and Melih Motro2
(1)
Faculty of Dentistry Department of Orthodontics, University of Marmara, Istanbul, Turkey
(2)
Henry M. Goldman School of Dental Medicine Department of Orthodontics & Dentofacial Orthopedics, Boston University, Boston, Massachusetts, USA
Introduction
The main aim in the treatment of cleft lip and palate cases is to achieve labial, palatal, velopharyngeal closure, a balanced profile, harmonic facial appearance, and a good occlusion (Eppley and Sadove 2000; Phua and de Chalain 2008; Cheung and Chua 2006; Jackson et al. 2004; Williams et al. 2001). Most of the time, these goals are accomplished in the early ages. However, in 20–25 % of the patients (Kumar et al. 2006), dentofacial skeletal deformities, and in 4–45 % (Phua and de Chalain 2008) of the patients, oronasal fistula occurrence, which require secondary surgical corrections can be seen. In this subgroup, if there is oronasal fistula, the main needs can be listed as surgical interventions for complete soft tissue coverage and secondary alveolar bone grafting. Also, surgeries that involve both jaws (either orthognathic surgery or distraction osteogenesis) may be necessary too. In severe cases with wide oronasal fistula, the usual approach is covering the gap with buccal, labial mucosal flaps or tongue flaps (Nakakita and Utsugi 1990; Argamaso 1990; Diah et al. 2007). However, tongue flaps may not always be very successful. Some complications, such as flap failure, bleeding, swelling, pain, infection, hematoma, contour deformities, temporary loss of tongue sensation, gustatory changes, requirement for a two-stage or three-stage procedures, and in rare cases, partial or total necrosis of flap can be observed (Elyassi et al. 2011).
Another difficulty of conventional approaches on cleft lip and palate patients is that if there is severe maxillary deficiency, it is hard to achieve the intended advancement due to the tight scarred tissues from the former surgical interventions and possible presence of pharyngeal flap (Eskenazi and Schendel 1992). Even if the intended advancement is achieved, there is always a tendency to relapse due to the same reasons that make the surgery hard (Chua et al. 2010; Hirano and Suzuki 2001).
In such cases, distraction osteogenesis is a good option to overcome the shortcomings mentioned above.
Distraction Osteogenesis
Distraction osteogenesis is a process of new bone formation between the surfaces of osteotomized bone segments that are separated gradually by incremental traction (Cope and Samchukov 2005). The process begins with the osteotomy of the segments and callus formation in between them, followed by gradual traction forces applied to the bone segments, which creates tensional stress in the callus and continues as long as the tissue is stretched. This stretching activity induces new bone formation and adaptive soft tissue changes such as formation of mucosa, muscle, nerve, vascular structures, connective tissue, and lymphatic vessels, and it is called distraction histiogenesis (Murray and Fitch 1996; Swennen et al. 2002; Wiltfang et al. 2002).
Periods of Distraction Osteogenesis
Distraction osteogenesis procedure consists of four sequential stages: (a) Osteotomy, (b) Latency, (c) Distraction, and (d) Consolidation (Cope and Samchukov 2005; Ilizarov 1990).
Osteotomy
This is the first stage of distraction osteogenesis in which the relevant bone area is osteotomized into two segments similar to a fracture line. This intervention triggers the healing process of the bone. Distraction osteogenesis helps to guide the healing process to regenerate a new bone in the desired direction. The healing process is similar to the fracture-healing process and consists of three main periods after the impaction: (1) inflammation, (2) callus formation, and (3) remodeling (McKibbin 1978). During the inflammation process, proliferative cells start to fill the fractured area. Then, the organization of the fracture hematoma starts to take place. Following this process, callus formation starts.
Latency
Latency period is the first period which represents the time allowed for callus formation. During this period, soft callus forms around and between the osteotomized bone segments, which contain inflammatory cells, fibroblasts, collagen, invading capillaries, and cells with osteogenic potential. This stage usually takes 5–7 days’ time (Ilizarov 1989b, 1990; Ilizarov et al. 1978b). Following this stage, granulation and loose connective tissue convert gradually to fibrous and cartilaginous tissues, which continue for about 3 weeks. In normal healing period, soft callus formation is followed by hard callus formation in which the fibrous and cartilaginous tissues are converted to woven bone by osteoblasts. This stage is continued by lamellar bone formation and gradual reconstitution of medullary canal. However, in distraction osteogenesis, this stage is consciously interrupted by the clinician to apply gradual traction to the bone segments after the soft callus is formed (Fig. 4.1).


Fig. 4.1
Soft callus and distraction stages seen on the mandible (Illustrated by Dr. Ali Murat Kökat)
There are some controversial studies on animals, which report that latency period may not be required before distraction procedure. However, there is no such evidence or study that represents the effect of latency period on humans. Latency period is still accepted as a crucial stage for the distraction osteogenesis procedure.
Distraction
The conscious interruption of callus formation and application of gradual traction is called the distraction stage. Mechanical stimulation during the distraction stage is believed to facilitate bone regeneration in the distraction gap. At the beginning of the distraction, the soft callus in between the two bone segments is elongated. Active distraction creates pressure, fluid flow, tensile strain, and tissue dilatation within and around the distraction area (Loboa et al. 2004, 2005). This stimuli influence the proliferation and differentiation of the multipotent mesenchymal cells. In the 2nd week, following the distraction, primary bone trabeculae begin to form. At the end of the 2nd week, mineralization starts at the surface of the bone segments and progresses to the center of the distraction gap. Slow stretching during the distraction osteogenesis is believed to prevent the formation of fibrotic tissue to fill the gap. The rate of distraction may affect the rate of bone formation and differentiation of the osteoprogenitor cells. A slow rate may cause early consolidation, whereas a high rate of distraction may cause a fibrous union of bone segments. Distraction rate of 1 mm/day in two to four equal increments is accepted as the ideal rate for clinically successful bone regeneration.
Consolidation
Consolidation is the last period, where the distractors are kept on the region to let the newly formed bone to mature. Following the end of the distraction period, bone trabeculae continue to grow at the center of the regenerate, toward each other until they fuse. The distraction gap ossifies gradually, and a bone bridge fills the gap. During the maturation of the regenerate, primary trabecular zone is resorbed completely. Typically, the consolidation stage involves twice as long as the time required for activation (Yu et al. 2004).
Effect of Distraction Osteogenesis on Soft Tissues
Distraction osteogenesis affects not only the involved bones, but also the soft tissues that surround them. During the distraction period, callus elongation and formation of new bone continue, and soft tissue elongation takes place as well. Growth changes and development occur in the muscles, vascular structures, nerves, connective tissues, and lymphatic vessels (Ilizarov 1989a).
Muscles
In muscle cells, not only cellular hypertrophy but also hyperplasia occurs (Guerrissi et al. 1994). Previously, the main belief was that the elongation of muscular tissue was caused by an increase in the length of sarcomeres. It is now accepted that the lengthening of the striated muscles is because of the given active adaptive response known as distraction histiogenesis (Pap et al. 2009). During distraction, the muscles lengthen throughout the entire muscle, not only at the level of osteotomy (Nakamura and Matsushita 1997).
Nerves
Nerves elongate by distraction of the bone too. Macroscopically, Ikeda et al. reported the consistency between the femural lengthening of the bone and the nerve in the ratio of, and it was also reported that at 0.8 mm/day, the rate of distraction was safe and did not cause any electrophysiological abnormality (Ikeda et al. 2000). In the maxillofacial region, however, if the application of the distraction osteogenesis procedure is onto the mandibular area because the inferior alveolar nerve is located inside a bony canal, the risk of nerve damage during the osteotomy or fixation of the pins is greater. Therefore, the osteotomies and the pin fixation should be carefully carried out.
Oral Structures
Gingiva responds favorably to gradual stretching during distraction histiogenesis. Initially, mild inflammation is observed during distraction (Fig. 4.2). However, after the first few weeks of consolidation, regenerative changes with neohistiogenesis are observed, by which the structural and functional integrity is restored (Kunimori et al. 2007; Cope and Samchukov 2005).


Fig. 4.2
Gingival inflammation occur on the newly formed area due to rapid tooth movement
The reaction of the periodontal ligament changes due to the design of the distraction device. If the device is bone-borne, then the load on the periodontal ligament decreases. If the device is a tooth-borne device, then the periodontal ligament around the involved teeth reacts as in orthodontic loads. Around the involved teeth, tension and compression sites cause bone remodeling (Liou and Huang 1998; Cope and Samchukov 2005). Therefore, the gap between the teeth may be more than the regenerate constituted between the bone segments. This can be explained by the tipping and orthodontic movement of the teeth.
Distraction Osteogenesis in the Craniofacial Region
The application of this technique has become a treatment, alternative to conventional orthognathic surgery, after McCarthy et al. introduced it to the craniofacial region (McCarthy et al. 1992). It was based on the technique that Gavril Ilizarov used for lengthening the extremities 1 mm/day (Ilizarov et al. 1978a; b).
One of the first applications of this technique on the cleft patients with maxillary hypoplasia was by Molina (Molina et al. 1998). Some of the cleft lip and palate patients may show severe maxillary deficiency at the adolescence and adult stages of growth. The main treatment approach in these cases was one-step advancement of the maxilla with Le Fort I osteotomy. However, one-step advancement has major disadvantages: soft tissue restriction may contribute to high relapse rates, and increased velopharyngeal insufficiency may also be seen. After Molina applied the technique to cleft patients with maxillary hypoplasia, the treatment approach started to change. However, even though distraction osteogenesis has shown to be effective in lengthening the membranous bone, including the maxilla, in the growing facial skeleton and in the adult patients, and even though a group of cleft patients benefit from the gradual advancement of the maxilla (Kumar et al. 2006), some difficulties with this technique still exist. Distraction osteogenesis may require multiple stages, and good occlusion may be more difficult to achieve. Another issue is that it is ineffective in reducing the oronasal fistula in cleft patients. The major shortcoming in bone grafting of the cleft area of cleft lip and palate patients is the difficulty in achieving complete soft tissue coverage, especially in cases with large defects. Therefore, buccal flaps or tongue flaps are used mostly for this purpose. Alveolar grafting is also performed to have a continuous alveolar bridge on the defective region. However, in large defects, these methods may be inefficient in repairing the fistula.
Alveolar distraction may be a more promising method to overcome such problems (Liou et al. 2000; Suzuki et al. 2006; Zemann and Pichelmayer 2011; Moore et al. 2011). In this chapter, a new method and an appliance with a vector control developed to treat cases with large defects by means of distraction osteogenesis will be presented.
Archwise Distraction Appliance
As mentioned above, conventional techniques have some shortcomings. To overcome these, an appliance involving a distractor was fabricated and named Archwise Distraction Appliance (AWDA).
Fabrication of the Appliance
The appliance consists of three parts: chromium–cobalt crowns, parallel stainless steel archwires, and archwise distractors.
Chromium Cobalt Crowns
Chromium cobalt crowns form the major part of the appliance. The crowns are fabricated on the unprepared teeth, right after the orthodontic treatment is finalized. Technical part of the crown preparation involves three stages:
1.
Blockout of the undercuts
2.
Wax modeling
3.
Casting stage, similar to the prosthetic metal abutment preparation stages of veneer crowns.
In the newer version, however, the facial facets of the anterior crowns will be made up of composite for esthetic reasons. Another issue that has to be considered is the drainage holes that have to be prepared occlusally to serve both as escape holes for the bonding agent and as areas that reduce the resistance of the crown to ease the removal.
The crowns also contain accessories which the guiding wires pass through: (1) double tubes and (2) semicircular tubes.
Double Tubes
This accessory consists of two connected tubes placed on top of each other on the crowns, which will serve as the anchoring unit of the appliance. Their main function is to house the guiding wires on which the distractors are placed. Their inner diameter is 2 mm (Fig. 4.3).


Fig. 4.3
Tube shape and diameter on the metal-casted appliance
The mesial border of the double tubes should end, close to the mesial edge of the anchoring teeth. This way, enough space, distal to the tubes, remains to provide space for the extensions of the guiding wires, which also helps the patient to avoid any impingement of the wires on the cheek mucosa. The size of the distal extension should be determined according to the planned sagittal movement of the anterior segments, with extra 5 mm dead wire part for cinching back to act as stops (Fig. 4.4).
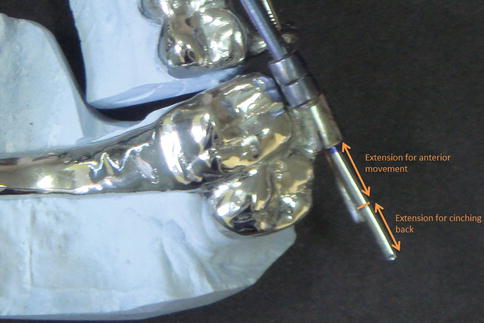
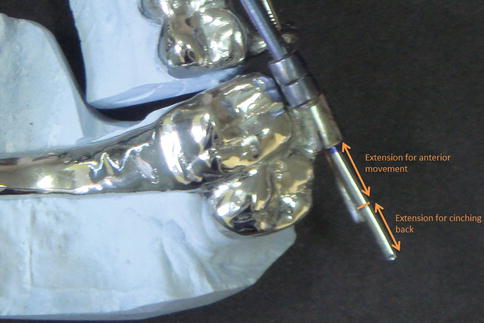
Fig. 4.4
Planned wire extension
Semicircular Tubes
These are the other accessories, which are placed in the interproximal areas in the distraction disk units. The diameters of these semicircular tubes are similar to that of the double tubes (Fig. 4.5).


Fig. 4.5
Semicircular tube shape and diameter on the metal-casted appliance
The distance between the mesial edge of the double tube and the first semitube of the distraction unit must be 1 mm longer than the width of the distractor to ease the insertion.
Palatal Bar
It is placed to reinforce the anchorage by connecting the molar teeth transpalatally to each other. In the cleft palate cases with hard palate defect, the anchorage unit must be reinforced with a palatal bar, since there is no bone bridge on the palatal vault.
Impressions and Wax Modeling
Two-step impression is taken with polyvinyl siloxane material for accuracy. Following the stone model acquisition, appliance design is traced on the model. Anchorage and distraction units are marked clearly, and the areas where the tubes and semitubes will be constructed are shown precisely.
The wax model is returned to the clinician for the last control of every part of the appliance. Any necessary changes and additional constructions are marked on the model, and the model is returned back to the laboratory. The most important thing to be controlled at this stage is the horizontal orientation of the tubes and the semitubes. They all have to be positioned on the same plane (Fig. 4.6).
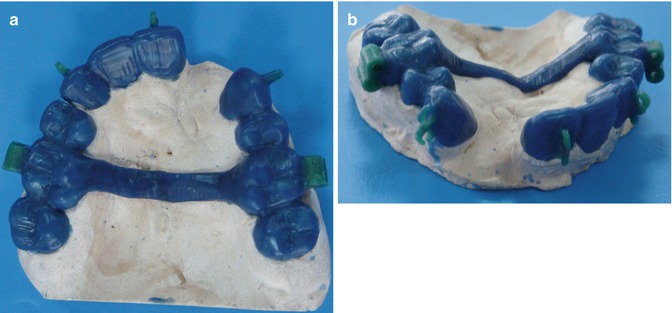
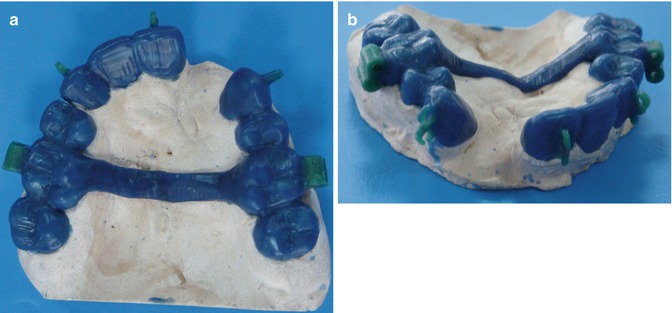
Fig. 4.6
(a) Occlusal view of wax-up model for clinician control. (b) Oblique view of the wax-up model
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


