Signs and Symptoms of Temporomandibular Disorders
“YOU CAN NEVER DIAGNOSE SOMETHING YOU HAVE NEVER HEARD ABOUT.”
—JPO
In the previous chapter certain events and conditions were described that can lead to alteration of the normal function of the masticatory system. Etiologic factors such as trauma, emotional stress, orthopedic instability, sources of deep pain, and muscle hyperactivity were implicated as significant components. In this chapter the common signs and symptoms of masticatory dysfunction are discussed. The clinical signs and symptoms of masticatory dysfunction can be grouped into categories according to structures that are affected: (1) the muscles, (2) the temporomandibular joints (TMJs), and (3) the dentition. Muscle and TMJ disorders make up the group of conditions known as temporomandibular disorders (TMDs).1 Included with the signs and symptoms of each are the etiologic factors that either cause or contribute to the disorder.
In evaluating a patient it is important to identify both signs and symptoms clearly. A sign is an objective clinical finding that the clinician uncovers during a clinical examination. A symptom is a description or complaint reported by the patient. Patients are acutely aware of their symptoms, yet they may not be aware of their clinical signs. For example, a person reports muscle tenderness during mandibular opening yet is totally unaware of the joint sounds that are also present. Both the muscle tenderness and the joint sounds are clinical signs, but only the muscle tenderness is considered a symptom. To avoid overlooking subclinical signs, the examiner must be acutely aware of the common signs and symptoms for each of the specific disorders.
Functional Disorders of the Muscles
Functional disorders of masticatory muscles are probably the most common TMD complaints of patients seeking treatment in the dental office.2,3 With regard to pain, they are second only to odontalgia (i.e., tooth or periodontal pain) in terms of frequency. They are generally grouped in a large category known as masticatory muscle disorders.4 As with any disorder, there are two major symptoms that can be observed: pain and dysfunction.
Pain
Certainly the most common complaint of patients with masticatory muscle disorders is muscle pain, which may range from slight tenderness to extreme discomfort. Pain felt in muscle tissue is called myalgia, which can arise from increased levels of muscular use. The symptoms are often associated with a feeling of muscle fatigue and tightness. Although the exact origin of this type of muscle pain is debated, some authors suggest it is related to vasoconstriction of the relevant nutrient arteries and the accumulation of metabolic waste products in the muscle tissues. Within the ischemic area of the muscle certain algogenic substances (e.g., bradykinins, prostaglandins) are released, causing muscle pain.4–9
Muscle pain, however, is far more complex than simple overuse and fatigue. In fact, the muscle pain associated with most TMDs does not seem to be strongly correlated with increased activity such as spasm.10–14 It is now appreciated that muscle pain can be greatly influenced by central mechanisms,6,15,16 as discussed later in this chapter.
The severity of muscle pain is directly related to the functional activity of the muscle involved. Therefore patients often report that the pain affects their functional activity. When a patient reports pain during chewing or speaking, these functional activities are not usually the cause of the disorder. Instead, they heighten the patient’s awareness of it. More likely some type of activity or central nervous system (CNS) effect has led to the muscle pain, and thus treatment directed toward the functional activity will not be appropriate or successful; rather, treatment must be directed towards diminishing the CNS effects or possibly muscle hyperactivity.
It must also be remembered that myogenous pain (pain originating in muscle tissue) is a type of deep pain and, if it becomes constant, can produce central excitatory effects. As described in Chapter 2, these effects may present as sensory effects (i.e., referred pain or secondary hyperalgesia) or efferent effects (i.e., muscle effects), or even autonomic effects. In particular, muscle pain can reinitiate more muscle pain (i.e., the cyclic effect discussed in Chapter 2). This clinical phenomenon was first described17 in 1942 as cyclic muscle spasm and later related to the masticatory muscles by Schwartz.18 More recently, with the findings that the painful muscles are not truly in spasm, the term cyclic muscle pain was coined for this text. The importance of cyclic muscle pain is discussed later in this chapter.
Another very common symptom associated with masticatory muscle pain is headache. Since there are numerous types of headaches, this symptom is discussed in a separate section later in this chapter.
Dysfunction
Dysfunction is a common clinical symptom associated with masticatory muscle disorders. Usually it is seen as a decrease in the range of mandibular movement. When muscle tissues have been compromised by overuse, any contraction or stretching increases the pain. Therefore to maintain comfort, the patient restricts movement within a range that does not increase the level of pain. Clinically this is seen as an inability to open the mouth widely. The restriction may be at any degree of opening depending on where discomfort is felt. In some myalgic disorders the patient can slowly open wider but the pain is still present and may even become worse.
Acute malocclusion is another type of dysfunction. The term acute malocclusion refers to any sudden change in the occlusal condition that has been caused by a disorder. An acute malocclusion may result from a sudden change in the resting length of a muscle that controls jaw position. When this occurs, the patient describes a change in the occlusal contact of the teeth. The mandibular position and resultant alteration in occlusal relationships depend on the muscles involved. For example, with slight functional shortening of the inferior lateral pterygoid, disocclusion of the posterior teeth will occur on the ipsilateral side and premature contact of the anterior teeth (especially the canines) on the contralateral side. With functional shortening of the elevator muscles (clinically a less detectable acute malocclusion), the patient will generally complain of an inability to occlude normally. It is important to remember that an acute malocclusion is the result of the muscle disorder and not the cause. Therefore treatment should never be directed toward correcting the malocclusion. Rather, it should be aimed at eliminating the muscle disorder. When this condition is reduced, the occlusal condition will return to normal. As discussed later, certain intracapsular disorders can also lead to acute malocclusion.
Many clinicians consider all masticatory muscle disorders to be the same. If this were the case, it would certainly make treatment considerations quite simple. However, experienced clinicians realize that this is not the case, since all muscle pain disorders do not successfully respond to the same treatment. Thus the experienced clinician realizes that all masticatory muscle disorders are not clinically the same. There are at least five different types, and being able to distinguish among them is important because the treatment of each is quite different. The five types are protective co-contraction (muscle splinting), local muscle soreness, myofascial (trigger point) pain, myospasm, and chronic centrally mediated myalgia. A sixth condition known as fibromyalgia must also be discussed. The first three conditions (protective co-contraction, local muscle soreness, and myofascial pain) are commonly seen in the dental office. Myospasm and chronic centrally mediated myalgia are less frequently seen. Many of these muscle disorders occur and resolve in a relatively short time. When these conditions are not resolved, more chronic pain disorders may result. Chronic masticatory muscle disorders become more complicated and treatment is generally oriented differently than for acute problems. It therefore becomes important that the clinician be able to identify acute muscle disorders from chronic disorders so that proper therapy can be applied. Fibromyalgia is a chronic myalgic disorder; it presents as a systemic musculoskeletal pain problem that needs to be recognized by the dentist and is best managed by referral to appropriate medical personnel.
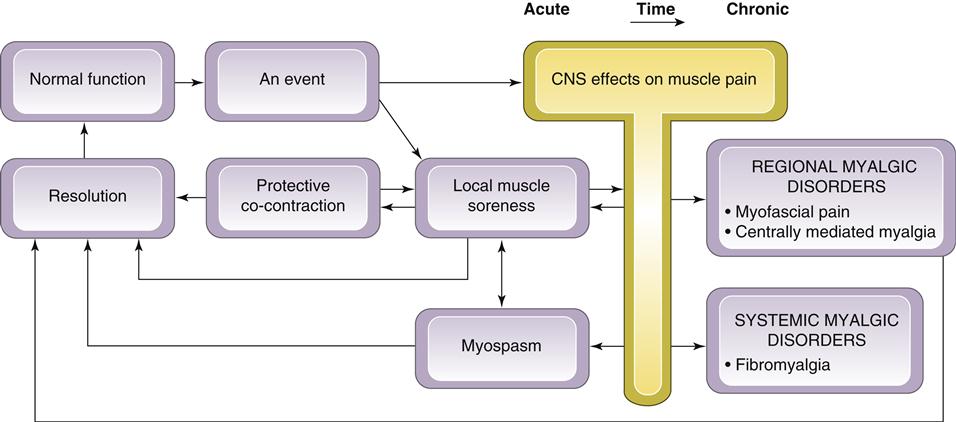
A Clinical Model of Masticatory Muscle Pain
To clarify the relationship between different muscle pain disorders, a model of masticatory muscle pain is presented in Figure 8-1. This model begins with the assumption that the muscles of mastication are healthy and functioning normally (as depicted in Chapter 2). Normal muscle function can be interrupted by certain types of events. If an event is significant, a muscle response known as protective co-contraction (muscle splinting) occurs. In many instances the consequence of the event is minor and co-contraction quickly resolves, allowing muscle function to return to normal. If, however, protective co-contraction is prolonged, local biochemical and later structural changes can occur, causing local muscle soreness. This condition may resolve spontaneously with rest or may require treatment.
If local muscle soreness does not resolve, changes in the muscle tissues may develop, resulting in prolonged pain input. This constant deep pain input can affect the CNS, leading to certain muscle responses (Chapter 2). Two examples of CNS-influenced muscle pain disorders are myofascial pain and myospasm. In some instances the CNS responds to certain events or local conditions by inducing an involuntary contraction seen clinically as a muscle spasm. Myospasms are not chronic but instead represent a condition of relatively short duration. At one time myospasm was thought to be the primary condition responsible for myalgia. However most of the present studies13,14,19–21 suggest that true myospasms are not common in patients suffering from masticatory muscle pain.
These masticatory muscle disorders usually present as relatively acute problems; once they are identified and treated, the muscle returns to normal function.22 If, however, these acute myalgic disorders are not recognized or appropriately managed, certain perpetuating conditions can advance the problem into a more chronic myalgic disorder. As the myalgic disorder becomes more chronic, the CNS contributes more to maintaining the condition. Because the CNS is an important factor in this condition, it is referred to as centrally mediated myalgia. Chronic centrally mediated myalgia is often very difficult to resolve and treatment strategies other than those used with the acute myalgic disorders must be employed.
Another example of a chronic musculoskeletal pain disorder is fibromyalgia. Although this is not primarily a masticatory pain disorder, the dentist must recognize this condition so as to avoid unnecessary dental therapy. Unlike the other muscle pain disorders, which are regional, fibromyalgia is a widespread global musculoskeletal pain condition. The dentist must be aware that the management or these chronic pain disorders is quite different from that employed with the relatively acute muscle disorders.
To better describe this clinical model of masticatory muscle pain, each component of the model is discussed in detail below.
An Event
Normal muscle function can be interrupted by various types of events. These can arise from either local or systemic factors. Local factors represent any events that acutely alter sensory or proprioceptive input in the masticatory structures—for example, the fracture of a tooth or the placement of a restoration in supraocclusion. Trauma to local structures, such as tissue damage caused by a dental injection, represents another type of local event. Trauma can also arise from excessive or unaccustomed use of masticatory structures, such as chewing unusually hard food or chewing for a long time (i.e., gum chewing). Opening too wide may produce a strain to ligaments supporting the joint and/or muscles. This may occur as a result of a long dental procedure or even by simply opening too wide (i.e., yawning).
Any source of constant deep pain input may also represent a local factor that alters muscle function. Such pain may have its source in local structures such as the teeth, joints, or even the muscles themselves. The source of the pain, however, is not significant, since any constant deep pain, even idiopathic pain, can create a muscle response.23
Systemic factors may also represent events that can interrupt normal muscle function. One of the most commonly recognized systemic factors is emotional stress.3,24–26 Stress seems to alter muscle function through either the gamma efferent system to the muscle spindle or by means of sympathetic activity to the muscle tissues and related structures.27–31 Of course responses to emotional stress are quite individualized. Therefore the patient’s emotional reaction and psychophysiologic response to stressors may vary greatly. It has been demonstrated that exposure to an experimental stressor can immediately increase the resting electromyographic (EMG) activity of the subject’s masticatory muscles. This physiologic response provides direct insight to how emotional stress directly influences muscle activity and muscle pain.
Other systemic factors can influence muscle function and are less understood, such as acute illness or viral infections. Likewise, there is a broad category of poorly understood constitutional factors that are unique to each patient. Such factors include immunologic resistance and autonomic balance. These seem to reduce the individual’s ability to resist or combat the challenges or demands arising from a stressful event. Constitutional factors are likely to be influenced by age, gender, diet, and perhaps even genetic predisposition. These factors, discussed in Chapter 7, influence the patient’s adaptability. Clinicians realize that individual patients often respond quite differently to similar events. It is assumed, therefore, that certain constitutional factors do exist and can influence the individual’s response. At this time these factors are poorly understood and not well defined as they relate to muscle pain disorders.
Protective Co-contraction (Muscle Splinting)
The first response of the masticatory muscles to one of the previously described events is protective co-contraction, which is a normal CNS response to injury or threat of injury. It has also been called protective muscle splinting.32 In the presence of an injury or threat of injury, the normal sequencing of muscle activity is altered so as to protect the threatened part from further injury.3–37 Protective co-contraction can be likened to the co-contraction38 observed during many normal functional activities, such as bracing the arm in attempting to complete a task with the fingers. In the presence of altered sensory input or pain, antagonistic muscle groups fire during movement in an attempt to protect the injured part. For example, a patient experiencing co-contraction in the masticatory system will demonstrate increased muscle activity of the elevator muscles during mouth opening.33,39,40 During closing of the mouth, increased activity is noted in the depressing muscles. This coactivation of antagonistic muscles is considered a normal protective or guarding mechanism and should be recognized as such by the clinician. Protective co-contraction is not a pathologic condition, although it can lead to muscle symptoms when it is prolonged.
The etiology of protective co-contraction can be any sudden change in sensory or proprioceptive input from associated structures. An example of such an event in the masticatory system is the placement of a high crown. Protective co-contraction can also be caused by any source of deep pain input or an increase in emotional stress.
Protective co-contraction is reported clinically as a feeling of muscle weakness directly following some event. There is no pain reported when the muscle is at rest, but use of the muscle will typically result in increased pain. The patient often presents with limited mouth opening, but when he or she is asked to open slowly, full opening can be achieved. The key to identifying protective co-contraction is that it immediately follows an event; therefore the history is very important. If protective co-contraction continues for several hours or days, the muscle tissue can become compromised and a local muscle problem may develop.
Local Muscle Soreness (Noninflammatory Myalgia)
Local muscle soreness is a primary noninflammatory myogenous pain disorder. It is often the first response of the muscle tissue to prolonged co-contraction and is the most common type of acute muscle pain seen in dental practice. Whereas co-contraction represents a CNS-induced muscle response, local muscle soreness represents a condition characterized by changes in the local environment of the muscle tissues. These changes involve the release of certain algogenic substances (i.e., bradykinin, substance P, even histamine41) that produce pain. Initially these changes may represent nothing more than fatigue. Along with protracted co-contraction, other causes of local muscle soreness are local trauma or excessive use of the muscle. When excessive use is the etiology, a delay in the onset of muscle soreness can occur.42 This type of local muscle soreness is often referred to as delayed onset muscle soreness or post-exercise muscle soreness.43–47
Since local muscle soreness itself is a source of deep pain, an important clinical event can occur. Deep pain produced by muscle soreness can, in fact, produce protective co-contraction. This additional co-contraction can, in turn, produce more muscle soreness. Therefore a cycle can be created (cyclic muscle pain) whereby muscle soreness produces more co-contraction and so on, as discussed in earlier chapters.
The clinician must be aware of the complications this might pose in arriving at a diagnosis. For example, if the medial pterygoid muscle were injured by an inferior alveolar nerve block, the trauma would cause local muscle soreness. The pain associated with the soreness, in turn, would produce protective co-contraction. Since protective co-contraction can lead to muscle soreness, a cycle would be set into motion. During this cycling, the original tissue damage produced by the injection would resolve. When tissue repair was complete, the original source of pain would have been eliminated; however, the patient might continue to suffer with a cyclic muscle pain disorder. Since the original cause of the pain would no longer be part of the clinical picture, the clinician might easily be confused during the examination. The clinician must therefore recognize that although the original cause has resolved, a cyclic muscle pain condition exists and must be treated. This condition is an extremely common clinical finding and, if not recognized, can lead to mismanagement of the patient.
Local muscle soreness presents clinically with muscles that are tender to palpation and reveal increased pain with function. Structural dysfunction is common, and when the elevator muscles are involved, limited mouth opening results. Unlike the case in protective co-contraction, the patient has great difficulty opening the mouth any wider. With local muscle soreness there is an actual muscle weakness.48–50 Muscle strength returns to normal when the muscle soreness has resolved.49–51
Central Nervous System Effects on Muscle Pain
The muscle pain conditions described to this point are relatively simple, having their origins predominantly in the local muscle tissues. Therefore these conditions can be managed successfully by treatment of the local structures (muscles, joints, or teeth). Unfortunately muscle pain can become much more complex. In many instances, activity within the CNS can either influence or actually be the origin of the muscle pain. This may occur either secondary to ongoing deep pain input or altered sensory input, or it may arise from central influences such as upregulation of the autonomic nervous system (i.e., emotional stress). This occurs when conditions within the CNS excite peripheral sensory neurons (primary afferents), creating the antidromic release of algogenic substances into the peripheral tissues and resulting in muscle pain (i.e., neurogenic inflammation).16,52–54 These central excitatory effects can also lead to motor effects (primary efferents) resulting in an increase in muscle tonicity (co-contraction).14,55
Therapeutically, it is important for the clinician to appreciate that the muscle pain now has a central origin. The CNS responds in this manner secondary to either (a) the presence of ongoing deep pain input, (b) increased levels of emotional stress (i.e., an upregulation of the autonomic nervous system), or (c) changes in the descending inhibitory system, which lead to a decrease in the ability to counter the afferent input, whether nociceptive or not.
Centrally influenced muscle pain disorders are therapeutically divided into acute myalgic disorders, such as myospasm, and chronic myalgic disorders, which are further divided into regional myalgic disorders and systemic myalgic disorders. Regional myalgic disorders are subdivided into myofascial pain and chronic centrally mediated myalgia. An example of a systemic myalgic disorder is fibromyalgia. Each of these conditions is discussed below.
Myospasm (Tonic Contraction Myalgia)
Myospasm is a CNS-induced tonic muscle contraction. For many years the dental profession felt that myospasms were the most common source of myogenous pain. More recent studies, however, have shed new light on muscle pain and myospasms.
It is reasonable to expect that a muscle in spasm or tonic contraction would reveal a relatively high level of EMG activity. Studies, however, do not support the assumption that painful muscles have a significant increase in their EMG output.10,14,19,34,55 These studies have forced us to rethink the classification of muscle pain and to differentiate myospasms from other muscle pain disorders. Although myospasms of the muscles of mastication do occur, this condition is not common; when present, it is usually easily identified by its clinical characteristics.
The etiology of myospasms has not been well documented. Several factors are likely to combine to promote myospasms. Local muscle conditions certainly seem to foster myospasms. These conditions involve muscle fatigue and changes in local electrolyte balances. Deep pain input may also precipitate myospasms.
Myospasms are easily recognized by the structural dysfunction they produce. Since a muscle in spasm is fully contracted, major positional changes result in the jaw according to the muscle or muscles in spasm. These changes create certain acute malocclusions to be discussed in detail in later chapters. Myospasms are also characterized by very firm muscles as noted by palpation.
Myospasms are usually short-lived, lasting for only minutes at a time. Such a spasm is similar to an acute cramp in a leg muscle. On occasion these uncontrolled muscle contractions can be repeated over time. When they are repeated, the condition may be classified as a dystonia. Dystonic conditions are thought to be related to CNS mechanisms and must be managed differently than simple myospasms. There are certain well-described oromandibular dystonias that predominantly affect the muscles of mastication. During these dystonic episodes the mouth may be forced open (opening dystonia) or closed (closing dystonia) or even off to one side. The precise jaw position is determined by the muscles involved.
Regional Myalgic Disorders
Myofascial pain (trigger-point myalgia)
Myofascial pain is a regional myogenous pain condition characterized by local areas of firm, hypersensitive bands of muscle tissue known as trigger points. This condition is sometimes referred to as myofascial trigger-point pain. It is a type of muscle disorder that is not widely appreciated or completely understood, yet it commonly occurs in patients with myalgic complaints. In one study56 more than 50% of the patients reporting to a university pain center were diagnosed as having this type of pain.
Myofascial pain was first described by Travell and Rinzler57 in 1952, yet the dental and medical communities were slow to appreciate its significance. In 1969, Laskin58 described the myofascial pain dysfunction (MPD) syndrome as having certain clinical characteristics. Although he borrowed the term myofascial, he was not describing myofascial trigger-point pain. Instead, MPD syndrome has been used in dentistry as a general term to denote any muscle disorder (not an intracapsular disorder). Since the term is so broad and general, it is not useful in the specific diagnosis and management of masticatory muscle disorders. MPD syndrome should not be confused with Travell and Rinzler’s description, which is used in this textbook. The term myofascial pain was further misused when the Research Diagnostic Criteria (RDCs) were first established in 1992.59 The RDCs referred to all muscle pain disorders and not necessarily muscle pain characterized by trigger points. If one is referring to all types of muscle pain, the term masticatory muscle pain should be used as a broad generic term. Myofascial pain should be used only if the condition meets the original description in the medical literature (discussed in the following section).
Myofascial pain arises from hypersensitive areas in muscles called trigger points. These very localized areas in muscle tissues and/or their tendinous attachments are often felt as taut bands on palpation, which elicits pain. The exact nature of a trigger point is not known. It has been suggested60–62 that certain nerve endings in the muscle tissues may become sensitized by algogenic substances that create a localized zone of hypersensitivity.63 There may be a local temperature rise at the site of the trigger point, suggesting an increase in metabolic demand and/or reduction of blood flow to these tissues.64,65 A trigger point is a very circumscribed region in which just a relatively few motor units seem to be contracting.66 If all the motor units of a muscle contract, the muscle will of course shorten (Chapter 2). This condition is called myospasm and has already been discussed above. Since a trigger point has only a select group of motor units contracting, no overall shortening of the muscle results, as occurs with myospasm.
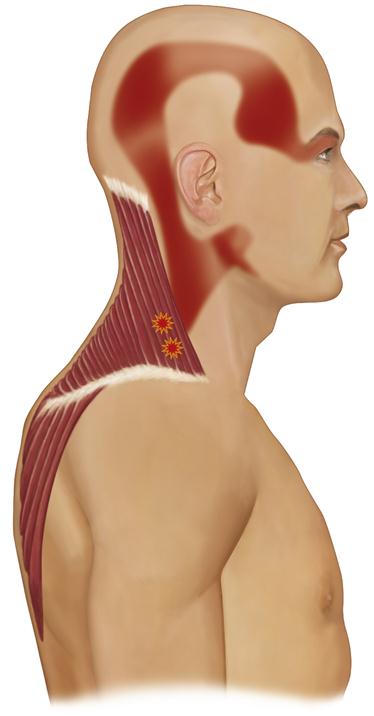
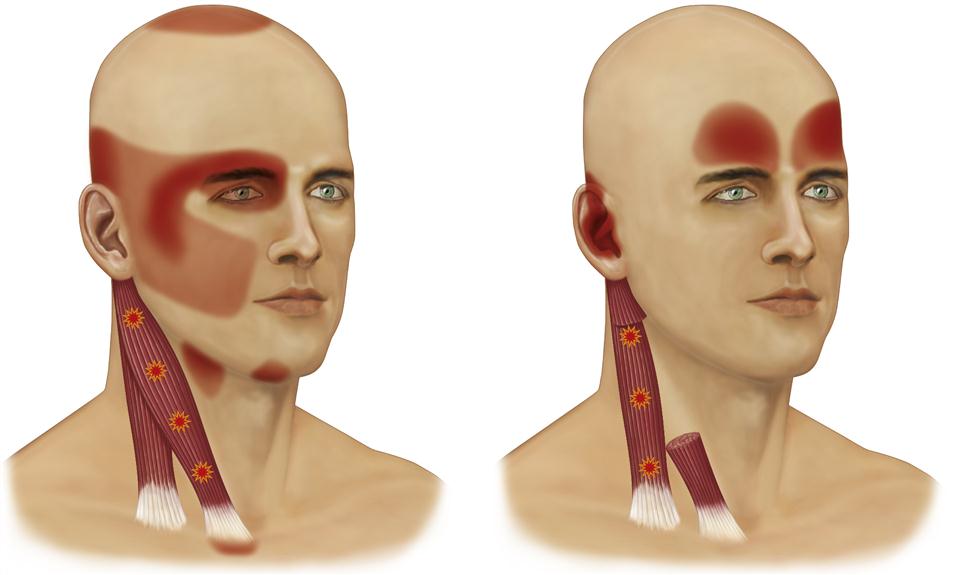
The unique characteristic of trigger points is that they are a source of constant deep pain and therefore can produce central excitatory effects (Chapter 2). If a trigger point centrally excites a group of converging afferent interneurons, referred pain will often result, generally in a predictable pattern according to the location of the involved trigger point (Figures 8-2 to 8-4).67 This is often reported by the patient as headache pain.
The etiology of myofascial pain is complex. Unfortunately we lack a complete understanding of this myogenous pain condition. It is therefore difficult to be specific concerning all etiologic factors. Travell and Simons have described certain local and systemic factors that seem to be associated, such as trauma, hypovitamintosis, poor physical conditioning, fatigue, and viral infection.68 Other important factors are likely to be emotional stress and deep pain input.
The most common clinical feature of myofascial pain is the presence of local areas of firm, hypersensitive bands of muscle tissue called trigger points. Although the palpation of trigger points produces pain, local muscle sensitivity is not the most common complaint of patients suffering from myofascial trigger-point pain. The most common symptom is usually associated with the central excitatory effects created by the trigger points. In many instances patients may be aware only of the referred pain and not even acknowledge the trigger points. A perfect example is the patient suffering from myofascial trigger-point pain in the trapezius muscle, which creates referred pain to the temple region (see Figure 8-3).67,69,70,76 The chief complaint is temporal headache, with very little acknowledgment of the trigger point in the shoulder. This clinical presentation can easily distract the clinician from the source of the problem. The patient will draw the clinician’s attention to the site of the pain (the temporal headache) and not the source. The clinician must always remember that for treatment to be effective, it must be directed toward the source of the pain, not the site. Therefore it is always important to search for the true source of the pain.
Since trigger points can create central excitatory effects,71–74 it is also important to be aware of all the possible clinical manifestations. As stated in Chapter 2, central excitatory effects can appear as referred pain, secondary hyperalgesia, protective co-contraction, or even autonomic responses. These conditions must be considered in evaluating the patient.
An interesting clinical feature of a trigger point is that it may present in either an active or a latent state. In the active state it produces central excitatory effects. Therefore when a trigger point is active, a headache is commonly felt. Since referred pain is wholly dependent on its original source, palpation of an active trigger point (local provocation) often increases the headache. Although this characteristic is not always present, when it is, it is an extremely helpful diagnostic aid. In the latent state a trigger point is no longer sensitive to palpation and therefore does not produce referred pain. When trigger points are latent, they cannot be found by palpation and the patient does not complain of headache pain. In this case the history offers the only data that can lead the clinician to the diagnosis of myofascial pain. In some instances the clinician should consider asking the patient to return to the office when the headache is present so that confirmation of the pattern of pain referral can be verified and the diagnosis confirmed.
It is thought that trigger points do not resolve without treatment. They may, in fact, become latent or dormant, leading to temporary relief of the referred pain. Trigger points may be activated by various factors75 such as increased use of a muscle, strain on the muscle, emotional stress, or even an upper respiratory infection. When trigger points are activated, the headache returns. This is a common finding with patients who complain of regular late-afternoon headaches following very trying and stressful days.
Along with referred pain, other central excitatory effects may be felt. When secondary hyperalgesia is present, it is commonly felt as an increased sensitivity to touching on the scalp. Some patients will even report that their “hair hurts” or that it is painful to brush their hair. Co-contraction is another common condition associated with myofascial pain. Trigger points in the shoulder or cervical muscles can produce co-contraction in the muscles of mastication.55 If this continues, local muscle soreness in the masticatory muscles can develop. Treatment of the masticatory muscles will not resolve the condition because its source is the trigger points of the cervicospinal and shoulder muscles. However, treatment of the trigger points in the shoulder muscles will resolve the masticatory muscle disorder since it is the primary source of the pain. Management may become difficult when muscle soreness has been present for a long time, because that can initiate cyclic muscle pain (Chapter 2). In these cases extending treatment to both the muscles of mastication and the trigger points in the cervicospinal and shoulder muscles will usually resolve the problem.
On occasion, autonomic effects are produced by deep pain input from trigger points. These may result in such clinical findings as tearing or drying of the eye or vascular changes (e.g., blanching and/or reddening of tissue). Sometimes the conjunctiva will become red. There may even be mucosal changes that produce nasal discharge similar to an allergic response. The key to determining whether the autonomic effects are related to central excitatory effects or to a local reaction such as allergies is the unilateral appearance. Central excitatory effects in the trigeminal area rarely cross the midline. Therefore if the deep pain is unilateral, the autonomic effects will be on the same side as the pain. In other words, one eye will be red and the other normal, one nostril draining mucus and the other not. With allergic responses, both eyes or both nostrils will be involved.
By way of summary, the clinical symptoms reported with myofascial pain are most commonly associated with the central excitatory effects created by the trigger points and not the trigger points themselves. The clinician must be aware of this and find the involved trigger points. When these are palpated, they appear as hypersensitive areas often felt as taut bands within the muscle. There is usually no local pain when the muscle is at rest but some pain when the muscle is used. Often some slight structural dysfunction will be seen in the muscle harboring the trigger points. This is commonly reported as a “stiff neck.”
Considerations of Chronic Muscle Pain
The myalgic disorders described above are commonly seen in the general practice of dentistry and usually represent problems of short duration. With proper therapy, these disorders can be completely resolved. However, when myogenous pain persists, more chronic and often complex muscle pain disorders can develop. With chronicity, myogenous pain disorders become even more influenced by the CNS, resulting in a more regional or even occasionally global pain condition. Often cyclic muscle pain also becomes an important feature that perpetuates the condition.
As a general rule chronic pain is considered to be pain that has been present for 6 months or longer. The duration of pain may not, however, be the most important factor in determining chronicity. Some pains are experienced for years that never become chronic pain conditions. Likewise, some pain conditions become clinically chronic in a matter of months. The additional factor that must be considered is the continuity of the pain. When a pain experience is constant, with no periods of relief, the clinical manifestations of chronicity develop quickly. On the other hand, if the pain is interrupted with periods of remission (no pain), the condition may never become a chronic pain disorder. For example, cluster headache is an extremely painful neurovascular pain condition that may last for years and never become a chronic pain disorder. The reason for this is that significant periods of relief occur between episodes of pain. Conversely, the constant pain associated with centrally mediated myalgia, when left untreated, can develop the clinical manifestations of chronicity within several months.
The dentist must recognize that as myalgic complaints progress from an acute to a chronic disorder, the effectiveness of local treatment is greatly reduced. Chronic pain disorders most often need be managed by a multidisciplinary approach. In many instances, the dentist alone is not equipped to manage these disorders. It is important, therefore, for the dentist to recognize chronic pain disorders and to consider referring such patients to a team of appropriate therapists who are better able to manage these conditions.
Perpetuating factors
There are certain conditions or factors that, when present, may prolong the muscle pain condition. These factors are known as perpetuating factors and can be divided into those with a local source and those with a systemic source.
Local perpetuating factors
The following conditions represent local factors that can be responsible for the progression of a relatively simple acute muscle disorder into a more complex chronic pain condition:
Systemic perpetuating factors
The following conditions represent systemic factors that can be responsible for the progression of an acute muscle disorder into a chronic pain condition:
2. Downregulation of the descending inhibitory system. As mentioned in Chapter 2, the descending inhibitory system represents a group of brainstem structures that regulate ascending neural activity. An effective descending inhibitory system minimizes nociceptive input as it ascends to the cortex. If this system becomes less efficient, increased nociception can reach the cortex, resulting in an experience of greater pain. It is unclear what factors lead to a downregulation of the system, but this concept may in part help to explain the marked differences in people’s responses to various events (patient adaptability). Perhaps factors such as nutritional deficiency and physical fitness play a role. Although a decrease in the function of the descending inhibitory system seems to fit the clinical presentation of continued pain problems, these factors have yet to be documented adequately.
3. Sleep disturbances. Sleep disturbances appear to be commonly associated with many chronic myalgic pain disorders.76–82 It is currently unknown whether the chronic pain condition produces a sleep disturbance or whether a sleep disturbance is a significant factor in the initiation of the chronic pain condition. Regardless of this cause-and-effect question, the relationship between sleep disturbances and chronic pain disorders must be recognized, since it may have to be addressed during therapy.
5. Secondary gain. Chronic pain disorders can produce certain secondary gains for the suffering patient.83–86 When a patient learns that chronic pain can serve to alter his or her normal life, the patient may have difficulty giving up the pain and going back to normal responsibilities. For example, if chronic pain becomes an excuse to avoid work, it will be difficult for the clinician to resolve the pain problem unless the patient wishes to return to work. It is important for the therapist to recognize the presence of secondary gains so that they can be properly addressed. Failure to eliminate secondary gains will lead to failure in resolving the chronic pain disorder.
6. Depression. Psychological depression is a common finding in chronic pain patients.87–95 It is well documented that patients who suffer for long periods of time will frequently become depressed.96–99 Since depression can result in an independent psychological problem, it must be properly addressed in order to manage the patient adequately.100,101 Elimination of the pain problem alone will not necessarily eliminate the depression.
Centrally mediated myalgia (chronic myositis)
Centrally mediated myalgia is a chronic, continuous muscle pain disorder originating predominantly from CNS effects that are felt peripherally in the muscle tissues. This disorder clinically presents with symptoms similar to those of an inflammatory condition of the muscle tissue and therefore is sometimes referred to as myositis. This condition, however, is not characterized by the classic clinical signs associated with inflammation (reddening, swelling, etc.); therefore myositis is not an accurate term for it. A more accurate term is neurogenic inflammation. We know now that when the CNS becomes exposed to prolonged nociceptive input, brainstem pathways can functionally change. This can result in an antidromic effect on afferent peripheral neurons. Inother words, neurons that normally only carry information from the periphery into the CNS can now be reversed to carry information from the CNS out to the peripheral tissues. This is likely to occur through the axon transport system.23 When this occurs, the afferent neurons in the periphery can release nociceptive neurotransmitters (e.g., substance P, bradykinin), which in turn causes peripheral tissue pain. This process is called neurogenic inflammation.102–106
The important concept to remember is that the muscle pain expressed by the patient with chronic centrally mediated myalgia cannot be treated by manipulating the painful muscle tissue itself. Management must be directed to the central mechanisms—a thought process that can be very foreign to dentists.
Chronic centrally mediated myalgia may be caused by the prolonged input of muscle pain associated with local muscle soreness or myofascial pain. In other words, the longer the patient complains of myogenous pain, the greater the likelihood of chronic centrally mediated myalgia. However, it is also possible that other central mechanisms may play a significant role in the etiology of centrally mediated myalgia, such as chronic upregulation of the autonomic nervous system, chronic exposure to emotional stress, or other sources of deep pain input.
It should be noted that chronic centrally mediated myalgia is more closely associated with continuity of muscle pain rather than actual duration. Many muscle pain disorders are episodic, leaving intermittent times of no muscle pain. Periodic episodes of muscle pain do not produce chronic centrally mediated myalgia. A prolonged and constant period of muscle pain, however, is likely to lead to chronic centrally mediated myalgia.
On occasion, a bacterial or viral infection can spread to a muscle, producing a true infectious myositis. For example, a traumatic penetrating injury to a muscle may result in a bacterial infection resulting in a true myositis. These conditions are not common, but when the history suggests trauma or a viral infection, proper treatment must be implemented.
A clinical characteristic of chronic centrally mediated myalgia is the presence of constant, aching myogenous pain. The pain is present during rest and increases with function. The muscles are very tender on palpation and structural dysfunction is common. The most common clinical feature is the extended duration of the symptoms.
Chronic systemic myalgic disorders (fibromyalgia)
Chronic systemic myalgic disorders must be recognized as such because therapy demands it. The word systemic is used because the symptoms are reported by the patient to be widespread or global and the etiology appears to be associated with a central mechanism. The treatment of these conditions becomes more complicated because perpetuating factors and cyclic muscle pain must also be addressed. A chronic systemic myalgic disorder that the dentist must be aware of is fibromyalgia. This is a global musculoskeletal pain disorder that can be confused with an acute masticatory muscle disorder. In the past fibromyalgia has been referred to in the medical literature as fibrositis. According to a major consensus report,107 fibromyalgia is a widespread musculoskeletal pain disorder in which tenderness is found in 11 or more of 18 specific tender-point sites throughout the body. More recently the criteria for fibromyalgia have come to include the Wide Spread Pain Index and the Symptom Severity Scale.108 It is important for the dentist to recognize that fibromyalgia is not a masticatory pain disorder yet that many patients with fibromyalgia often report complaints similar to those associated with TMD.109–114 This similarity of presentation may lead some fibromyalgia patients to be mistreated with TMD therapies.115 This occurs because 42% of patients with fibromyalgia also report TMD-like symptoms.115 Because several chronic systemic muscle pain conditions can coexist,116 there is a need to recognize this and to refer those patients who require nondental treatment to the appropriate medical personnel. Chronic systemic myalgic disorder is discussed more completely in Chapter 12, so that it may be properly identified and distinguished from a masticatory muscle disorder.
Functional Disorders of the Temporomandibular Joints
Functional disorders of the TMJs are probably the most common findings observed in examining a patient for masticatory dysfunction. These findings are due to the high prevalence of signs and not necessarily symptoms. Many of the signs, such as joint sounds, are not painful; therefore the patient may not seek treatment. When present, however, functional disorders generally fall into three broad categories: derangements of the condyle-disc complex, structural incompatibility of the articular surfaces, and inflammatory joint disorders. The first two categories have been collectively referred to as disc-interference disorders. The term disc-interference disorder was first introduced by Welden Bell117 to describe a category of functional disorders that arise from problems with the condyle-disc complex. Some of these problems are due to a derangement or alteration of the attachment of the disc to the condyle; others stem from an incompatibility between the articular surfaces of the condyle, disc, and fossa; still others are due to the fact that relatively normal structures have been extended beyond their normal range of movement. Although these broad categories have similar clinical presentations, they are treated quite differently. It is therefore important that they be clinically differentiated.
Inflammatory disorders arise from any localized response of the tissues associated with TMJ structures. These disorders are often the result of chronic or progressive disc derangement disorders. The two major symptoms of functional TMJ problems are pain and dysfunction.
Pain
Pain in any joint structure (including the TMJs) is called arthralgia. It would seem logical that such pain should originate from the articular surfaces when the joint is loaded by the muscles. This is impossible, however, in a healthy joint, since there is no innervation of the articular surfaces. Arthralgia can therefore originate only from nociceptors located in the soft tissues surrounding the joint.
Three periarticular tissues contain such nociceptors: the discal ligaments, capsular ligaments, and retrodiscal tissues. When these ligaments are elongated or the retrodiscal tissues compressed, the nociceptors send out signals and pain is perceived. The individual cannot differentiate between the three structures, so any nociceptors that are stimulated in any of these structures radiate signals perceived as joint pain. Stimulation of the nociceptors creates inhibitory action in the muscles that move the mandible. Therefore when pain is suddenly and unexpectedly felt, mandibular movement immediately ceases (nociceptive reflex). When chronic pain is felt, movement becomes limited and very deliberate (protective co-contraction).
Arthralgia from normal healthy structures of the joint is a sharp, sudden, intense pain closely associated with joint movement. When the joint is rested, the pain resolves quickly. If the joint structures break down, inflammation can produce a constant pain that is accentuated by joint movement. As discussed below, a breakdown of joint tissues results in a loss of normal articular surfaces, creating pain that can actually originate in the subarticular bone.
Dysfunction
Dysfunction is common with functional disorders of the TMJ. Usually it presents as a disruption of the normal condyle-disc movement, with the production of joint sounds.118–120 The joint sounds may be single events of short duration known as clicks. If such a click is loud, it may be referred to as a pop. Crepitation is a multiple, rough, gravel-like sound described as grating and complicated. Dysfunction of the TMJ may also present as catching sensations when the patient opens his or her mouth. Sometimes the jaw can actually lock. Dysfunction of the TMJ is always directly related to jaw movement.
The Continuum of Functional Disorders of the Temporomandibular Joint
As with muscle disorders, all functional disorders of the TMJ are not the same. Therefore proper identification of symptoms and the establishment of an accurate diagnosis are essential for successful treatment. Below, the three major categories of disorders of the TMJ are discussed, along with their various subcategories. The clinical presentation of each is identified and the more common etiologic factors are enumerated.
Derangements of the condyle-disc complex
These disorders present as a range of conditions, most of which may be viewed as a continuum of progressive events. They occur because the relationship between the articular disc and the condyle changes. To understand this relationship, it is appropriate to review briefly a description of normal joint function (Chapter 1).
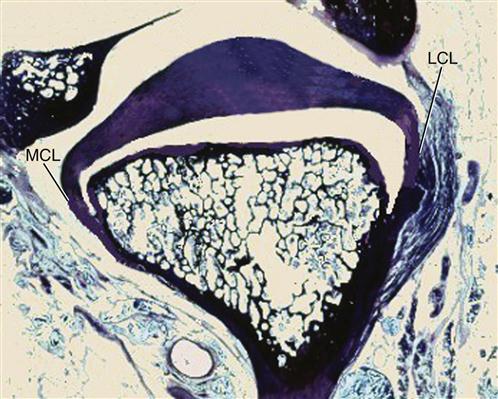
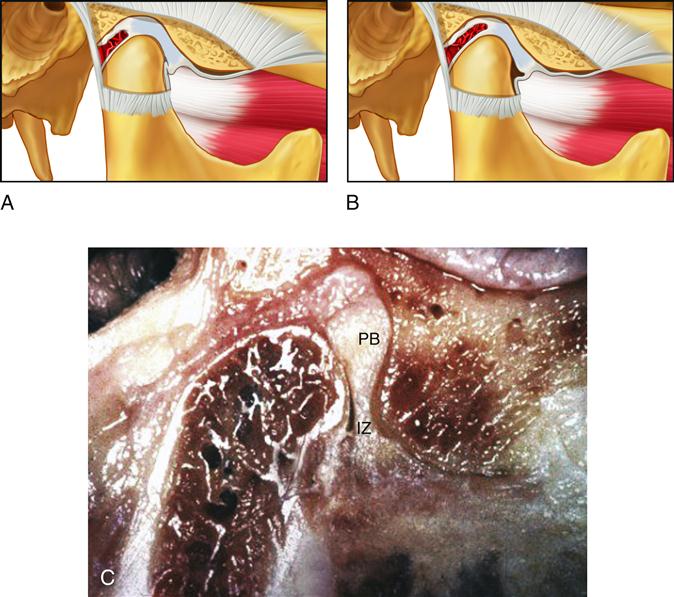
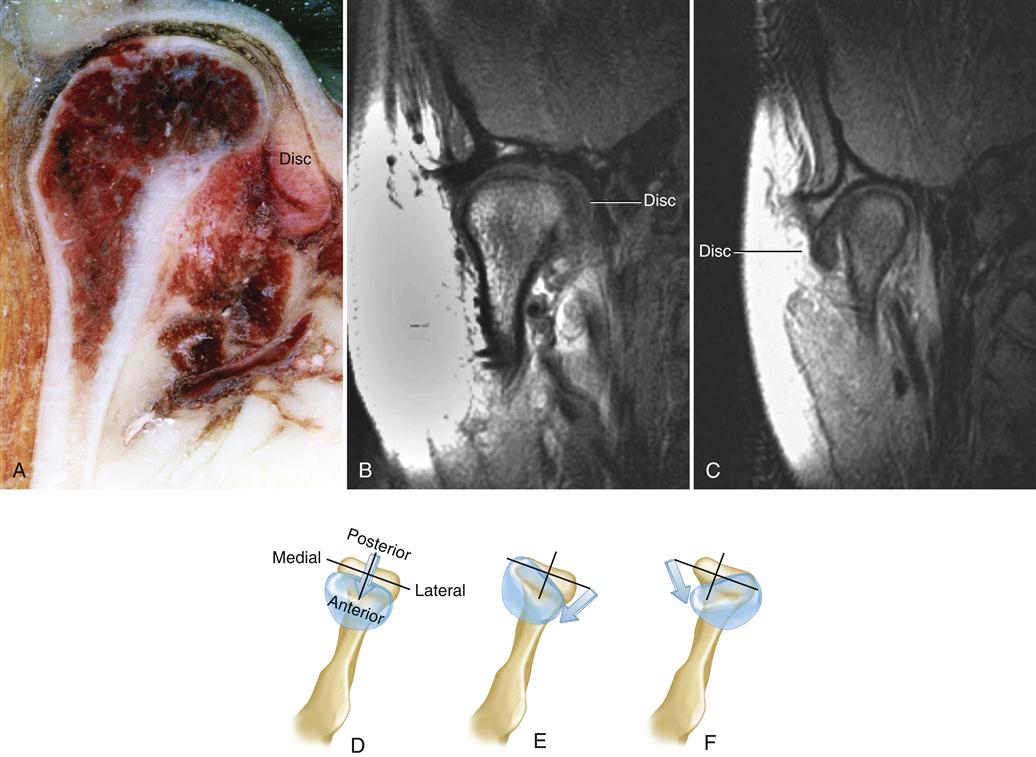
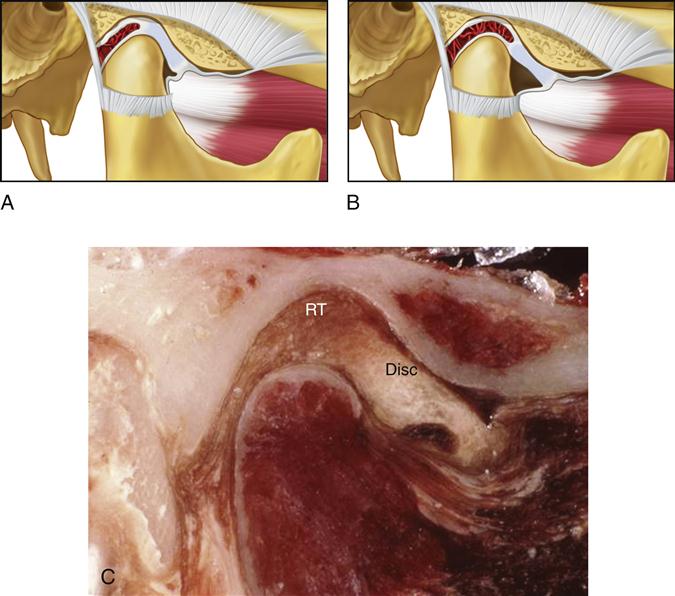
The disc is laterally and medially bound to the condyle by the discal collateral ligaments; thus translatory movement in the joint can occur only between the condyle-disc complex and the articular fossa (Figure 8-5). The only physiologic movement that can occur between the condyle and the articular disc is rotation. The disc can rotate on the condyle around the attachments of the discal collateral ligaments to the poles of the condyle. The extent of rotational movement is limited by the length of the discal collateral ligaments as well as by the inferior retrodiscal lamina posteriorly and the anterior capsular ligament anteriorly. The amount of rotation of the disc on the condyle is also determined by the morphology of the disc, the degree of interarticular pressure, and the superior lateral pterygoid muscle as well as the superior retrodiscal lamina.
When the mouth opens and the condyle moves forward, the disc rotates posteriorly on the condyle. The superior retrodiscal lamina lengthens, allowing the condyle-disc complex to translate out of the fossa. Interarticular pressure provided by the elevator muscles maintains the condyle on the thinner intermediate zone of the articular disc and prevents the thicker anterior border from passing posteriorly through the discal space between the condyle and the articular surface of the eminence. When a person bites on some firm food, the interarticular pressure decreases in the ipsilateral (biting side) joint. To stabilize the joint during this power stroke, the superior lateral pterygoid pulls the condyle-disc complex forward. The fibers of the superior lateral pterygoid that are attached to the disc produce a forward rotation of the disc, allowing the thicker posterior border to maintain intimate contact between the two articular surfaces. The fibers of the superior lateral pterygoid that are attached to the neck of the condyle pull the condyle forward, bracing it against the posterior slope of the eminence.
The superior retrodiscal lamina is the only structure that can retract the disc posteriorly. This force, however, can be applied only when the condyle is translated forward, unfolding and stretching the superior retrodiscal lamina. (In the closed joint position there is no tension in the superior retrodiscal lamina.) The disc can be rotated forward by action of the superior lateral pterygoid, to which it is attached. In the healthy joint the surfaces of the condyle, disc, and articular fossa are smooth and slippery, allowing easy, frictionless movement.
The disc therefore maintains its position on the condyle during movement because of its morphology and interarticular pressure. Its morphology (i.e., the thicker anterior and posterior borders) provides a self-positioning feature that, in conjunction with the interarticular pressure, centers it on the condyle. Backing up this self-positioning feature are the medial and lateral discal collateral ligaments, which do not permit sliding movements of the disc on the condyle.
If the morphology of the disc is altered and the discal ligaments become elongated, the disc is then permitted to slide (translate) across the articular surface of the condyle. This type of movement is not present in the healthy joint. Its degree is determined by changes that have occurred in the morphology of the disc and the degree of elongation of the discal ligaments.
An important concept to remember is that ligaments cannot be stretched. They are made up of collagenous fibers that have particular lengthens. Ligaments determine the border movements of the joint. Stretch implies extension followed by a return to the original length. Ligaments do not have elasticity; therefore, once elongated, they generally remain at that length (see Chapter 1). Once ligaments have been elongated, the biomechanics of the joint is frequently altered (often permanently). This concept applies to all joints and must be appreciated to understand changes that occur with the TMJ.
If, for example, the discal ligaments became elongated in normal closed joint position and during function, interarticular pressure would allow the disc to position itself on the condyle and no unusual symptoms would be noted. However, if the morphology of the disc were altered—such as a thinning of the posterior border accompanied by elongation of the discal ligaments—changes in the normal function of the disc could occur. In the resting closed joint position, the interarticular pressure is very low. If the discal ligaments are elongated, the disc is free to move on the articular surface of the condyle. Since, in the closed joint position, the superior retrodiscal lamina does not provide much influence on disc position, tonicity of the superior lateral pterygoid muscle will encourage the disc to assume a more forward position on the condyle.
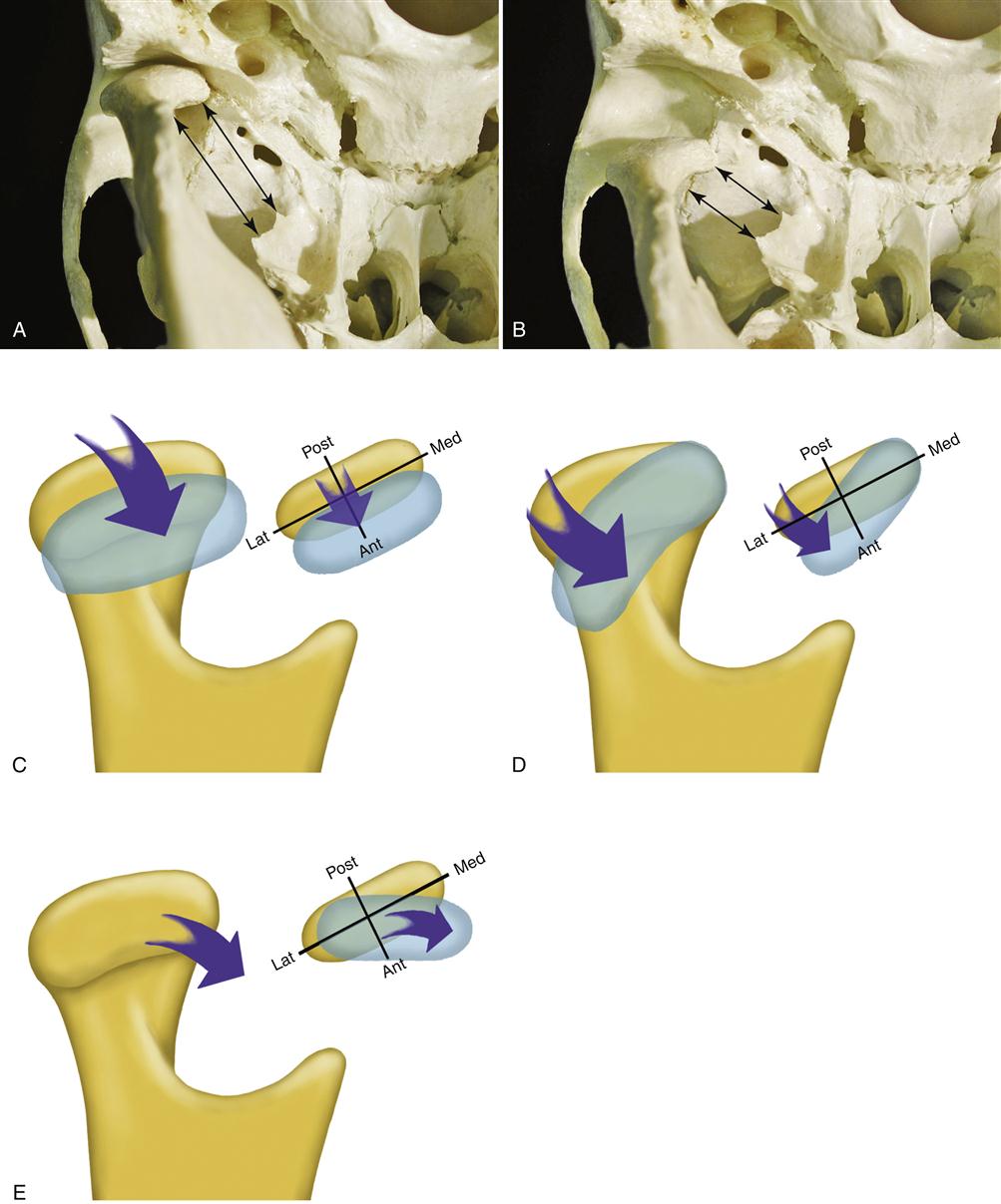
The forward movement of the disc will be limited by the length of the discal ligaments and the thickness of the posterior border of the disc. Actually the attachment of the superolateral pterygoid pulls the disc not only forward but also medially on the condyle (Figure 8-6). If the pull of this muscle is prolonged, over time the posterior border of the disc can become more thinned. As this area is thinned, the disc may be displaced more in the anteromedial direction. Since the superior retrodiscal lamina provides little resistance in the closed joint position, the medial and anterior position of the disc is maintained. As the posterior border of the disc becomes more thinned, it can be displaced further into the discal space so that the condyle becomes positioned on the posterior border of the disc. This condition is known as functional disc displacement (Figure 8-7). Most people report functional displacements of the disc initially as a momentarily altered sensation during movement but usually without pain. Pain may occasionally be experienced when the person bites (a power stroke) and activates the superior lateral pterygoid. As this muscle pulls, the disc is displaced further and tightness in the already elongated discal ligament can produce joint pain.
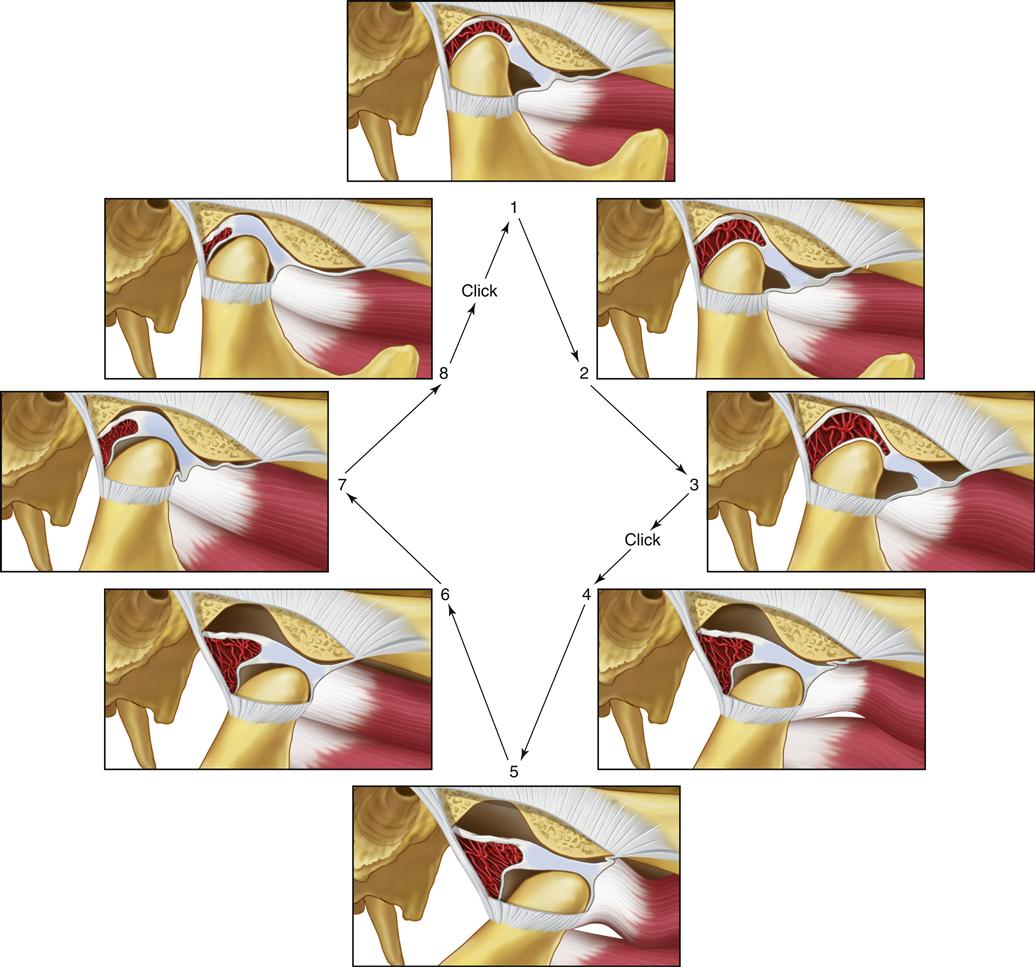
When the disc is in this more forward and medial position, function of the joint can be somewhat compromised. As the mouth opens and the condyle moves forward, a short translatory movement can occur between the condyle and the disc until the condyle once again assumes its normal position on the thinnest area of the disc (intermediate zone). Once it has translated over the posterior surface of the disc to the intermediate zone, interarticular pressure maintains this relationship and the disc is again carried forward with the condyle through the remaining portion of the translatory movement. After the full forward movement is completed, the condyle begins to return and the stretched fibers of the superior retrodiscal lamina actively assist in returning the disc with the condyle to the closed joint position. Again, the interarticular pressure maintains the articular surface of the condyle on the intermediate zone of the disc by not allowing the thicker anterior border to pass between the condyle and the articular eminence.
Once in the closed joint position, the disc is again free to move according to the demands of its functional attachments. The presence of muscle tonicity will again encourage the disc to assume the most anteromedial position allowed by the discal attachments and its own morphology. If muscle hyperactivity were present, the superior lateral pterygoid muscle would have an even greater influence on the disc position.
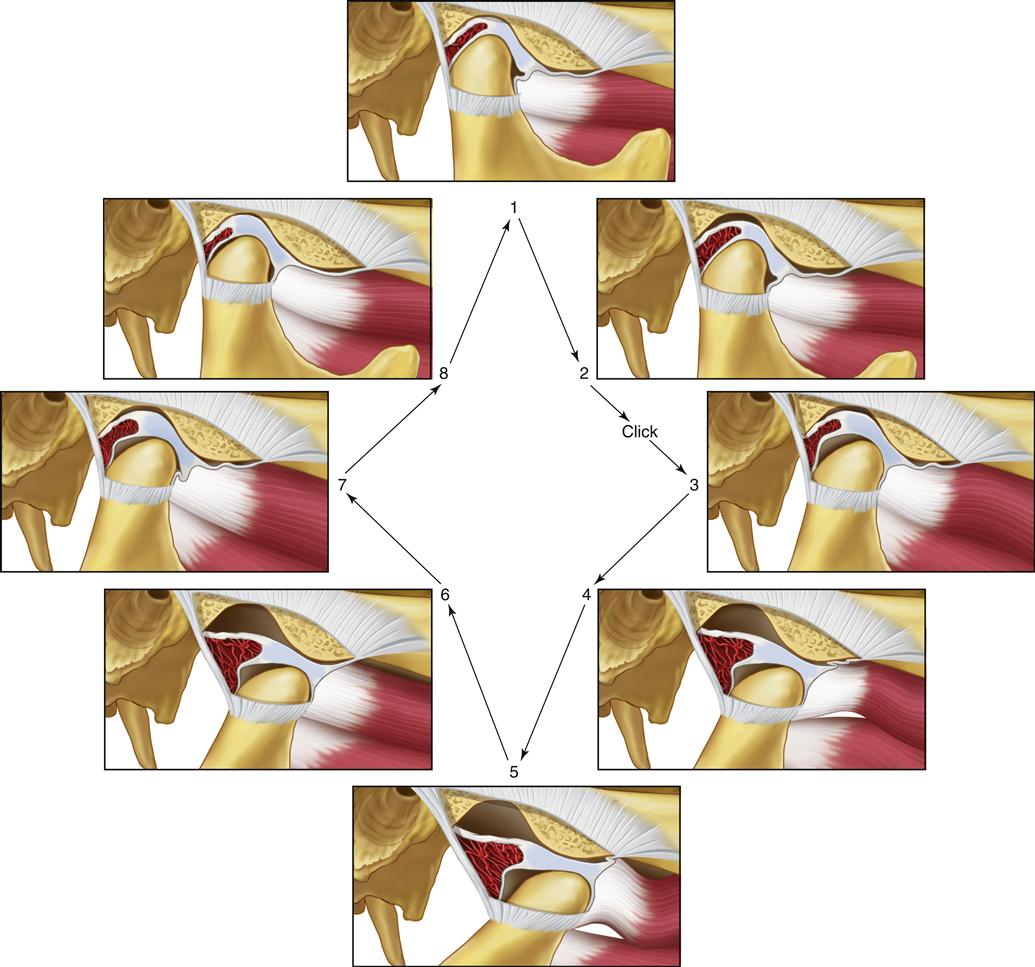
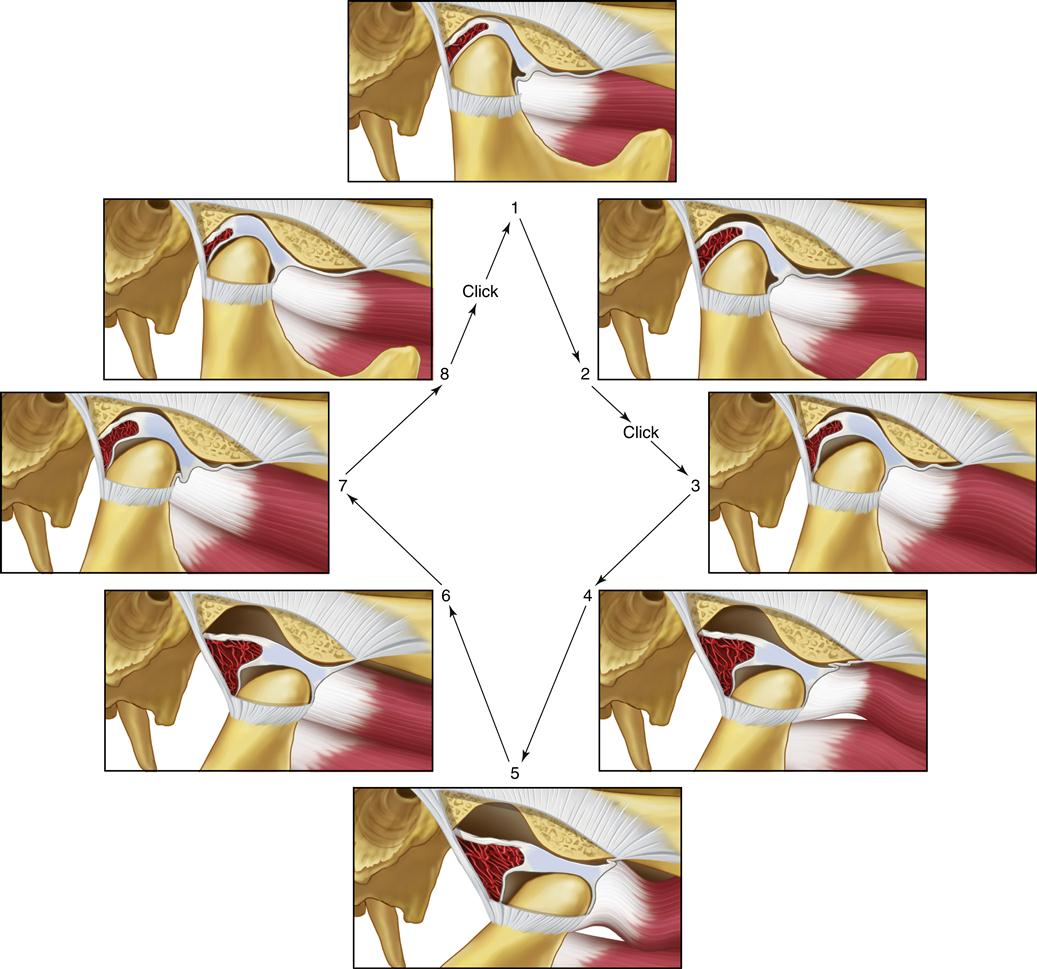
The important feature of this functional relationship is that the condyle translates across the disc to some degree when movement begins. This type of movement does not occur in the normal joint. During such movement the increased interarticular pressure may prevent the articular surfaces from sliding across each other smoothly. The disc can stick or be bunched slightly, causing an abrupt movement of the condyle over it into the normal condyle-disc relationship. A clicking sound often accompanies this abrupt movement. Once the joint has clicked, the normal relationship of the disc and condyle is reestablished, and this relationship is maintained during the rest of the opening movement. During closing of the mouth, the normal relationship of the disc and condyle is maintained because of interarticular pressure. However, once the mouth is closed and the interarticular pressure is lower, the disc can once again be displaced forward by tonicity of the superior lateral pterygoid muscle. In many instances, if the displacement is slight and the interarticular pressure is low, no click is noted during this redisplacement (Figure 8-8). This single click observed during opening movement represents the very early stages of disc derangement disorder or what is also called internal derangement.
If this condition persists, a second stage of derangement is noted. As the disc is more chronically repositioned forward and medially by muscle action of the superior lateral pterygoid, the discal ligaments are further elongated. Continued forward positioning of the disc also causes elongation of the inferior retrodiscal lamina. Accompanying this breakdown is a continued thinning of the posterior border of the disc, which permits the disc to be repositioned more anteriorly, so that the condyle is positioned more posteriorly on the posterior border.119–121 The morphologic changes of the disc at the area where the condyle rests can create a second click during the later stages of condylar return just prior to the closed joint position. This stage of derangement is called the reciprocal click.122
Reciprocal clicking (Figure 8-9) is characterized as follows:
The opening click can occur at any time during that movement depending on disc-condyle morphology, muscle pull, and the pull of the superior retrodiscal lamina. The closing click almost always occurs very near the closed or intercuspal position.
When the disc is anteriorly displaced by the muscles, the superior retrodiscal lamina is being elongated slightly. If this condition is maintained for a prolonged period, the elasticity of the superior retrodiscal lamina can break down and be lost. This area is the only structure that can apply retractive force on the disc. Once this force is lost, there is no mechanism to retract the disc posteriorly.
Some authors123 suggest that the superior lateral pterygoid muscle is not the major influencing factor on the anterior medial displacement of the disc. Although this would appear to be the obvious influencing factor, other features certainly must be considered. Tanaka124,125 has identified the presence of a ligamentous attachment of the medial portion of the condyle-disc complex to the medial wall of the fossa (Figure 8-10). If this ligament were tightly bound, forward movement of the condyle might create a tethering of the disc to the medial. Tanaka124 has also identified that the retrodiscal tissues are tightly attached in the medial aspect of the posterior fossa but not in the lateral aspect. This would suggest that the lateral aspect of the disc can be more easily displaced than the medial, allowing the direction of the disc displacement to be more anteromedial. There are likely to be still other factors that have not yet been described. Further investigation in this area is needed.
As mentioned earlier, the displaced disc is most commonly located anteromedially. This is likely due to the directional forces of the superior lateral pterygoid muscle on the disc. However, the disc can be displaced only anteriorly or, in a few cases, even laterally. Furthermore, the entire disc may not be displaced to the same degree. In other words, in some instances only the medial aspect of the disc is displaced with the remaining portion maintained in its normal position (Figure 8-11). In another instance, only the lateral portion of the disc may be displaced. With all these variations, it is sometimes difficult to determine the exact position of the disc clinically because the joint sounds may be quite different. When this occurs, a soft tissue image (obtained by magnetic resonance imaging) maybe be needed to determine the actual position of the disc (see Chapter 9).
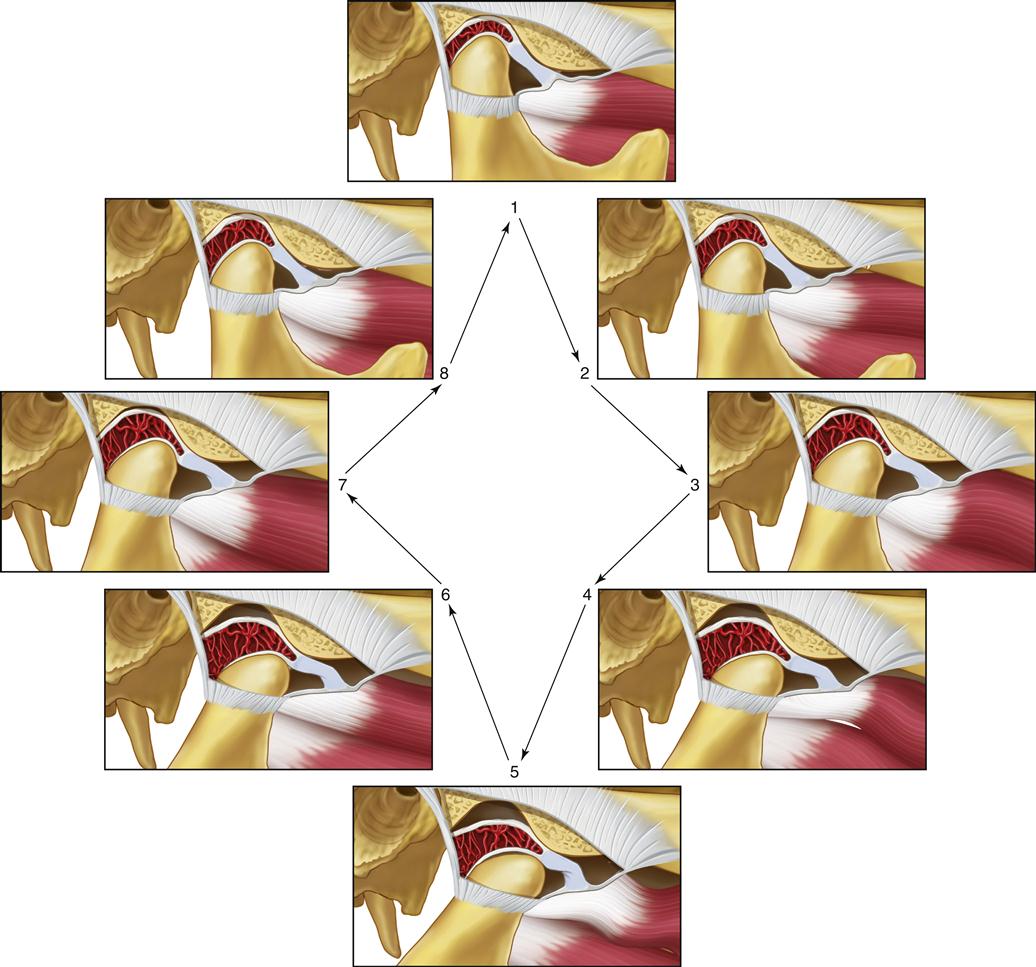
With this in mind, we can now begin a discussion of the next stage of disc derangement. As previously discussed, the longer the disc is displaced anteriorly and medially, the greater the thinning of its posterior border and the more the lateral discal ligament and inferior retrodiscal lamina will be elongated.126 Also, protracted anterior displacement of the disc leads to a greater loss of elasticity in the superior retrodiscal lamina. As the disc becomes more thinned and flat, it further loses its ability to self-position on the condyle, thus allowing more translatory movement between condyle and disc. The more freedom the disc has to move, the greater the positional influence from the attachment of the superior lateral pterygoid muscle. Eventually the disc can be forced through the discal space, collapsing the joint space behind it. In other words, if the posterior border of the disc becomes thin, the functional attachment of the superior lateral pterygoid can encourage an anterior migration of the disc completely through the discal space. When this occurs, interarticular pressure will collapse the discal space, trapping the disc in the forward position. Then the next full translation of the condyle is inhibited by the anterior and medial position of the disc. The individual then feels the joint being locked in a limited closed position. Since the articular surfaces have actually been separated, this condition is referred to as a functional dislocation of the disc (Figure 8-12).
As already described, a functionally displaced disc can create joint sounds as the condyle skids across the disc during normal translation of the mandible. If the disc becomes functionally dislocated, the joint sounds are eliminated, since no skidding can occur. This can be helpful information in distinguishing a functional displacement from a functional dislocation.
Some people with a functional dislocation of the disc are able to move the mandible in various lateral or protrusive directions to accommodate the movement of the condyle over the posterior border of the disc, thus the locked condition is resolved. If the lock occurs only occasionally and the individual can resolve it with no assistance, it is referred to as a functional dislocation with reduction. The patient will often report that the jaw “catches” when the mouth is opening wide (Figure 8-13). This condition may or may not be painful depending on the severity and duration of the lock and the integrity of the structures in the joint. If the condition is acute, having a short history and duration, joint pain may be associated only with elongation of the joint ligaments (such as trying to force the jaw open). As episodes of catching or locking become more frequent and chronic, ligaments break down and innervation is lost. Pain becomes less associated with ligaments and more related to forces placed on the retrodiscal tissues.
The next stage of disc derangement is known as functional disc dislocation without reduction. This condition occurs when the person is unable to return the dislocated disc to its normal position on the condyle. The mouth cannot be opened maximally because the position of the disc does not allow full translation of the condyle (Figure 8-14). Typically the initial opening will be only 25 to 30 mm intrincisally, which represents the maximal rotation of the joint. The person is usually aware of which joint is involved and can remember the occasion that led to the locked feeling. Since only one joint usually becomes locked, a distinct pattern of mandibular movement is observed clinically. The joint with the functionally dislocated disc without reduction does not allow complete translation of its condyle, whereas the other joint functions normally. Therefore when the patient opens wide, the midline of the mandible is deflected to the affected side. Also, the patient is able to perform a normal lateral movement to the affected side (only the condyle on the affected side rotates). However, when movement is attempted to the unaffected side, a restriction develops (the condyle on the affected side cannot translate past the anterior functionally dislocated disc). The dislocation without reduction has also been termed a closed lock,122 since the patient feels that he or she is locked near the closed-mouth position. Patients may report pain when the mandible is moved to the point of limitation, but pain does not necessarily accompany this condition.127–130
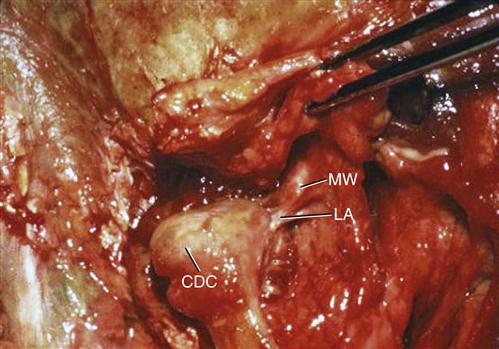
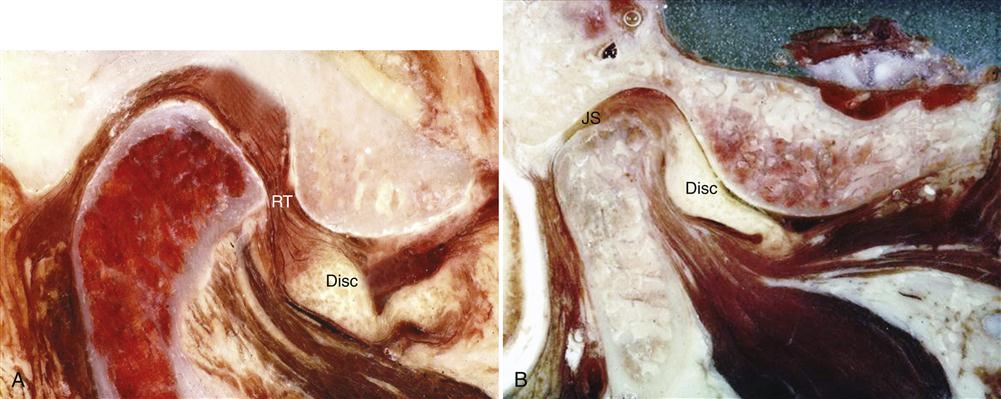
If the closed lock continues, the condyle will be chronically positioned on the retrodiscal tissues. These tissues are not anatomically structured to accept force (Figure 8-15). Therefore, as force is applied, a great likelihood arises that the tissues may break down.120,131,132 With this breakdown comes tissue inflammation (which is discussed as another category of TMJ disorders).
Any condition or event that leads to elongation of the discal ligaments or thinning of the disc can cause these derangements of the condyle-disc complex. Certainly one of the most common factors is trauma. Two general types of trauma must be considered: macrotrauma and microtrauma.
Macrotrauma
Macrotrauma is any sudden force to the joint that can result in structural alterations. The most common structural alterations affecting the TMJ are elongations of the discal ligaments. Macrotrauma can be subdivided into two types: direct and indirect.
Direct trauma
There is little question that significant direct trauma to the mandible, such as a blow to the chin, can instantly create an intracapsular disorder. If this trauma occurs when the teeth are separated (open-mouth trauma) the condyle can be suddenly displaced from the fossa. This sudden movement of the condyle is resisted by the ligaments. If the force is great, the ligaments can become elongated, which may compromise normal condyle-disc mechanics. The resulting increased looseness can lead to discal displacement and to the symptoms of clicking and catching. Unexpect/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


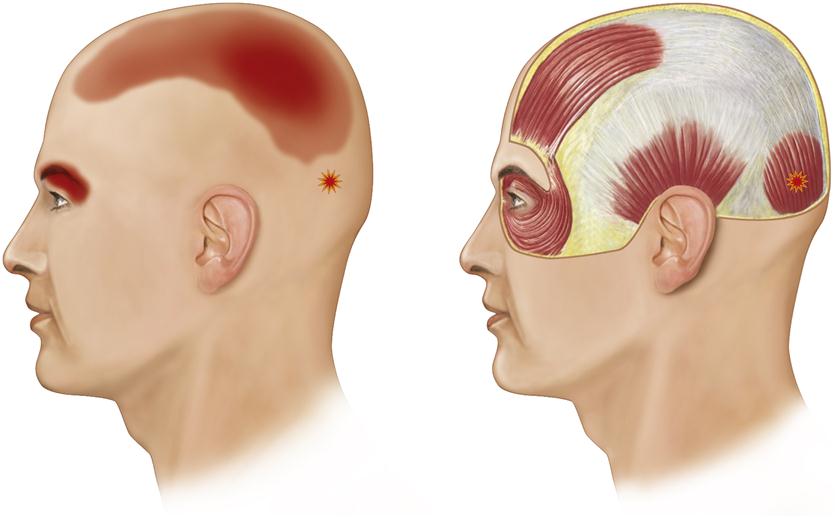
 ) in the occipital belly of the occipitofrontalis muscle can produce referred headache pain behind the eye.
) in the occipital belly of the occipitofrontalis muscle can produce referred headache pain behind the eye.