- Widening of the apical periodontal ligament space of the root treated 12.
- The existing root filling appeared reasonably well condensed, but was under-extended.
Diagnosis and treatment planning
The diagnosis was chronic periapical periodontitis associated with an existing root canal treatment.
The patient’s symptoms were due to inflammation of the periapical tissues as a result of infection within the root canal space. The bacteria responsible for the infection may have survived the original endodontic treatment due to inadequate or incomplete disinfection of the root canal. Alternatively, the bacteria may have entered the root canal system subsequently, by way of coronal leakage.
What were the treatment options for this tooth?
- Root canal re-treatment followed by replacement of the crown.
- Peri-apical surgery.
- Extraction followed by replacement with: (a) implant-retained crown, (b) bridge, (c) removable partial denture.
- Leave alone.
Following discussion of the various treatment options, the patient decided to proceed with root canal re-treatment of the 12. The patient was advised that a post may be required to retain the new crown, and that a final decision could only made once the existing crown had been removed and the amount of remaining sound coronal tooth structure had been assessed (Figure 6.3.2).
Figure 6.3.2 Remaining tooth structure following crown removal.

Why was it necessary to remove the crown?
- To assess the amount of remaining tooth structure, i.e. to know whether the tooth is restorable.
- To ensure that the tooth is free of caries, particularly if the crown margins appear defective.
- To minimize the removal of sound tooth tissue during access cavity preparation, particularly when the existing cast restoration is not representative of the original form and position of the tooth.
- To allow unimpeded access to the root canal system, aiding in the location of the root canal(s), as well as obtaining straight-line access.
- To allow the operator to decide on the most appropriate method for restoring the tooth based on the amount and position of the remaining tooth structure. The decision as to whether a post-retained restoration is necessary cannot be made without assessment of the remaining coronal tooth structure.
Treatment
Following local anaesthesia, a putty index of the upper incisor teeth was taken. The porcelain-bonded crown on the 12 was sectioned using a tungsten carbide bur, once the crown had been sectioned, it was loosened and removed. The tooth was assessed, and judged to be restorable, after which rubber dam isolation was obtained. The root canal was located, and the existing gutta-percha root filling was removed using Gates Glidden burs and stainless steel hand files. Copious irrigation with sodium hypochlorite solution was carried out throughout the procedure. The working length of the root canal was determined using an electronic apex locator; and a radiograph was taken to verify this reading (Figure 6.3.3). Root canal preparation was then carried out using a combination of stainless steel hand files and nickel–titanium rotary instruments. After completion of root canal preparation, the canal was rinsed with ethylenediamine tetra-acetic acid (EDTA) solution, followed by a final flush with sodium hypochlorite. The canal was dried with paper points, and the apical 5 mm of the root canal was obturated with gutta-percha and sealer using warm vertical compaction. The patient was advised that the tooth would require a post-retained crown.
Figure 6.3.3 Working length radiograph showing negotiation of the root canal to full length. Characteristically, upper lateral incisors demonstrate a disto-palatal curvature in the apical third.

When is post retention necessary?
Posts are necessary when there is insufficient tooth structure to support the coronal restoration. In most cases where a post is required, the definitive restoration will involve the provision of a crown. The purpose of a post in this case was to facilitate the retention of the core; this core or foundation could then be used for retention of the crown.
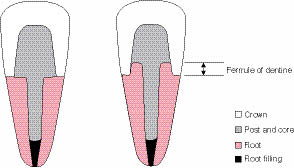
What is meant by the ferrule effect?
The ferrule effect refers to the circumferential collar of cast metal or ceramic (provided by a crown), which encircles the near parallel walls of dentine, coronal to the margins of the crown preparation (Figure 6.3.4).
Figure 6.3.4 The ‘ferrule effect’ refers to the circumferential band of a crown that encircles the remaining coronal tooth structure. Ideally, there should be at least 2 mm of sound dentine (height) which is encased by the crown margins. The ferrule reduces the incidence of root fracture and also provides an optimal seal. (a) A post-crowned tooth with no ferrule. The fulcrum axis is such that occlusal forces are transmitted entirely into the root with no protection from the remaining tooth structure, (b) A post-crowned tooth with a ferrule. The presence of an adequate ferrule of dentine moves the axis of rotation and dissipates forces more favourably, reducing the risk of root fracture.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


