Chapter 7 An Oral and Maxillofacial Surgeon’s Role in Advanced MDI Therapeutics
Engineering Assisted Surgery™, MDIs in Functional Reconstructive Surgery Within Great Britain and New Zealand Venues
Engineering Assisted Surgery™ (EAS) Medical Art and Surgical Craft
The Art and Craft of Clinical Practice
Applications of EAS in Healthcare
Head and Neck Surgery: Cost of Treatment
Projections of Cost Savings in Clinical Practice
Application Of EAS to the Healthcare Industry
EAS: Oral and Maxillofacial Surgery Model
Case Discussion 1: Marginal Mandibulectomy and Concomitant Reconstruction of the Dentition with an MDI Technique
Case Discussion 2: The Management of Major Facial Trauma with a Combined EAS/MDI Technique
Case Discussion 3: Maxillary Atrophy
Case Discussion 4 Maxillary Atrophy
Case Discussion 5 Customized Hybrid Implant Systems
Engineering Assisted Surgery™ (EAS) Medical Art and Surgical Craft
Engineering Assisted Surgery™ (EAS) may be defined as “the application of industrial and engineering systems to healthcare delivery”15 with respect to existing interventions and new and evolving surgical procedures and includes:
• Identification of and appropriate industrial input in healthcare modernization programs at a global level;
• Facilitation of transfer of industrial and engineering solutions to healthcare;
• Bringing industrial concepts of service, management, and delivery into healthcare;
• Improved diagnosis and replicable 3D planning for all medical and surgical specialities;
• Customized medical devices (e.g., tissue engineering, implants, custom jigs);
• Reduction in intervention trauma with appropriate use of available resources;
• A universal improvement of quality and standardization of outcome;
• Facilitation of audit with demonstrated significant reduction in cost and intervention;
• Improved ergonomics and reduction in waiting lists;
Logistical Considerations
Reconstructive surgery traditionally involves long∗ complex procedures, which often involve the harvesting of complex composite free flaps from a second surgical site and microvascular techniques. The dentition is reconstructed using osseointegrated titanium implants in multistaged procedures.
Functional Reconstruction
Mini Dental Implants
The introduction of Dr. Victor Sendax’s concept of a mini dental implant (MDI) system17,18,19,20,21 has produced a major impact in tissue engineering techniques employed in otolaryngology/head and neck surgery, craniomaxillofacial surgery, and oral and maxillofacial reconstructive surgery.
Definition of MDI
In UK MDI training workshops, Peckitt defines MDIs with the following characteristics:
Indications for the Use of MDIs
Medical Considerations
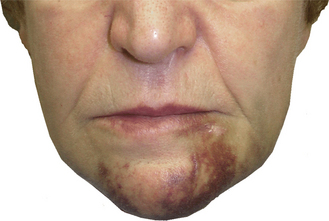
Minimal surgery is needed in nearly all patient groups. MDIs have advantages for patient groups in which minimal surgical trauma is an added advantage or quite simply mandatory. MDI placement is often flapless, predictable, and quick. This offers advantages to medically compromised patients (e.g., patients with stable anticoagulation and antiplatelet medication regimens) and those undergoing major reconstructive maxillofacial surgery (Figure 7-1).
Surgical Considerations
Five-year survival rates for patients with advanced squamous cell carcinoma of the oral cavity are poor and have not improved significantly in the past 30 years.1,13 Current treatment modalities are:
• Multimodal, involving complex composite surgery, radiotherapy, and possible chemotherapy;
• Associated with significant perioperative morbidity:
• Associated with significant perioperative mortality as a function of the metabolic response to major surgical trauma.
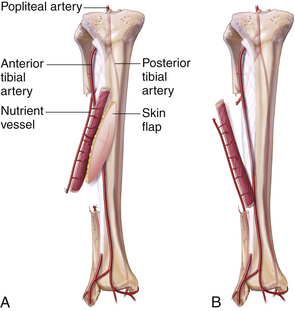
Although there have been significant advances in free flap tissue transfer, especially in the reconstruction of the hemimandible and anterior mandible, the introduction of techniques such as the free fibula flap has an association with both donor and recipient site morbidity, cumulating in the disaster of flap loss and loss of the patient (Figure 7-2).
Patients with oral cancer are commonly debilitated and are more likely to have higher American Joint Committee on Cancer (AJCC) fitness scores.3 The implications are that this group of patients is more likely to succumb to the consequences of major surgery. Therefore offering patients treatment options involving reduced surgical trauma has distinct advantages (Table 7-1).
| AJCC (H) Performance Scale | Definition |
|---|---|
| H0 | Normal activity |
| H1 | Symptomatic and ambulatory |
| H2 | Ambulatory > 50% of time Occasionally needs assistance |
| H3 | Ambulatory < 50% of time Nursing care required |
| H4 | Bedridden May need hospitalization |
Moreover, major surgical treatment modalities are costly to the purchasers of healthcare, and if neither cure nor adequate palliation can be achieved at reasonable cost, the value of such treatment protocols requires reappraisal.22
Logistical Issues
The low cost of MDIs is of special interest to state healthcare systems providing complex composite reconstructive head and neck cancer services. With modern planning techniques, MDI placement is possible at the time of resection and reconstruction with presurgical manufacture of the dental prosthesis. As we shall see, treatment is even possible without the use of flap surgery. This further improves the efficiency of the treatment modality, making treatment possible in a single surgical procedure. The financial implications of this scenario are profound for the patient whose surgery is simplified, for the provider with reduced demand for resources, and for the purchaser with significant reduction in cost (Table 7-2).
| Type of Surgery | Annual Cost |
|---|---|
| Reconstructive surgery | ≤18,125,000 ($28, 206,078) |
| Engineering assisted surgery™ | ≤10,537,875 ($16,399,014) |
| Savings | ≤7,587,125 ($11,807,064) |
Indications: MDI Implants in Oral Rehabilitation?
Anatomical Considerations
Atrophic Ridges
Ridge Height
Although it has been suggested that MDI implants should not be used as a transmandibular system, it is our experience that penetration of the inferior mandibular border results in no problems. This method permits the placement of larger diameter implants down to the lower border of the mandible with an increased surface area for osseointegration. Currently the role of the denser cortex at the lower border is undetermined; however, it is likely that this will enhance the osseointegration process.
Any protruding sharp MDI tips may be smoothed as required before wound closure.
Factors Influencing Functional Dentition
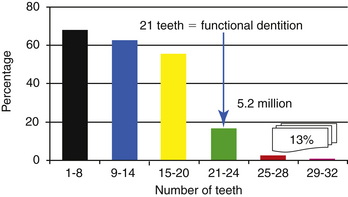
The 1998 Adult Dental Health Survey (Oral Health)26 in the United Kingdom documented that a minimum of 21 teeth are required for functioning dentition (Figure 7-3).
In a base sample size of 923 adults with dental prostheses, speaking difficulties (9%), eating difficulties (37%), and other problems (16%) were recorded. An overall incidence of prosthetic problems was documented in 40% of patients sampled (Tables 7-3 to 7-6).
| Problem with Speaking | Percentage |
|---|---|
| Loose denture/slips when talking | 4% |
| Alters or slurs speech | 3% |
| Other speaking problems | 2% |
| No problems | 93% |
Data modified from Adult Dental Health Survey Oral Health in the United Kingdom 1998. Office for National Statistics; London: The Stationery Office.
TABLE 7-4 Problems with Eating with Dentures
| Problems with Eating | Percentage |
|---|---|
| Food sticks under denture plate | 12% |
| Loose/denture/slips when eating | 9% |
| Hurts gums | 8% |
| Cannot chew or bite well | 5% |
| Other eating problems | 3% |
| No problems | 74% |
36% of patients have eating difficulties.
Data modified from Adult Dental Health Survey Oral Health in the United Kingdom 1998. Office for National Statistics; London: The Stationery Office.
TABLE 7-5 Other Denture Problems
| Other Denture Problems | Percentage |
|---|---|
| Loose dentures | 5% |
| Gets ulcers | 3% |
| Sore gum/plate rubs gums | 3% |
| Denture worn down | 1% |
| Other denture problem | 4% |
| No problems | 84% |
16% of patients have other denture problems.
Data modified from Adult Dental Health Survey Oral Health in the United Kingdom 1998. Office for National Statistics; London: The Stationery Office.
| Prosthetic Outcome | Percentage |
|---|---|
| Prosthetic problems (incidents) | 40% |
| No problems | 60% |
Data modified from Adult Dental Health Survey Oral Health in the United Kingdom 1998. Office for National Statistics; London: The Stationery Office.
Because stability of the lower denture is now so effective with inexpensive MDIs and outcomes so superior (compared with the tissue-borne full lower denture prosthesis, which is indicated only if dental implant placement is contraindicated), Peckitt now advocates that the MDI-retained lower overdenture is now the primary denture treatment option.22
MDIs and Complex Maxillofacial Reconstruction
• Simple fused abutment system
• MDI max system is particularly useful in less dense bone
• Immediate loading possible in mandible
• Concomitant placement at time of resection and reconstruction
• Placement without flap surgery
• Presurgical fabrication of prosthesis
• Effective in maxilla, mandible, and craniofacial regions
• Able to be used in curative procedures
• Especially useful in palliative procedures and associated issues related to the cost of effective palliation
• Postoperative irradiation may be given
• Implant loss is readily retrievable, often without bone grafting
Contraindications to the Use of MDIs
| Medical | Psychiatric disease |
| Chronic facial pain syndromes | |
| History of infected endocarditis | |
| Rheumatic fever |
| Surgical | Severe jaw atrophy (bone height) |
| Grade 4 bone density (not necessarily) | |
| Heavy occlusion that cannot be relieved | |
| Gross dental sepsis | |
| Immediate tooth replacement after extraction may present problems |
Peckitt has demonstrated the successful use of MDI implants in severe maxillary atrophy16 and in grade 4 bone density in conjunction with bone grafting and platelet rich plasma techniques,12 with stability at 9 years.
The Art and Craft of Clinical Practice
• The discovery of osseointegration;
• Transmucosal or transcutaneous implant systems (in particular the MDI concept of Dr. Victor Sendax);
• New (bio)engineering materials;
• Advanced computer technology;
• Computer assisted diagnosis, design, and manufacture;
• Rapid prototyping, reverse engineering, and biomodel manufacture;
• New manufacturing processes;
Successful Outcome
The parameters of successful outcome are often arbitrary and based on current practice, which does not necessarily portray the best outcome possible and does not take into account recent developments especially in the field of EAS. Best practice is a complex function of many parameters in relation to accepted national standards of outcome. In the United Kingdom, crucial data are not freely available or have not been documented; for many parameters, no national standards have been agreed upon. This has an adverse effect on clinical audit, evidence-based practice, and clinical governance issues.
Applications of EAS in Healthcare
Let us therefore examine the effects of EAS on the delivery of healthcare on the available evidence.
Oral Cancer
The Logistics of MDIs in Orofacial Reconstruction
Each year in the United Kingdom there are more than 2500 new cases of oral cancer14,15,24 (approximately 1% of all cancer registrations) with an annual mortality of approximately 1400 compared with 1339 deaths from cervical cancer in 1995. Some evidence shows that oral cancer is becoming more common in women and younger patients in the United Kingdom and other countries. Oral cancer is twice as common in men.
Although the incidence of oral cancer was static in the 1980s, now signs show a rising incidence. Four patients die of this disease every day in the United Kingdom.4
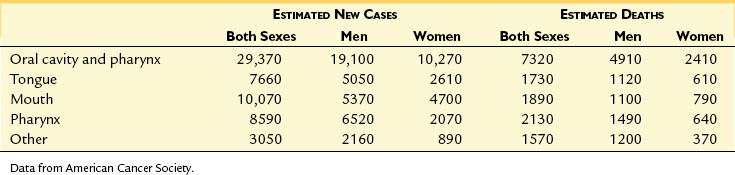
In the United States in 2005, new cases of cancer of the oral cavity and pharynx were estimated at 29,370, with an estimated annual mortality of 73202 (Table 7-7).
Lymph Node Status and Survival
In a series of 2550 cases of epidermoid carcinoma of the oral cavity and oropharynx, Spiro et al25 observed a 14% reduction in 5-year survival—from 51% for the clinically negative neck (cN0) to 37% if only one node was histologically diagnosed positive for metastatic tumor,. If multiple unilateral nodes were histologically positive, the 5-year survival was reduced to 24% (i.e., the survival rate was nearly halved). For histologically involved bilateral nodes, the 5-year survival dropped to 5%. This series of patients roughly numbers the new cases that would be expected to present annually in the United Kingdom.
Head and Neck Surgery: Cost of Treatment15
Average Costs of Treatment: One Live Patient at 2 years
The average cost of a 2-year survival episode is documented at ≤85,000 (USD $132,000) for patients treated with complex composite microvascular techniques (assuming a 70% 2-year mortality rate at ≤25,000 (USD $38,900) per case in line with Lavery’s estimation). In a pilot study of seven patients with cancer treated in Doncaster Royal Infirmary with customized titanium implants,15 zero mortality was recorded at 4.5 years at a cost of ≤14,535 (USD $22,600) per case episode for those patients treated 1994 to 1996.
Complex composite microvascular flap reconstructive techniques are reserved for patients with advanced disease, the majority of which affect the mandible. If the percentage of cases presenting as T3/T4 cases of 28% is accepted, approximately 725 microvascular oral reconstruction episodes per year are carried out in the United Kingdom, at an annual cost of ≤18,125,000 (USD $28,206,000) (assuming the estimated cost of ≤25,000 (USD $38,9000) per episode has remained unchanged since 1993).15
The cost of free flap surgery in New Zealand has been estimated at NZ $60,000 to NZ $80,000 per case intervention (Izzard: 2007 Auckland Head and Neck Cancer Centre) (Table 7-8).
TABLE 7-8 Cost Comparison: Composite Free Flap Transfer Versus Engineering Assisted Surgery (EAS)
| Composite Free Flap Transfer | EAS |
|---|---|
| ≤25,000 (USD $38,900)/case | ≤14,535 (USD $22,600)/case (7 patients) |
| 70% expected mortality @ 2 years | 0% mortality @ 4 years |
| Average cost: 2 year survival ≤85,000 (USD $132,000) | Average cost: 2 year survival ≤14,535 (USD $22,600) |
Data from Peckitt: EAS Costs 1994-1996. Doncaster Royal Infirmary, United Kingdom, www.maxfac.com/costsavings.html.
Simplification of treatment plans incorporating (EAS techniques has demonstrated a reduction in cost (see Table 7-2) of treatment to ≤14,535 (USD $22,600) per surgical intervention and, in comparison, the national annual total cost of treatment would be ≤10,537,875 (USD $16,399,000) for this option, an annual saving to the nation of ≤7,587,125 (USD $11,807,000) plus an associated improvement in long-term overall mortality figures and statistical significance even on a small sample size.
Research and Development
The palliative care of patients with head and neck cancer is discussed by Lovel,11 who quotes Stjernsward: “No further research is required; the knowledge of what needs to be done exists. The single most useful thing that we can do is to make sure that every patient benefits from that knowledge.”
However, “If surgical treatment is a component of such palliation, it is argued that there is still much to learn” (Peckitt).15
Treatment Planning: Huge Cost Savings with Biomodels
For the management of complex reconstruction and trauma cases, savings are higher per unit case as a function of the consequences of reduced surgical trauma. Savings of ≤30,000 (USD $46,685) per case intervention are possible1 with projections of reduced operating times, less dependency on critical care facilities, earlier discharge from hospital, and enhanced rehabilitation.
EAS: Discussion
New developments in engineering, used for the first time in oral and maxillofacial surgery,15,22 permit the manufacture of accurate anatomical biomodels of the skeleton from CT scans, using a variety of reverse engineering methods. Biomodels have been used in treatment planning and the design and manufacture of customized titanium implants for the single staged reconstruction of the orofacial region using very simple cost effective interventions. These may carried out without surgery from a second surgical site and obviate the necessity for complex flap surgery.
We now have a treatment option that permits endosseous stabilization of a prosthetic device:
• With the advantages of a flapless technique and minimal trauma;
• In cases of compromised osseous width and/or bone volume;
• As a single staged or immediate technique;
• To produce an excellent quality of prosthetic retention and palliation;
• With simple and economical salvage in the event of implant loss.
As this technology is development and mastered, reappraisal of the principles of surgery in general are warranted, especially in relation to the incredible accuracy that is possible using these techniques and the potential of the elimination of operator error.
Resource Implications
• Short simple operations; single site and/or single staged surgery;
• Reduction in the use of donor sites and their morbidity if flaps are not used;
• Projections of reduced morbidity; projections of reduced perioperative mortality;
• Reduction in use of critical care facilities;
• Surgical planning is facilitated;
• Nonmutilating reconstructions are possible;
• Excellent esthetics and immediate dental rehabilitation is possible;
• Tumor recurrence is not possible in the titanium prosthesis;
• Intraoral wound breakdown is not related to failure of the technique;
• Implants can be salvaged in the presence of complications that would have resulted in total loss of alternative surgical methods of reconstruction:
• Conventional surgery can still be employed in cases of implant failure;
Indications For EAS
EAS has relevance to many specialties, especially maxillofacial surgery and orthopaedics:
• To promote the accuracy of planning and delivery of surgical treatment plans.
• To facilitate the transfer of the surgical plan from biomodel to patient.
• To replicate bone resection cuts exactly at operation with customized cutting jigs.
• To accurately determine positions of the bones with position jigs.
• To eliminate operator error.
• To facilitate single stage reconstructive surgery.
• To facilitate single site surgery.
• To reduce the dependency on postoperative critical care.
• To guarantee quality of outcome related to technique.
• To facilitate audit of outcomes.
• To promote the principles of clinical effectiveness and governance.
Projections of Cost Savings in Clinical Practice
It is likely that cost savings and enhanced outcome illustrated in oral and maxillofacial reconstructive surgery will be mirrored in other specialties, especially in orthopedics; in the United Kingdom the logistics of major trauma management and their outcomes have been reassessed.5
Application of EAS to the Healthcare Industry
The consequences of this modus operandi are that interventions rely heavily on (variable) human ability, performance, and a complex and expensive resource network, which is inefficiently used. The quality of outcome must vary as a consequence of the inconsistencies related to planning variables, the human variable, the degree of clinical trauma required to achieve the outcome.
EAS: Oral and Maxillofacial Surgery Model
In maxillofacial surgery, EAS techniques have been shown to facilitate:
• Accuracy of diagnosis and treatment planning;
• Translation of a 3D plan into a 3D patient;
• Reduction in surgical trauma and operating time;
• Accuracy in existing interventions;
• Treatment previously thought impossible using established interventions;
• The creation of new procedures that simplify treatment;
• The conversion of staged multiple interventions into a single intervention;
• Promotion of normal esthetics and functional rehabilitation;
MDIs and Mandibular Reconstruction
It has long been known within the sphere of dental surgery that the oral cavity has the ability to heal by secondary intention without complication, even in the environment of hostile sepsis. Postextraction sockets illustrate this “par excellence” and yet this innate gift is ill recognized by those providing reconstructive services within this hostile oral environment. This situation has led to the generation and propagation of myths and guidelines on the requirements for oral healing that have in reality no basis in fact or experience (Figure 7-4).
• Degloving injuries of the lips;
• Orthognathic surgery, especially maxillary bone grafting following Le Fort I downfracture: In this scenario nasal mucosa does not break down even though the maxillary graft is initially avascular;
• Orbital reconstruction (bone graft): In this scenario, exposure of the graft to the maxillary sinus does not result in infection and loss of graft;
• Similarly, sinus lift surgery in cases where the schneiderian membrane is breached does not invariably result in the loss of graft;
• The use of deepithelialized flaps in reconstructive surgery.
The routine use of flaps for bone cover in the oral cavity must be questioned.
Anterior Rim Sparing Mandibulectomy
In marginal mandibulectomy, the dental clearance is carried out, only this time with an oscillating saw and the dental clearance concomitantly with the jaw resection.
CASE Discussion 1
Marginal Mandibulectomy and Concomitant Reconstruction of the Dentition with an MDI Technique
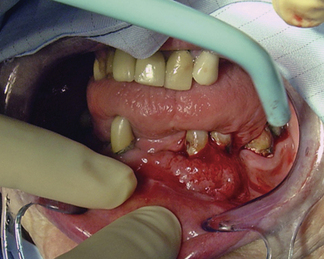
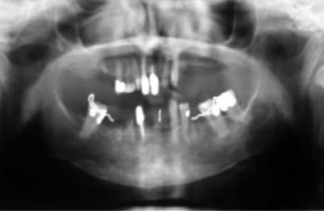
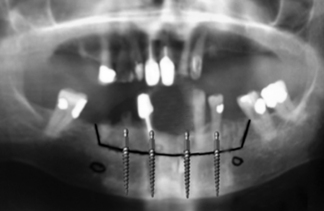
An 82-year-old woman presented with a well differentiated squamous cell carcinoma of the gingiva.
Past Medical History: Poorly controlled hypertension (Figures 7-5 and 7-6).
Treatment Planning
Selected treatment option: Marginal mandibulectomy without neck dissection.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses