5
Renal and Urinary Tract Disease
I. Background
Renal and urinary tract diseases encompass a number of different entities, but the major individual disease process affecting the oral cavity and dental treatment is renal or kidney disease. Kidney disease is a major public health problem throughout the world, and as it progresses, results in a concomitant decrease in kidney function and is associated with complications in nearly all organ systems. It is linked to poor health outcomes and increasing medical expenditures.
Description of Disease/Condition
Kidney disease and kidney failure can be classified broadly as acute or chronic renal failure (CRF). CRF leads to the deterioration of nephrons and the functional unit of the kidney, and includes a broad spectrum of disease processes. CRF is defined as a progressive loss of kidney function and the development of systemic complications, namely cardiovascular disease.
Acute renal failure (ARF) is characterized by a sudden loss of kidney function, as evidenced by oliguria or anuria and an increase in blood urea nitrogen (BUN) or serum creatinine.
There are numerous causes of ARF, which can be classified as
- diminished kidney perfusion (prerenal);
- glomerular, vascular, or tubulointerstitial/acute tubular necrosis (renal);
- obstruction of the urinary tract (postrenal).
Pathogenesis/Etiology
The most common causes of CRF are diabetes mellitus (34%), hypertension (25%), and chronic glomerulonephritis (16%). Other common causes include systemic lupus erythematosus, neoplasms, polycystic kidney disease, and acquired immune deficiency syndrome (AIDS) nephropathy. A variety of hereditary and environmental factors may contribute to the disease process as well.
The progression to end-stage renal disease (ESRD) begins with an initially asymptomatic stage known as “diminished kidney reserve.” This stage is characterized by a 10–20% decline in glomerular filtration rate (GFR) and a mildly elevated creatinine level. Diminished kidney reserve progresses to “renal insufficiency” where nitrogenous products begin to accumulate in the blood and the GFR continues to decline (20–50% of normal). “Renal failure” is the final stage of the disease process in which the kidney can no longer maintain its excretory, metabolic, and endocrine functions beyond the normal compensatory mechanisms. This stage involves multisystem organ involvement including endocrine, neuromuscular, cardiovascular, gastrointestinal, hematological, and dermatological manifestations.
Patients with kidney disease have a variety of metabolic abnormalities such as impaired excretory capacity, fluid and electrolyte imbalance, moderate-to-severe hypertension, anemia, bleeding problems, skeletal abnormalities, and altered drug metabolism. Medical management of kidney disease has improved considerably during the past decade. Presently, preventive health care is improving and conservative care is initiated as early in the progression of the disease as possible, with the goals to retard disease progression and preserve the patient’s quality of life. When kidney disease can no longer be treated by conservative medical management, dialysis is initiated, and if necessary, kidney transplantation is performed.1
Epidemiology
In the United States, more than 20 million people (10% of adults) have some form of CRF.2 The largest growth in the CRF population has occurred among Medicare patients.
The overall incident rate of ESRD has increased dramatically since 1992. Approximately 548,000 patients in the United States have irreversible ESRD, and the point prevalence rate is 1752 per 1 million U.S. residents.2 ESRD occurs more commonly in African-, Native, and Asian-Americans, and patients from ages 45–64 years. Specifically, African-Americans have the highest incident rates, at 982 per million population in 2002. Additionally, the rate of new ESRD cases remains higher for males than females. Treatment of ESRD patients in the United States in 2008 involved dialysis (382,343) or transplant (17,413), and numbers are predicted to increase in the future. Nearly 60,000 Americans die annually as a result of ESRD, most with cardiovascular complications.2
 Coordination of Care between Dentist and Physician
Coordination of Care between Dentist and Physician
Patients with kidney disease may have significant oral and dental complications, either directly related to kidney failure, from systemic complications arising from their kidney disease, or as untoward sequelae from various treatment modalities, including pharmacotherapy, dialysis, and/or transplant. Adequate pretreatment dental evaluation and dental treatment with proper consideration for the patient’s kidney status and related problems can prevent significant complications. Coordination of care between the dentist and physician cannot be overemphasized to ensure proper medical and dental care and overall health optimization, tailored to each individual patient.
 II. Medical Management
II. Medical Management
Most dentists will encounter CRF with more frequency in their patient population, but a general understanding of ARF is necessary for dentists who may be consulted to examine or treat a hospitalized patient undergoing treatment for ARF.
Identification
The National Kidney Foundation (NKF) defines CRF as either kidney damage for ≥3 months or a GFR of <60 mL/min/1.73 m2 for ≥3 months. CRF follows a predictable course and is categorized based on clinical and laboratory findings.3
- pathological abnormalities or
- markers of kidney damage, including abnormalities in the composition of the blood or urine or abnormalities in imaging tests
Medical History
In 2002, the Kidney Disease Outcome Quality Initiative (K/DOQI) of the NKF published clinical guidelines and a classification system for chronic kidney disease (CKD).3–5 Staging of the disease is based on the level of kidney function, regardless of the underlying etiology or disease process, and allows dentists and physicians to discuss kidney disease with more clarity than ever before. This also allows patients the opportunity to take greater control of their disease and understand their own progression when the classification is based on their GFR.3 See Table 5.1.
Table 5.1. NKF Classification of Chronic Kidney Disease and Clinical Features
Adapted from the National Kidney Foundation. Am J Kidney Dis 2002;39(Suppl. 1):S1–S266.
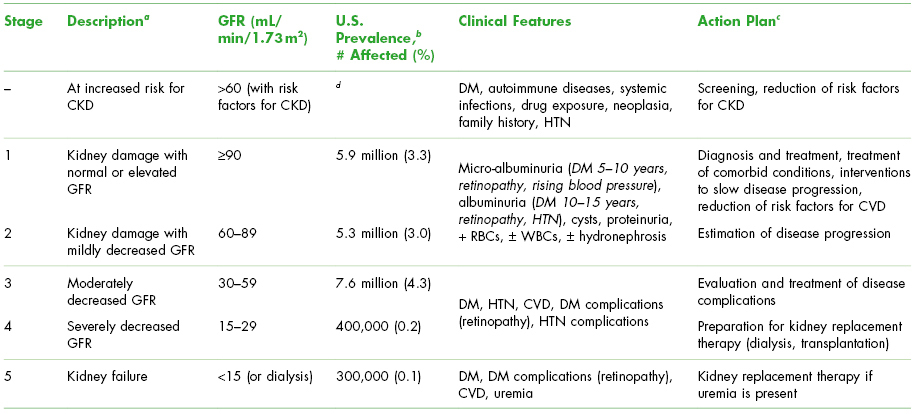
a For stages 1 and 2, kidney damage was estimated by a ratio of greater than 17 mg of albumin to 1 g of creatinine in men or greater than 25 mg of albumin to 1 g of creatinine in women on two untimed (spot) urine tests.
b Prevalence age ≥20 for stages 1 through 4 are based on data obtained from the Third National Health and Nutrition Examination Survey (1988–1994) (Sources: Jones CA et al. Am J Kidney Dis 1988;32(6):992–9; for stage 5, from the U.S. Renal Data Survey, NIDDK, 1998).
c Includes actions from preceding stages.
d Prevalence of persons at increased risk for CKD has not been estimated accurately.
NKF, National Kidney Foundation; GFR, glomerular filtration rate; CVD, cardiovascular disease; HTN, hypertension; DM, diabetes mellitus; RBCs, red blood cells; WBCs, white blood cells.
CKD, chronic kidney disease; defined as either kidney damage or a GFR <60 mL per minute per 1.73 m2 for ≥3 months. Kidney damage is defined as pathological abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies.
Patients with CKD require a complete medical evaluation to determine the specific type of kidney disease (diagnosis), comorbid conditions, severity of the disease (based on level of kidney function), risk for further loss of kidney function, and development of complications, either directly related to the loss of kidney function or from systemic organ involvement. K/DOQI also published guidelines for risk factors for CKD, treatment guidelines, and disease outcomes.2,6–8 Many of the susceptibility, initiation, progression, and end-stage factors can be determined through a thorough medical history and physical exam. Certain clinical and sociodemographic factors that have been implicated in the development and progression of CKD can be elicited during routine health-care visits. If these factors are present, further medical testing for the presence of albuminuria or diminished GFR should be performed.1
Physical Examination
Clinical manifestations of kidney disease and of uremia (excessive urea and other nitrogen compounds in the blood due to loss of kidney function) include nocturia, fatigue, altered mental status, peripheral neuropathy, nausea, vomiting, anorexia, and pruritis. Other common findings are hypertension, fluid and electrolyte abnormalities, anemia, and osteodystrophy. It is important to note that uremia is a serious medical syndrome, due in part to the various systemic complications that can develop. For example, uremic patients can have qualitative platelet abnormalities, may develop pericarditis, become encephalopathic with mental status changes, have immune suppression, and can develop a dermatological condition known as “uremic frost.”9,10 Many dentists may never encounter a patient with uremic syndrome since most patients with kidney failure undergo dialysis, prior to such manifestations.
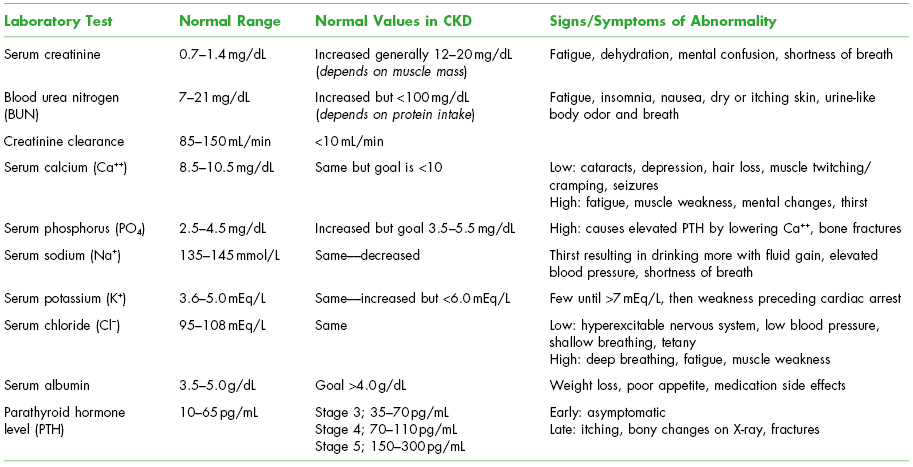
Laboratory Testing
Some general guidelines for medical assessment of the patient with kidney disease are listed below11,12:
- The degree of kidney function should be estimated by assessment of serum creatinine (the breakdown product of creatine phosphate in muscle that ends up in blood), creatinine clearance, BUN (BUN is the waste product of protein metabolism), and other factors. Progressive reduction in creatinine clearance is a direct reflection of diminishing renal capacity. The BUN level is also a reflection of renal function and increases during progressive renal failure. See Table 5.2.
- Patients with CKD usually have chronic anemia due to the inability of the kidney to produce sufficient erythropoietin (EPO) to stimulate bone marrow production of red blood cells. Patients may be taking iron, vitamin B12, and folic acid supplements, and EPO (Procrit®) injections thrice weekly to achieve a target hemoglobin of 10–12 g/dL. Hematocrit or hemoglobin should be measured before administering general anesthesia or intravenous sedation, before beginning dental procedures that might cause significant blood loss, or before prescribing narcotics.
- Patients with CKD usually have qualitative and quantitative platelet deficiencies. The platelet count, prothrombin time/international normalized ratio, and partial thromboplastin time should be measured before surgery.
- Hypertension is often associated with CKD. Blood pressure determination, before and during dental treatment, may be indicated and, when significantly elevated, appropriate medical referral should be considered.
- Abnormalities such as metabolic acidosis, fluid overload, and hyperkalemia can exist. Measurement of serum electrolytes and an electrocardiogram may be indicated prior to dental treatment. Elective dental treatment should be deferred when these abnormalities are present.
Table 5.2. Serum Chemistry Laboratory Changes in Chronic Kidney Disease (CKD)
Modified from Dialysis Lab Tests at a Glance. Available at: http://www.esrdnetworks.org.
Medical Treatment
Medical treatment for CKD begins with therapy for the specific underlying etiology; recognition and treatment of comorbid conditions; intervention to slow the loss of kidney function; measurements to prevent and treat cardiovascular disease and other systemic complications; and preparation for kidney failure and replacement of kidney function, by dialysis or transplantation if necessary.
First-line medical treatment may include angiotensin-converting enzyme (ACE) inhibitors to decrease the progression to kidney failure, in both diabetic and nondiabetic patients. Protein restriction has also been advocated as a preventive measure to slow the progression, once diagnosed with renal insufficiency. Other pharmacological agents employed in kidney disease include diuretics, potassium-binding resins to treat hyperkalemia, phosphate binders to prevent the development of renal osteodystrophy (elevated parathyroid hormone and subsequent calcium mobilization), sodium bicarbonate for acidosis, EPO for anemia, and fresh frozen plasma (FFP) or cryoprecipitate for bleeding diathesis.
CKD may progress to CRF, and thus, dialysis must be initiated to artificially filter the blood. This decision is usually made when the serum creatinine is chronically above 20 mg/dL, the creatinine clearance is below 20 mL/min, serum BUN is greater than 100 mg/dL, volume overload, refractory acidosis, and refractory hyperkalemia are present. The NKF guideline7 recommends discussion of options for treatment, including kidney transplantation, peritoneal dialysis (PD), hemodialysis (HD) in the home or in-center, and conservative treatment, when patients reach CKD stage 4 (estimated GFR <30 mL/min/1.73 m2) and initiation at least by stage 5 (estimated GFR <15 mL/min/1.73 m2). Over 382,000 patients receive dialysis in the United States at a cost of more than $39 billion dollars a year.2 Dialysis can be performed by either PD, HD, or, in the acute setting, continuous renal replacement therapy (CRRT):
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


