter Reed Army Hospital. At that conference, Professor Obwegeser offered American surgeons techniques to correct facial skeletal deformities with access through intraoral incisions. As important advances in surgical technique and anesthesia evolved for the surgical procedures, a major contribution by American orthodontists in collaboration with surgeons was the creation of a common diagnostic, planning, and treatment scheme for use by both clinician groups in the treatment of dentofacial deformities, the skeletal and dental problems of the most severely affected 5% of the population. This article summarizes what American orthodontists and surgeons have learned in the late 20th and early 21st centuries, and forecasts what might be the future of treatment for patients with dentofacial deformities.
Highlights
- •
Interactive treatment planning.
- •
Coordinated orthodontic and surgical treatment procedures.
- •
Sequence of treatment.
- •
Surgeon-orthodontist interactions during treatment.
- •
A 21 st century perspective: what does the future hold?


Although occasional mandibular surgery to set back the mandible was performed in the first half of the 20th century, modern orthognathic surgery began in the 1950s with the introduction of ramus osteotomy to reposition the tooth-bearing segments of the mandible. The use of a fixed orthodontic appliance for presurgical and postsurgical orthodontics and for stabilization at surgery followed quickly. The key surgical procedures, bilateral sagittal split ramus osteotomy (BSSO) and LeFort I down-fracture, were introduced in the 1960s, instigated by Professor Hugo Obwegeser, who showed American surgeons how to correct facial skeletal deformities through intraoral incisions. Since then, the combined efforts of orthodontists and surgeons have led to steady progress in efficient and predictable treatment outcomes, with the options of 3-dimensional (3D) imaging and computer-assisted surgical planning the most recent advances.
The purpose of this article is to provide an overview of how current surgical-orthodontic treatment evolved, with an emphasis on what has been learned about the controversial aspects of diagnosis and treatment planning, the coordination of orthodontic and surgical treatment, and computer applications for planning surgical procedures and evaluating outcomes. Although any prediction of the future is problematic, based on our collective experience we offer what we see evolving in the decades ahead as treatment for patients with dentofacial deformities.
Orthognathic surgery procedures
Most orthognathic surgery patients now are treated with 1 or both of 2 procedures developed in the late 1950s and 1960s: BSSO of the mandibular ramus and LeFort I osteotomy of the maxilla via down-fracture, refined by American surgeons.
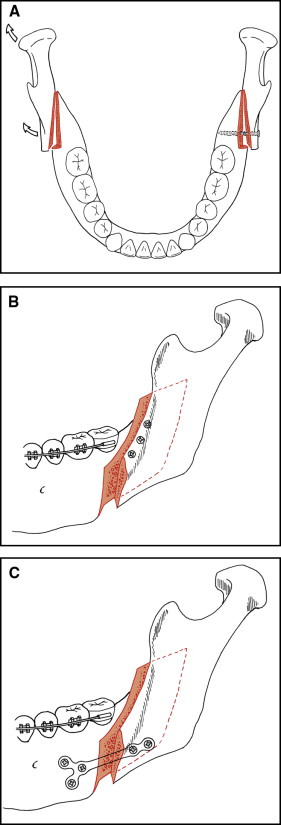
The basic technique of BSSO has not changed, but some important modifications have been introduced in recent years. The key element in this surgical procedure is the split within the ramus to obtain good bony apposition of the condylar and body segments after the body segment has been repositioned ( Fig 1 ). The current emphasis is on completing the procedure with minimal trauma to the inferior alveolar nerve. The steps in the surgery and the critical elements are discussed in detail in current texts.
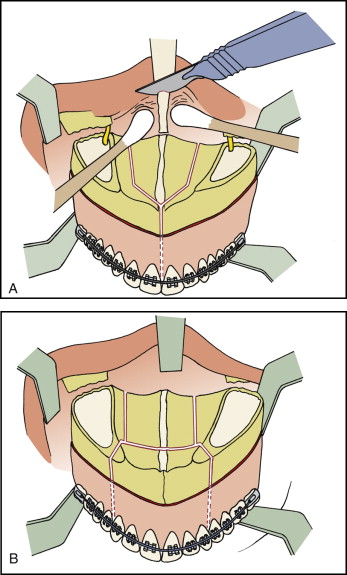
As with BSSO, the basic technique of the LeFort I down-fracture remains unchanged, with important modifications through the years. Its critical element is osteotomy cuts that make down-fracture possible, giving access to superior structures so that segmentation of the maxilla and modifications in the nose are possible ( Fig 2 ). This surgery also is described and illustrated in detail in current texts. The combination of these surgeries occurs frequently in current orthognathic surgery.
In the later decades of the 20th century, lower border osteotomy of the mandible was added more often to the surgical plan. This procedure allows repositioning of the bony chin in all 3 planes of space ( Fig 3 ). In contrast to BSSO and LeFort I down-fracture, it has not been widely presented in the orthodontic literature.
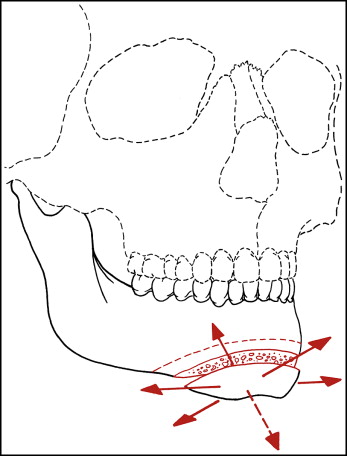
In patients with true mandibular asymmetry, the chin often is deviated to 1 side more than the dentition is, and repositioning the chin along with a ramus osteotomy to achieve normal occlusion and symmetry often is preferred. The bony chin can be moved backward, but the limitation with backward movement is the relaxation of the soft tissues over the chin. The effect of backward movement can be an unesthetic wrinkling of the skin. Moving the chin forward or up can be achieved by angling the direction of the osteotomy cut upward; moving it down requires a bone graft but is quite feasible.
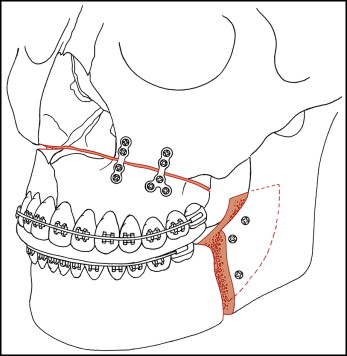
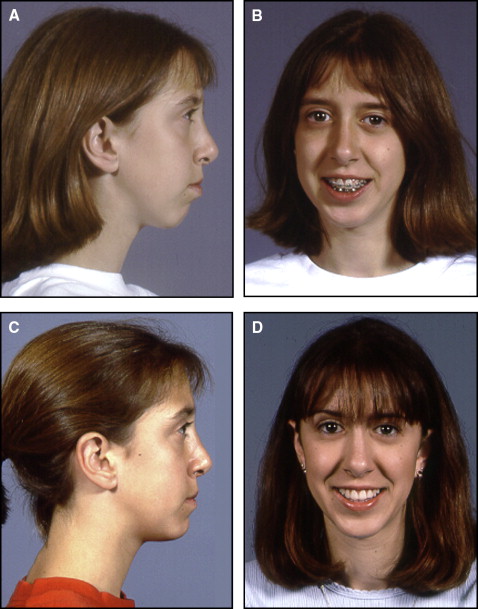
A lower border osteotomy to move the chin upward and forward is termed a functional genioplasty because it allows normal lip function after correction of excessive chin height and inadequate chin projection. The procedure can be done at any time after the mandibular canines erupt. It is much less invasive than LeFort I or mandibular ramus surgery ( Fig 4 ) and can greatly improve the functional and esthetic outcomes of orthodontic treatment for long-face Class II patients. An important recent finding is that bone remodeling above and behind the chin segment is better when this surgery is done before age 15 years than in older adolescents, and the results are better in older adolescents than in adults. Genioplasty is an underused component of comprehensive orthodontic treatment at present.
With surgically assisted rapid palatal expansion (SARPE), transverse expansion of the maxilla is an important part of current orthodontic therapy. Before age 8 or 9 years, the midpalatal suture can be opened with a relatively light force delivered by a lingual arch (jackscrew devices are contraindicated at those ages). By the beginning of adolescence, a heavier force from a jackscrew is needed to fracture overlapping bone spicules at the suture, and by late adolescence even a heavy force from a jackscrew is unlikely to open the suture.
The original idea with SARPE was that making horizontal cuts in the lateral walls of the maxilla would reduce resistance to expansion enough to allow a fracture at the midpalatal suture. As the surgical technique developed, additional cuts were added to decrease the chance of an uncontrolled fracture (which could have disastrous consequences such as uncontrolled bleeding without access to the ruptured vessels or sensory nerve damage). In the evolved technique, all the cuts needed for a LeFort I down-fracture seem necessary, even without completing the mobilization of the maxilla. SARPE, therefore, is not a minor surgical procedure. If the only thing a late adolescent or an adult patient needs is transverse expansion, it may be the preferred approach. If the patient would need a later LeFort I osteotomy for vertical or anteroposterior repositioning of the maxilla, SARPE is sometimes justified as the first stage of 2-stage surgery because the required maxillary expansion would be more stable than with a segmental maxillary osteotomy included in a 1-stage surgical plan.
The best data now available indicate that the typical amount of skeletal expansion with SARPE is less than the expected 50% of the outcome with jackscrew expansion at earlier ages, and that there is significant relapse of the dental component of expansion. The presumably greater transverse stability of SARPE followed by LeFort I maxillary surgery is not an indication for avoiding segmental osteotomy for expansion with a LeFort I procedure.
Treatment outcomes: short-term and long-term stability
Much of what had been learned during the 20th century about postsurgical stability with orthognathic procedures is summarized in chapter 12 of Contemporary Treatment of Dentofacial Deformity . There are 2 important points to keep in mind when stability is considered.
- 1.
Mean changes and statistical analysis based on the assumption of a normal distribution of outcomes after surgery tend to be misleading because a few patients typically have most of the changes. It often is more useful to discuss postsurgical stability with patients in terms of the percentage of patients who have clinically significant changes: ie, “Ms Jones, there are 4 chances out of 5 that you will have little or no postsurgical change, but you should understand that means there is a 20% chance of change toward your original jaw position.”
- 2.
Although it seems reasonable that postsurgical changes related to the surgery itself should be completed well within the first year, this simply is not true. Changes often continue to 5 years postsurgery and look as if the patient is having further growth in the pattern that produced the problem initially, even though he or she would seem too old to have that much growth.
Regarding Class II and Class III stability, during the first postsurgical year, the jaw relationship in patients who have had mandibular setback surgery tends to be unstable. In the past before rigid fixation was available, up to 50% had more than a 2-mm relapse forward in chin position, and 15% to 20% had greater than a 4-mm change. The percentages have improved with rigid fixation, but still mandibular setback is a potentially problematic procedure. Mandibular stability is better in Class III patients who have 2-jaw surgery. For Class III patients with isolated maxillary advancement, there is an 80% chance of no significant change (<2 mm) in the postsurgery position of the maxilla and essentially no chance of more than a 4-mm change.
In contrast, in patients who have mandibular advancement surgery with rigid fixation, there is a minimal (<5%) chance of greater than a 4-mm relapse at the chin in the first postsurgical year, and about a 20% chance of more than a 2-mm relapse, but almost as many patients have more than 2 mm of forward positioning of the chin. Patients with the most stable mandibular advancements are those who had downward movement of the chin to increase anterior face height. Rotation of the mandible superiorly to decrease anterior face height in a long-face patient continues to be notoriously unstable without augmented fixation, and patients with this treatment need further documentation from larger case series before reliable and predictable outcomes evolve.
The stability situation for orthognathic surgery reverses itself beyond 1 year; then the Class III patients are more stable than the mandibular advancement ones. Age at surgery is a factor. At 5-year recall, maxillary or 2-jaw surgery patients who were selected for early (adolescent) Class III surgery because mandibular growth had subsided to adult levels were as stable as older patients with the same surgery; both groups had about an 80% chance of less than a 2-mm change. In contrast, Class II patients treated with mandibular advancement surgery at ages when growth should have been completed were significantly more likely to have backward movement of the chin than those treated at an earlier age, but overjet was stable even if chin position changed because of mandibular incisor proclination when the mandible moved posteriorly.
Superior repositioning of the maxilla via LeFort I osteotomy was the first successful way to correct long-face and open-bite problems. Many of these patients also have a mandibular deficiency, and mandibular advancement is combined with moving the maxilla up. With rigid fixation this is quite stable during the first postsurgical year, but downward movement (growth) of the maxilla causes about a 20% chance of more than a 2-mm long-term increase in face height by the 5-year recall.
The recent adoption of strategically placed bone plates or screws for skeletal anchorage allows orthodontic treatment to intrude the maxillary posterior teeth. This shows promise for the correction of less severe open bites (<6 mm of correction needed). Based on the data, at 1 and 2 years postintrusion its stability is similar to that of LeFort I surgery to close open bites. Interestingly, the amount of superior repositioning of the maxilla at surgery is not related to postsurgical stability.
Orthodontist and surgeon interactions: who does what, when, and why
Until the 1960s, surgeons and orthodontists tended to work independently to correct dentofacial deformities. It soon became apparent that there were problems if surgery was done first, and it was left to the orthodontist to finish the treatment. Neither the orthodontist nor the surgeon understood the other’s treatment limitations. Orthodontists often had difficulty because the surgeon failed to position the jaw so that the orthodontist could adequately define the occlusion. Similar problems arose if the orthodontic treatment was done first and the surgeon had to complete the treatment. These problems were largely resolved by a treatment sequence that began with interactive treatment planning and continued with a pretreatment agreement on a sequence that involved orthodontic preparation for surgery, surgery with archwires used for stabilization, and a relatively short period of postsurgical orthodontic finishing. Planning to keep postsurgical treatment short appears to improve patient satisfaction with treatment. This remains the standard approach to comprehensive surgical-orthodontic treatment, although some clinicians now are again advocating surgery first (see discussion below).
Interactive diagnosis and treatment planning
In the patient evaluation, most young adults with a dentofacial deformity are otherwise healthy. If so, a procedure under general anesthesia is not contraindicated. In practice, patients are often discharged to home on the day of surgery. Older patients who for various reasons have delayed treatment can have orthognathic surgery, even up to and beyond age 60 years. Obviously, these patients can have medical problems requiring adjustments to treatment plans, even to the extent of accepting less-than-ideal outcomes. All involved must understand this before treatment begins.
Dentofacial proportions in potential surgical patients should be evaluated thoroughly, with a recommendation for orthognathic surgery or orthodontics alone based on the evaluation. Two-dimensional computer image predictions of profile changes from repositioning the jaws or the teeth are now reasonably accurate in nongrowing patients, who constitute most potential surgical patients. Imaging has been shown to improve the patient’s understanding of the changes that would result from surgery or orthodontic camouflage (correcting the dental occlusion but not repositioning the jaws), without creating a risk of later claims of inadequate treatment, and make it easier for the treatment team to decide what combination of tooth movement and surgical repositioning would be optimal for the patient.
An important question now is whether 3D imaging is needed to improve diagnosis and treatment planning for surgical patients. The guideline is reasonably straightforward: 3D radiographic imaging (typically cone-beam computed tomography) is so much better in the analysis of patients with major asymmetry that it now is the standard of care, and 3D photography for these patients is advantageous. By comparison, adequate diagnosis and initial treatment planning for most other surgery patients can be done with 2-dimensional cephalometric radiographs and photographs. For patients with temporomandibular joint problems, magnetic resonance imaging rather than radiographs of the joints is indicated.
Three-dimensional radiographs also facilitate the surgical planning for patients with complex problems and may be needed at that stage, even though they were not used initially (see discussion below).
A key question from the evaluation of dentofacial proportions is the extent to which orthodontic camouflage can meet the requirement of acceptable posttreatment facial appearance, without surgery.
For Class III patients, orthodontic camouflage is a combination of forward movement of the maxillary teeth and retraction of the mandibular incisors. It can be quite successful in patients of Asian descent because they tend to have proclined mandibular incisors, but it is much less useful when the mandibular incisors are upright or tilted lingually, as they usually are in patients of European descent. Because retracting the mandibular incisors increases the relative prominence of the chin, this can make the facial appearance worse rather than better. Extracting the mandibular first premolars to provide space for a major retraction of the incisors is rarely a good idea; extracting 1 mandibular incisor allows modest retraction and often does not lead to the tooth-size discrepancy that might be expected. The discrepancy decreases and may even disappear with upright mandibular incisors and proclined maxillary incisors. Bone screws in the mandibular ramus can provide enough anchorage to retract the entire mandibular arch, although doing this requires extraction of the third molars and often the second molars as well.
For Class II patients, camouflage is just the reverse: retraction of the maxillary incisors and proclination of the mandibular incisors. With skeletal anchorage, it is easy now to retract the maxillary incisors too much. They should not be retracted beyond the point that the upper lip is vertical—a backward slope of the lip is unesthetic. Proclination of the mandibular incisors can be camouflaged with genioplasty as described above ( Fig 5 ), and genioplasty extends the amount of advancement of the mandibular incisors that can be compatible with a normal facial appearance.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


