Armamentarium
|
History of the Procedure
Attempts have been made since the 1880s to remove the infected section of the root of a tooth and leave the remaining portion in the oral cavity. Complete regeneration of previously infected periapical areas was demonstrated with bone fill histologically in 1930. Techniques referred to as ‘‘retrograde filling,’’ ‘‘retrofill,’’ or ‘‘retroseal’’ began to appear in the literature in the mid-twentieth century. These terms can be defined as the resection and preparation of the root tip and insertion of a root-end filling in the prepared cavity while leaving the main portion of the tooth intact. Surgical endodontic success rates have dramatically improved over the years due to the development of new retrofilling materials and the increased use of ultrasonic preparation of the retrograde site. Previously, success rates had been documented at 60% to 70%; these have since increased to 90% or greater.
History of the Procedure
Attempts have been made since the 1880s to remove the infected section of the root of a tooth and leave the remaining portion in the oral cavity. Complete regeneration of previously infected periapical areas was demonstrated with bone fill histologically in 1930. Techniques referred to as ‘‘retrograde filling,’’ ‘‘retrofill,’’ or ‘‘retroseal’’ began to appear in the literature in the mid-twentieth century. These terms can be defined as the resection and preparation of the root tip and insertion of a root-end filling in the prepared cavity while leaving the main portion of the tooth intact. Surgical endodontic success rates have dramatically improved over the years due to the development of new retrofilling materials and the increased use of ultrasonic preparation of the retrograde site. Previously, success rates had been documented at 60% to 70%; these have since increased to 90% or greater.
Indications for the Use of the Procedure
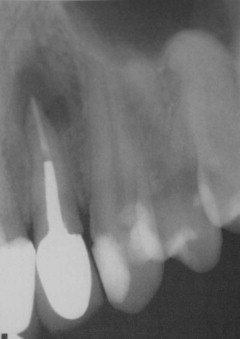
There are two main indications for apicoectomy in selected teeth. The first category comprises teeth with active periapical pathology with adequate endodontic therapy. These are teeth that continue to be symptomatic with clinically sound conventional orthograde endodontic therapy ( Figures 15-1 and 15-2 ).

The second category of teeth indicated for apicoectomy comprises those with active periapical pathology with inadequate endodontic therapy that cannot be retreated because of one of the following factors:
- •
Severely curved roots
- •
Presence of a post and core
- •
Silver point filling
- •
Broken instrument (hand file)
- •
Fracture at the apical one third of the tooth
- •
Perforation of the apex
- •
Calcified canals
Limitations and Contraindications
There are several contraindications to periradicular surgery. One such contraindication is teeth with short roots; if apicoectomy is performed on these teeth, it will reduce the size of the tooth, leading to an inadequate crown-to-root ratio and ultimately to root fracture and surgical failure.
Another contraindication to apicoectomy is a tooth with a root that is inaccessible secondary to anatomic structures, such as the maxillary sinus, inferior alveolar nerve, mental nerve, greater palatine foramina, and incisive foramen. Teeth that have marked periodontal disease or are prosthodontically nonrestorable also are not amenable to periradicular surgery. Finally, as with any surgical procedure, patients who are medically compromised should not undergo periradicular surgery.
Technique: Apicoectomy
Incision Design
The surgical plan must be laid out in detail before the initial incision is made. The design of the incision depends on several factors, including the tooth’s position in the arch, the presence of fixed prosthodontic restorations, the extent of periapical abscess, and gingival recession.
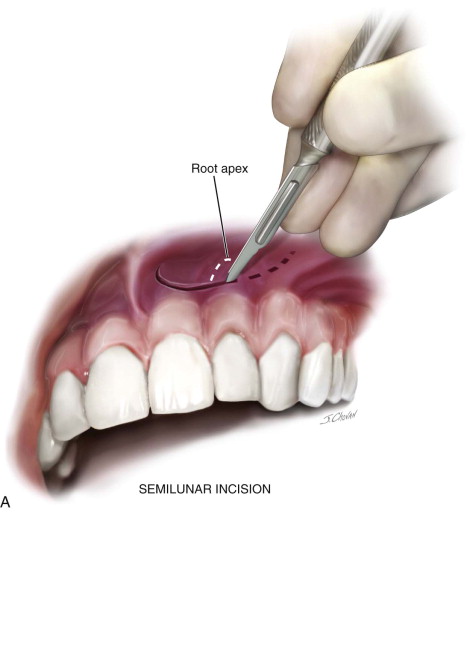
Several incision designs are commonly used to perform an apicoectomy. The first we will discuss is the semilunar flap ( Figure 15-3, A ). Classically, this flap is used in the region of the anterior maxilla. It is a semicircular flap with the concave portion of the incision hanging cervically. The exact location of the root apex must be known for this incision to be successful. Wound healing problems have been reported to be a drawback of this incision; therefore, the incision must be made such that the closure is over healthy bone.
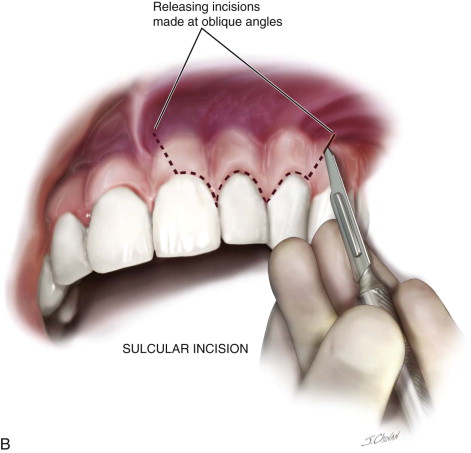


Another incision design is the sulcular flap ( Figure 15-3, B ). The incision is made in the gingival sulcus one tooth anterior to the tooth undergoing apicoectomy and is carried to one tooth posteriorly.
After the sulcular incision, one or two releasing incisions are made at an oblique angle so that the base of the flap is wider than the apex. These releasing incisions are made at the distal line angles of the two teeth immediately adjacent to the tooth in question to preserve the dental papilla. If the surgeon is unsure of the exact location of the tooth apex, if there is a large periapical lesion, or if the patient requires bone grafting in the area, this design is the incision of choice. A disadvantage of the sulcular flap is recession of the gingiva, which can be unesthetic in the region of the anterior maxilla, especially in dentition with fixed prosthodontics.
More recently, reports have described a “submarginal flap” ( Figure 15-3, C ). This essentially is a combination of the sulcular and semilunar flaps. A horizontal incision is made no less than 2 mm from the sulcus of the affected tooth, and a releasing incision is made mesially and distally. The submarginal flap is more commonly used in areas of gingival recession.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


