Dental implants provide completely edentulous and partial edentulous patients the function and esthetics they had with natural dentition. It is critical to understand and apply predictable surgical principles when treatment planning and surgically restoring edentulous spaces with implants. This article defines basic implant concepts that should be meticulously followed for predictable results when treating patients and restoring dental implants. Topics include biological and functional considerations, biomechanical considerations, preoperative assessments, medical history and risk assessments, oral examinations, radiographic examinations, contraindications, and general treatment planning options.
Key points
- •
Dental implants provide a predictable, effective, and reliable means to replace dentition.
- •
Dental implants provide completely edentulous and partial edentulous patients the function and esthetics they had with natural dentition.
- •
It is critical to understand and apply predictable surgical principles when treatment planning and surgically restoring edentulous spaces with implants.
- •
Basic implant concepts should be meticulously followed for predictable results when treating patients and restoring dental implants.
Implant basic concepts
Dental implants provide a predictable, effective, and reliable means for tooth replacements. Additionally, dental implants provide completely edentulous and partial edentulous patients the function and esthetics they had with natural dentition. It enables patients to regain normal masticatory function, esthetics, speech, smile, and deglutition. In patients with orofacial pain, it may resolve painful symptoms as well as improve facial esthetics and appearance. Edentulous patients gain a feeling of higher self-esteem and well-being. In patients with craniomaxillofacial defects, implants can be used to replace ears, noses, eyes, and other maxillofacial defects. Moreover, congenital, traumatic, and developmental oral defects can be treated with implants.
Implant basic concepts
Dental implants provide a predictable, effective, and reliable means for tooth replacements. Additionally, dental implants provide completely edentulous and partial edentulous patients the function and esthetics they had with natural dentition. It enables patients to regain normal masticatory function, esthetics, speech, smile, and deglutition. In patients with orofacial pain, it may resolve painful symptoms as well as improve facial esthetics and appearance. Edentulous patients gain a feeling of higher self-esteem and well-being. In patients with craniomaxillofacial defects, implants can be used to replace ears, noses, eyes, and other maxillofacial defects. Moreover, congenital, traumatic, and developmental oral defects can be treated with implants.
Biological and functional considerations
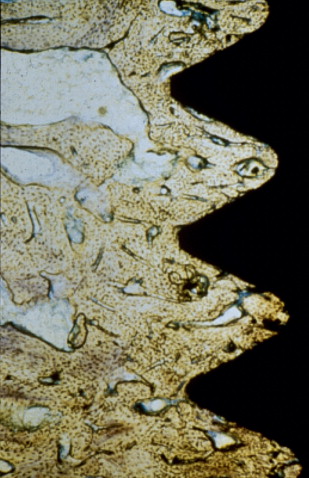
Osseointegration is the primary goal of implant placement. In 1952, Brånemark began extensive studies on the microscopic circulation of bone marrow healing. These studies led to a dental implant application in the early 1960s in which a 10-year implant integration was established in dogs without significant adverse reactions in the soft and hard tissues. Osseoeintegration can be defined as the direct structural and functional connection between organized, living bone and the surface of a load-bearing implant without intervening soft tissue between the implant and bone. Clinically, osseoeintegration can be defined as the asymptomatic rigid fixation of an implant in bone with the ability to withstand occlusal forces. Rigid fixation is a clinical term that implies no observable movement of the implant when a force of 1 to 500 g is applied ( Fig. 1 ).
Advancements in biomaterials, implant science, and nanotechnology; improved biotechnology; and an understanding of the bone–implant interface have resulted in improved outcomes and an expanded utilization of implants. Improved imaging techniques help aid in diagnosis; a varied availability of implant geometries, surfaces, and refined surgical techniques has made it possible for most healthy patients to receive implants. Numerous materials are available to aid in bone regeneration in the maxillofacial region, including bone substitute composite grafts and autogenous bone. These tissue types involve the key concepts of osteogenisis, osteoinduction, osteoconduction, and osteopromotion ( Boxes 1 and 2 ).
- •
Informed consent
- •
Perioperative antibiotics
- •
Imaging modalities
- •
Documentation
- •
Atraumatic surgery
- •
Biocompatible material
- •
Placement of implant with initial stability
- •
Immobility of implant
Surgical preparation in a standard sterile fashion is recommended for all implant procedures. The goal is to minimize mechanical and thermal injuries to the bone. Osteotomies should be completed under copious irrigation using sharp osteotomy drills at high torque and slow speed. It is critical to maintain bone temperatures under 47°C. Bone necrosis and failure of integration can occur when temperatures exceed 47°C.
The material of choice for implants needs to be biocompatible with bone and biologically inert. Titanium is an optimal material that encompasses both of these required qualities.
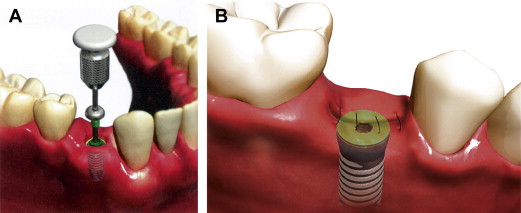
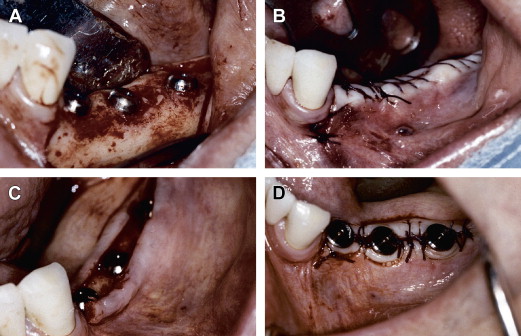
Volume and quality of bone that contacts the implant determine its initial stability. This stability must be maintained in order for bone to form at the implant surface. Immobility of the implant is imperative for successful osseoeintegration. Implants can be placed using a staged surgical plan depending on the initial stability and quality of bone available. A single-stage surgery requires adequate primary stability and can be loaded immediately. A 2-staged approach requires submerging the implant when initial stability is less than adequate. A surgical uncovering and placement of healing abutment is required in 3 to 4 months ( Figs. 2 and 3 ).
Soft tissue
Understanding and managing the peri-implant soft tissue are critical to long-term success clinically and esthetically. The soft tissue consists of connective tissue covered by epithelium, extending into an epithelial lined sulcus. Junctional epitheliam lines the most apical portion, which forms an attachment. Soft tissue thickness should be assessed prior to surgery, noting that soft tissue thickness affects the vertical edentulous space. The minimum vertical space needed for a cemented crown is 9 mm; however, the tissue thickness is as much as 3 mm in the posterior mandible, affecting the depth of implant placement.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


