Introduction
In this study, we aimed to evaluate the reasons for failure of orthodontic treatment for impacted maxillary canines and to recommend measures to overcome them.
Methods
Twenty-eight patients (ages, 17.4 ± 4.3 years) with 37 maxillary impacted canines were referred after a failed attempt to resolve the impaction. Reasons for failure were analyzed, and corrective measures undertaken. The success rate of the revised treatments and the durations of both treatments were recorded.
Results
The mean duration of the failed treatments was 26.2 ± 17.2 months. The failed treatments were mostly based on plane radiographs, intra-arch dental anchorage, and elastic traction directly to the labial archwire. The major reasons for failure were inadequate anchorage (48.6%), mistaken location and directional traction (40.5%), and ankylosis (32.4%). In several patients, there was more than 1 possible reason for failure. The success rate of the revised treatments was 71.4%, and the mean duration was 14.4 ± 7.2 months. Repeat surgery was needed for 62.9% of the canines in which corrective treatment was started, mostly to redirect the ligature wires. The corrective measures included the use of 3-dimensional imaging and a change in the direction of traction. Anchorage was reinforced by dental and skeletal means.
Conclusions
Inaccurate 3-dimensional diagnosis of location and orientation of impacted teeth and failure to appreciate anchorage demands were the major reasons for failure in the treatment of impacted canines.
Today, most patients seeking correction of malalignment and malocclusion of the erupted dentition are assured of a predictable, superb treatment outcome. This is reflected in the exacting demands established by the various examining bodies that have been set up worldwide to regulate the admission of professionals aspiring to the rank of specialist orthodontist or an equivalent title, and in the case presentations published in the clinical orthodontic literature.
However, when the patient’s malocclusion includes an impacted tooth, particularly a maxillary canine, some apprehension, doubt, or uncertainty creeps into the equation. The proposed treatment plan is usually accompanied by a warning to the patient that treatment of this particular element in the overall treatment plan might fail.
The chief reason for this striking contrast includes the many complicating factors related to the impacted tooth that are not normally present in a fully erupted dentition. Thus, it is difficult to determine accurately the 3-dimensional (3D) position of the tooth in relation to both its crown and root, and the proximity to the roots of other teeth. It is nearly impossible to clinically examine for crown anomaly, color, shape, mobility, and pathology of an impacted tooth. Surgery is needed, and it is difficult to determine directionally suitable orthodontic forces that will resolve the impaction, and whether they should include extrusion, rotation, crown tipping, or root uprighting components. Treatment is likely to be extended and painful, and the periodontal prognosis of the outcome is difficult to predict.
Analysis of the reasons for failure must consider many factors, which can be roughly divided into 3 groups as follows.
- 1.
Patient-dependent factors: abnormal morphology of the impacted tooth, age, pathology of the impacted tooth, grossly ectopic tooth, resorption of the root of an adjacent tooth, and lack of compliance (eg, missed appointments, inadequate oral hygiene).
- 2.
Orthodontist-dependent factors: mistaken positional diagnosis and inappropriate directional force, missed diagnosis of resorption of the root of an adjacent tooth, poor anchorage, inefficient appliance, and inadequate torque.
- 3.
Surgeon-dependent factors: mistaken positional diagnosis, exposure on the wrong side, or rummaging exposure; injury to the impacted tooth; injury to an adjacent tooth; soft-tissue damage; and surgery without orthodontic planning.
The purpose of this article was to examine the records of patients with an impacted tooth whose original orthodontic treatment did not resolve the impaction. The patients were referred to one of the authors. We analyzed the reasons for failure of the initial treatment approach, devised an alternative treatment approach, and evaluated its success.
Material and methods
A sample of 28 patients (18 female, 10 male; ages, 17.4 ± 4.3 years) with 37 impacted canines was assembled from the private practices of the 3 authors. The patients’ initial records showed that 26 impactions were palatal, 9 were buccal, and 2 were in the midalveolus. All patients had been treated elsewhere for a malocclusion that included at least 1 impacted maxillary canine that did not respond to treatment. They were referred by general practitioners or orthodontists and were taken consecutively in the referral system for inclusion in our investigative sample. In this study, an orthodontist was defined as a dentist who has received specialty training in a state-recognized university graduate orthodontic course.
Of the sample, 9 patients had bilateral impaction of the canines, and each failed canine was considered separately in the study. From the patient records, the following treatment information was gathered.
- 1.
Details related to the initial treatment: had the treating practitioner received specialist orthodontic training (as detailed above) with more or less than 10 years of postgraduation experience, or was he or she a general practitioner with more or less than 10 years since graduating from dental school; was the patient transferred in relation to the surgical exposure (before, after); was the patient transferred in relation to the stage of orthodontic treatment (before orthodontic treatment or after the failed treatment); was radiographic documentation used for the original diagnosis; how many times was surgical exposure performed on the tooth; was the surgery successful; how was traction applied (patients were differentiated into those whose traction was performed directly to the labial archwire and those whose traction had 2 stages, first vertically downward to clear the root of the incisor and then laterally into its place in the arch); was the anchorage base intra-arch dental, interarch dental, extraoral, or implant; how much time elapsed between the start of treatment and the realization of failure; and what were the assumed reasons for failure.
- 2.
Details related to the second orthodontic treatment: were additional radiographic records needed; what was the outcome of revised treatment (success or failure); how long was the revised treatment; what were the revised reasons for initial treatment failure; and what corrective measures were adopted (new surgery, altered direction of traction, reinforced anchorage).
Results
The patients were referred by 26 clinicians. Twenty were specialists, including 15 who had over 10 years of experience, and 6 were general practitioners, including 3 with more than 10 years of experience. Most patients (26 of 28; 92.9%) were referred after surgery had been performed. In 2 (patients 11 and 22), space had been prepared for the impacted teeth without surgery. It had been optimistically expected that the teeth would erupt spontaneously, but that had not occurred. Twenty-five patients (89.3%) had been referred during active orthodontic treatment and 3 after the treatment was stopped because of failure.
Table I describes the initial treatment plans. Panoramic and cephalometric films were available for all patients, together with variable numbers of periapical views. Two patients had undergone 3D imaging, one (patient 8) with conventional spiral computed tomography (CT), and the other (patient 12) with cone-beam CT (CBCT). Among the 35 canines that had previously been exposed, 10 (28.6%) had had 3 such episodes. In 1 bilateral case (patient 3), who had been treated by open exposure, the bonded attachments had failed on both canines, and the tissues had subsequently rehealed over the teeth. In 2 (patients 6 and 24), the surgeon had failed to find the impacted tooth because of misdiagnosis of labiolingual location.
| Patient | Records | Surgeries (n) | Traction | Duration (mo) | Assumed reason for failure |
|---|---|---|---|---|---|
| 1 | P, C, Pa | 1 | D | 72 | Unknown |
| 2 | P, C, Pa | 1 | D | 40 | Unknown |
| 3 | P, C, Pa, O | 2 | D | 10 | Attachment failure |
| P, C, Pa, O | 2 | D | 10 | Attachment failure | |
| 4 | P, C, Pa | 1 | D | 12 | Unknown |
| 5 | P, C, Pa | 1 | D | 54 | Unknown |
| 6 | P, C, O | 1 | X | 10 | Surgical |
| 7 | P, C, Pa | 3 | D | 8 | Attachment failure |
| 8 | CT | 1 | D | 20 | Ankylosis, incisor root resorption |
| 9 | P, C, Pa | 1 | D | 36 | Not enough time |
| 10 | P, C, Pa | 1 | D | 32 | Erupted intractable |
| P, C, Pa | 1 | D | 32 | Erupted intractable | |
| 11 | P, C, Pa | – | X | 54 | Inadequate follow-up |
| 12 | CT | 1 | D | 35 | Ankylosis |
| CT | 1 | D | 35 | Ankylosis | |
| 13 | P, C, Pa | 1 | TS | 48 | Ankylosis, incisor root resorption |
| 14 | P, C, Pa | 1 | D | 36 | Incisor root resorption |
| 15 | P, C, Pa | 1 | D | 23 | Incisor root resorption |
| 16 | P, C, Pa | 3 | D | 39 | Ankylosis |
| 17 | P, C, O | 3 | D | 48 | Ankylosis |
| P, C, O | 3 | D | 48 | Ankylosis | |
| 18 | P, C | D | 12 | Unknown | |
| 19 | P, C, Pa | 3 | D | 28 | Ankylosis |
| 20 | P, C, Pa | 1 | D | 48 | Unknown |
| 21 | P, C, Pa | 1 | D | 30 | Ankylosis |
| 22 | P, C, PA | – | X | 30 | Intractable position |
| 23 | P, C | 1 | D | 18 | Incisor root resorption |
| P, C | 1 | D | 18 | Incisor root resorption | |
| 24 | P, C, Pa | 3 | X | 9 | Surgical |
| 25 | P, C, O | 1 | D | 9 | Ankylosis |
| P, C, O | 1 | D | 9 | Ankylosis | |
| 26 | P, C, O | 3 | TS | 7 | Ankylosis |
| P, C, O | 3 | TS | 7 | Ankylosis | |
| 27 | P, C, Pa | 1 | TS | 7 | Ankylosis |
| P, C, Pa | 1 | TS | 7 | Ankylosis | |
| 28 | P, C, Pa | 3 | TS | 14 | Ankylosis |
| P, C, Pa | 3 | TS | 14 | Ankylosis |
Elastic traction, directly to the arch, was used for 26 canines. For the 7 canines treated in 2 stages, an auxiliary spring was used, with the express aim of erupting the canine into the palate as the initial maneuver. The orthodontic anchorage used in all patients in this sample consisted exclusively of intraoral dental anchorage from other dental units with fixed bonded appliances; this was therefore omitted from Table I . The mean duration of treatment, from start to realization of failure, was 26.2 ± 17.2 months. The reasons for failure, as assumed by the practitioners, were ankylosis (17 teeth, 45.9%), incisor root resorption (6 teeth, 16.2%), intractable position (3 teeth, 8.1%), attachment failure (3 teeth, 8.1%), surgical failure (2 teeth, 5.4%), and inadequate follow-up period (2 teeth, 5.4%). In 6 teeth (16.2%), the orthodontist could find no explanation for the failure, and, for 2 patients, 2 reasons were given.
Table II shows the supplementary records that were considered necessary for each patient. As the result of the new information and consequent practical steps taken, the success rate of the revised treatment plans was 67.6% for the whole group. However, 2 patients (2 canines) refused more treatment, yielding an actual success rate of 71.4%. The mean duration of the new treatment in the successful patients was 14.4 ± 7.2 months. After this, it became possible to diagnose the reasons for failure in each patient more accurately. The major causes were poor anchorage (18 teeth, 48.6%), mistaken positional diagnosis and directional traction (15 teeth, 40.5%), and ankylosis (12 teeth, 32.4%). Seven ankylosed teeth were treated by surgical luxation and subsequent traction, but only 3 were successfully brought in their place in the arch. In 5 patients (6 teeth, 16.2%), resorption of the incisor roots had escaped the practitioner’s notice until treatment was advanced. Three teeth (8.1%) failed to erupt because of interference of soft tissues. In 3 patients (8.1%), inadequate space was considered to be a cause for noneruption. In one (patient 6), surgery was initially performed at the wrong site, and, in another patient (24), the tooth was in an extremely difficult position; therefore, these teeth remained unexposed after surgical intervention. In 2 patients (11 and 22), traction was never applied, and the first practitioner waited in vain for 54 and 30 months, respectively, for the teeth to erupt unaided. Repeated bond failure of the attachments after surgery in 2 patients (3 and 7) accounted for treatment failure. In 1 patient (24), both the first practitioner and the surgeon did not realize that the canine crown was situated on the palatal side between the central and lateral incisors, but its root was labial to the root of the lateral incisor. This created an intractable situation, from which there was no possibility of saving the tooth. In 1 patient (5), the treatment failed because of poor compliance (missed appointments) and inefficient appliances. In several patients, there were 2 or more possible reasons for failure.
| Patient | Additional records | Outcome | Treatment duration (mo) | Revised reasons for failure |
|---|---|---|---|---|
| 1 | No | S | 10 | Direction, space, anchorage |
| 2 | No | S | 6 | Direction, anchorage |
| 3 | No | S | 8 | Attachment failure after surgery |
| No | S | 8 | Attachment failure after surgery | |
| 4 | No | S | 6 | Inadequate space |
| 5 | No | S | 12 | Missed appointments, inefficient appliance |
| 6 | CT | S | 14 | Exposure in wrong site |
| 7 | No | S | 12 | Attachment failure, direction |
| 8 | No | S | 10 | Soft tissue, anchorage, incisor root resorption |
| 9 | No | S | 11 | Direction, space, anchorage |
| 10 | No | S | 17 | Direction, anchorage |
| No | S | 17 | Direction, anchorage | |
| 11 | CT | S | 6 | No traction applied |
| 12 | No | F | – | Ankylosis |
| No | F | – | Ankylosis | |
| 13 | CT | S | 15 | Direction, soft tissue, anchorage, incisor root resorption |
| 14 | Pa | S | 16 | Direction, incisor root resorption |
| 15 | CT | S | 18 | Incisor root resorption, direction, anchorage |
| 16 | No | S | 9 | Ankylosis ∗ , anchorage |
| 17 | No | F | – | Ankylosis, anchorage |
| No | F | – | Ankylosis, anchorage | |
| 18 | No | S | 8 | Direction |
| 19 | CT | No treatment | – | Unknown |
| 20 | CT | No treatment | – | Direction |
| 21 | CT | F | – | Ankylosis, anchorage |
| 22 | CT | S | 30 | No traction applied |
| 23 | CT | S | 27 | Incisor root resorption, direction |
| CT | S | 27 | Incisor root resorption, direction | |
| 24 | CT | F | – | Intractable (pseudotransposition) |
| 25 | No | F | – | Ankylosis, direction |
| No | F | – | Ankylosis, direction | |
| 26 | No | F | – | Ankylosis, anchorage |
| No | F | – | Ankylosis, anchorage | |
| 27 | No | S | 12 | Soft tissue, anchorage |
| No | S | 12 | Soft tissue, anchorage | |
| 28 | Pa | S | 25 | Ankylosis ∗ , anchorage |
| Pa | S | 25 | Ankylosis ∗ , anchorage |
∗ Canines whose ankylosis was resolved with surgical luxation, and the teeth were successfully brought into their place in the arch.
Table III summarizes the corrective measures taken for this group of potentially failed patients. Surgery was needed for 22 of the 35 canines (62.9%). Of these, 7 (in 5 patients) were to redirect the ligature wires to permit a change in direction of traction, 3 (in 3 patients) to clear soft tissues, 7 (in 4 patients) to luxate ankylosed canines; 3 teeth needed bond attachments, and 2 were reoperated to expose them in their newly diagnosed positions. In 2 patients, exposure was performed for the first time. Orthodontic corrective measures included the application of traction in 4 canines to which forces had never been applied. A change in the direction of traction was mandatory for 15 canines. Anchorage was reinforced by various methods in 18 canines and included heavier base archwires, intermaxillary elastics, and temporary implant devices in the more recent cases. Additional space was needed in 2 patients (2 canines).
| Corrective measure | Number of teeth |
|---|---|
| Surgical | |
| Expose in revised (correct) location | 2 |
| Reexpose to bond attachments | 3 |
| Reexpose to change the direction of ligatures | 7 |
| Reexpose to remove soft tissue | 4 |
| Luxation | 7 |
| Total number of teeth reoperated | 22 |
| Expose teeth not previously exposed | 2 |
| Orthodontic | |
| Apply traction when it had not been applied before | 4 |
| Reevaluate position and change direction of traction | 15 |
| Reinforce anchorage | 18 |
| Create space | 2 |
Case presentations
Patient 6 had a mistaken positional diagnosis of the labially impacted canine. The original clinician had referred the patient for full photographic facial and dental records, and cephalometric, panoramic, and anterior occlusal views ( Fig 1 ). Based on these, she assumed that the canine was displaced on the palatal side, close to the midline. Using fixed multibracketed appliances, she had aligned and leveled the teeth to create space in the appropriate location. The patient was then referred to an oral and maxillofacial surgeon for surgical exposure. The surgeon reflected a palatal flap, removed bone on that side of the incisors, but failed to find the canine. He then sutured the flap back to its former place and sent the patient back to the orthodontic practitioner, who consulted with one of the authors (A.B.). Figure 2 shows the aligned and leveled dentition at the consultation visit. It also shows the iatrogenic periodontal defect on the palatal side of the left central incisor, caused by the futile surgical exposure.


Comparing these pictures with the initial clinical photographs shows how this stage of treatment had eliminated the clinical signs that were present initially, which should have indicated to the practitioner and the surgeon that the impacted canine was on the labial side. Moreover, this could have been positively confirmed by using the vertical parallax method of diagnosis, from the plane radiographic panoramic and anterior occlusal views that had been commissioned at the outset ( Fig 1 ).
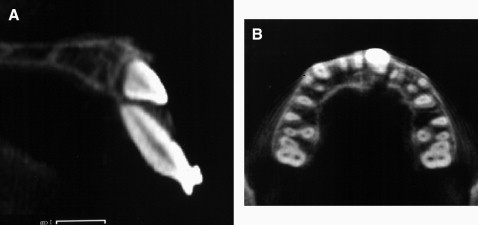
Before the recommencement of treatment, a CBCT image ( Fig 3 ) was taken to diagnose or negate any pathologic changes from the earlier orthodontic and surgical procedures and to accurately locate the tooth in 3 dimensions, along its entire length. The canine was exposed on the labial side ( Fig 4 , A ) and aligned in the normal way with 2-stage traction—first to the labial ( Fig 4 , B ) and then to the distal—to circumnavigate the root of the lateral incisor. The clinical and panoramic views at 5 years posttreatment show the alignment achieved and the similarity between the treated and untreated sides ( Fig 5 , A, B, and D ). However, the palatal gingival defect from the first surgical procedure remained ( Fig 5 , C ).