Bone Grafts and Bone Substitute Materials
At the conclusion of this chapter, the reader will be able to:
 . Understand the commonly used techniques for bone augmentation.
. Understand the commonly used techniques for bone augmentation.
 . Understand the advantages and disadvantages of various types of bone grafts.
. Understand the advantages and disadvantages of various types of bone grafts.
 . Discuss the limitations of nonautogenous grafts.
. Discuss the limitations of nonautogenous grafts.
 . Identify and manage complications associated with grafting.
. Identify and manage complications associated with grafting.
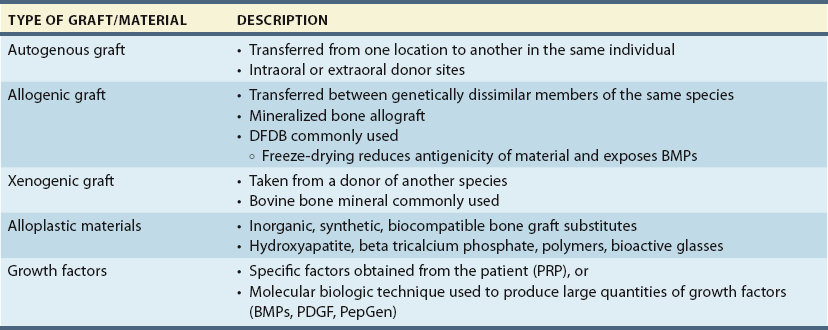
Alveolar defects resulting from loss of teeth or trauma often require bone augmentation before dental implants are placed. Attempting to place implants in locations with significant bone loss or lack of bone formation may lead to implant failure or a comprised position of the implant and patient dissatisfaction. The process of grafting involves a combination of biomaterials and clinical procedures, both of which affect the outcomes of the grafting procedure. Several types of grafts and materials are used for grafting (Table 5-1). These materials are classified in a general sense as autogenous (from the same person) or nonautogenous. Common surgical techniques include guided bone regeneration (GBR), onlay block grafting, and interpositional grafting. In choosing the technique or grafting material to use, the dental practitioner must evaluate characteristics such as the size and geometry of the anatomic location to be grafted.1
Overview of Different Types of Biomaterials
Autologous (or autogenous) bone is often referred to as the “gold standard” for regenerative and reconstructive procedures. However, performing a bone harvest, either intraorally or extraorally, may lead to significant morbidity for the patient. To overcome this problem, alternative materials have been developed; these materials are known collectively as biomaterials.2,3 Ideally, a biomaterial is able to:
Autogenous Bone
Features
The graft is harvested from the patient using either extraoral sites (e.g., the iliac crest or tibia) or intraoral donor sites (e.g., the mandibular symphysis, maxillary tuberosity, or mandibular ramus). The size of the defect helps determine which site is chosen. For isolated defects intraoral grafts have advantages over extraoral grafts, such as ease of access, proximity of the donor site and alveolar defect, ability to harvest in the office, decreased cost, and avoidance of morbidity associated with extraoral harvest sites.4,5
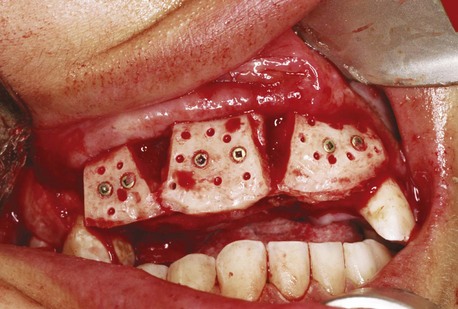
Cortical Bone Grafts
Cortical bone grafts are blocks composed predominantly of cortical bone. They provide a very dense, compact bone that offers great structural support. A cortical bone graft is suitable for reconstruction of both horizontal and vertical defects and is usually placed as a block graft secured with screws to the underlying ridge (Figure 5-1). This type of graft takes longer to revascularize than a cancellous graft.
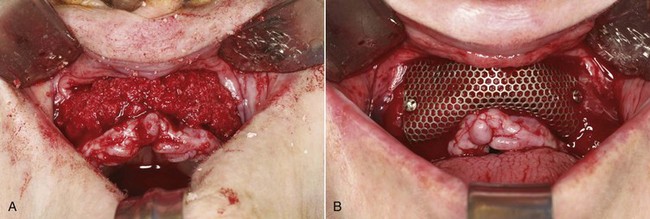
Cancellous (Particulate) Bone Grafts
The structure of cancellous bone allows rapid revascularization of the graft. It also reduces the number of cells that undergo necrosis, allowing more rapid neoangiogenesis, with early incorporation of the graft. These grafts often exhibit greater resorption than block grafts because of their lower density. A limitation of cancellous bone grafts is their instability immediately after placement. This type of graft requires a rigid biologic scaffold provided by barriers or walls of bone. Cancellous bone grafts are suitable for covering peri-implant osseous defects and periodontal fenestrations, for obtaining small alveolar reconstructions in GBR, for filling the spaces between cortical bone grafts, and for sinus lift and split-crest procedures (Figure 5-2).6
Donor Sites
The choice of the site for bone harvesting depends on the quantity and quality of bone needed to restore the proper morphology of the alveolar ridge. The choice also is influenced by the conditions at the recipient site, the patient’s expectations, and the dental practitioner’s capabilities and preferences. The available literature is a good reference source for determining specific sites according to an evidence-based approach to the grafting of various defects.7,8
Intraoral Donor Sites
Intraoral bone samples are indicated for reconstruction of bone defects that affect edentulous areas of one to three teeth or, alternatively, to provide enough bone to fill a sinus, because the amount of bone harvested is limited (Figure 5-3). A major advantage of an intraoral donor site is that the harvest site is close to the defect9,10; this translates into reduced operating and anesthesia time and often accelerated healing because of the rapidity of mucosal healing in the oral cavity. In addition to their reduced postoperative morbidity compared with extraoral sites (and the use of transcutaneous access), intraoral sites leave less scarring. Generally, this grafting procedure can be performed using local anesthesia or intravenous sedation, which reduces costs.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses