Chapter 3
Threats to Oral Health in Older Adults
Aim
The aim of this chapter is to outline potential threats to the ideal of retaining teeth for life. A further aim of this chapter is to describe how dentists and auxiliary staff can promote oral health in the older adult.
Outcome
The practitioner should be aware of the need to plan care for life, not just the short term. They should recognise that a number of conditions increase in prevalence in old age and threaten tooth survival. By planning care with this in mind, it is possible to maintain a natural, functioning dentition for life. At the end of this chapter, the practitioner should understand pathological conditions affecting the soft tissues that can occur in the older patient and how these may be prevented with vigilance and timely advice. The importance of health promotion by the dental team should also be recognised.
Factors Leading to Increased Tooth Retention by Older Adults
The improvement in tooth retention rate as reported in surveys of adult dental health could be attributed to a number of factors. These include:
-
improved awareness of oral health
-
improved access to dental care
-
oral health promotion by the dental profession
-
fluoridation of toothpastes
-
fluoridation from local (e.g. mouth rinses) and systemic (fluoridation of water supplies) sources.
The influence of fluoride on adult oral health is particularly dramatic in young and middle-aged adults and, as these cohorts age, tooth retention is likely to increase further.
Threats to Oral Health
There are many potential threats to oral health in older adults, and these are summarised in Fig 3-1.
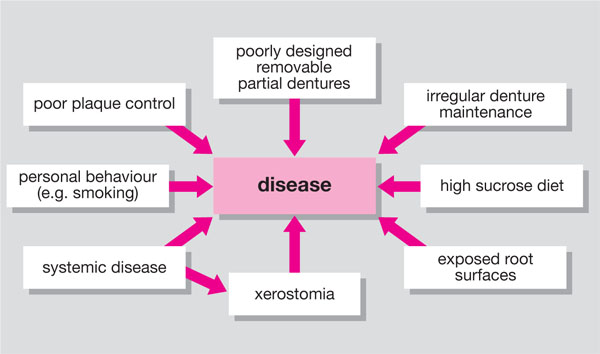
Fig. 3-1 Factors that threaten oral health in older adults.
Tooth retention
Whilst improvement is welcome, there are a number of significant threats to oral health in older adults. Many adults have teeth that have been heavily restored, and the burden of maintaining heavily restored dentitions will remain significant for many years. This factor, coupled with the tendency for older adults to find plaque control more difficult to maintain with age, poses a significant threat to the dentition of older adults. A further consideration is the reticence of older adults to attend a dentist on a regular basis, and this will require thought from policymakers in the future. In the past, older adults tended to accept deterioration of their teeth as an inevitable consequence of ageing. However, promotion of healthy ageing is now made more straightforward using mass communication media including the internet. Health promotion may also be facilitated by members of the dental team designated to undertake this process as part of the patient’s overall care. Finally, the importance of prevention cannot be overemphasised.
Common clinical problems in older adults that pose a threat to retention of teeth are:
-
Periodontal disease
-
Root caries
-
Tooth wear
-
Poorly designed removable prostheses
-
Systemic diseases.
Plaque control tends to diminish with age, mainly due to loss of manual dexterity. Periodontal disease is not an inevitable consequence of ageing, but the effects of cumulative periodontal attachment loss may become apparent in old age in patients susceptible to periodontal disease. Periodontal disease and the elderly will be described in greater detail in Chapter 4.
The prevalence of root caries is increasing as more adults retain teeth into old age. This is partly explained by the increased tooth retention by older adults and partly due to other environmental factors. Recession of the gingival tissues exposes the root-surface dentine and predisposes the patient to caries. This risk increases with the presence of RPDs, age and reduced salivary flow. The aetiology, diagnosis and treatment of root caries will be discussed in greater detail in Chapter 5.
Pathological (as opposed to normal physiological) tooth wear is a threat to the vitality of teeth. The prevalence of tooth wear in adults has increased, and this may be explained mostly by lifestyle and dietary changes that have taken place over the past 20 to 30 years. Management strategies for tooth wear in older adults are considered in more detail in Chapter 6.
RPDs that have been well designed, constructed and maintained pose minimal threat to oral health. However, many studies show that RPDs are associated with high levels of caries and periodontal disease. Plaque levels increase markedly in the presence of RPDs and, in the absence of meticulous plaque-control measures, oral disease can be the consequence. A particular problem is the tissue-supported acrylic denture commonly known as the “gum stripper”. This tissue-supported prosthesis (Fig 3-2) has been prescribed widely, mainly due to its low cost and ease of repair. A significant problem arises when these dentures are not maintained or regularly reviewed. As the underlying alveolar ridge resorbs, the denture sinks into the tissues. This in turn “strips” the gingival tissues, leading to exposure of the underlying root surfaces (Fig 3-3). Consequently, these types of prosthesis, especially in the lower jaw, can hasten the process of tooth loss.

Fig 3-2 Tissue-supported, free-end saddle removable partial denture. Note the sinking of the denture into the tissues. (Courtesy of Mr ID Murray)

Fig 3-3 Damage caused by poorly maintained tissue-supported free-end saddle removable partial denture. Note the inflamed gingival margins, exposure and carious lesions on root surfaces. (Courtesy of Mr ID Murray)
Tooth-supported dentures can also affect oral health. A common fault is to encroach upon the gingival tissues with components of the denture such as connectors and clasp tips (Fig 3-4). This in turn causes plaque accumulation and predisposes the patient to caries and gingival inflammation. However, when partial dentures are carefully designed, and plaque control is adequate, research indicates that it is possible to maintain good oral health in the presence of RPDs. When providing RPDs, prevention of disease can be aided by:
-
Providing tooth support for the denture where possible. In cobalt-chromium-based dentures, rests should be placed on the tooth surfaces adjacent to the saddles. Wrought rests can be incorporated into acrylic-based RPDs to provide tooth support.
-
Minimising coverage of the dental and gingival tissues. Essentially, keep the design of the RPD as simple as possible. The connector should not encroach on the gingival margins of the teeth, and clasps should not cover exposed root surfaces. Every design of acrylic dentures can be provided in the maxilla (Fig3-5).
-
Carefully instructing the patient in cleaning techniques for both RPD and the natural teeth. This includes careful instruction in oral-hygiene procedures, encouraging the patient to clean the denture after meals and to use denture cleaners.
-
Arranging regular inspection visits and checking the fit of the RPD to ensure that it is not causing damage. The frequency of these inspection visits depends on the individual patient, but at least one inspection visit per year is recommended.

Fig 3-4 Extensive coverage of the denture-bearing tissues with the major connector of the denture. This is likely to damage the tissues, particularly the gingival margins.
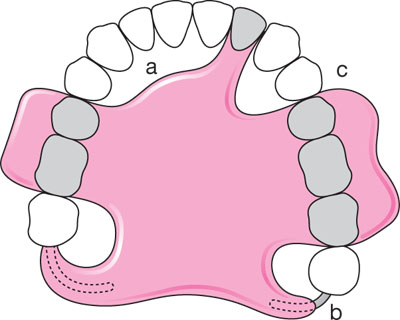
Fig 3-5 Design features of Every style acrylic removable partial denture. The key features of this design are: (a) relief of the connector from the standing teeth; (b) wrought clasps engaging the distal surface of the last standing teeth; (c) good proximal contact with natural teeth.
A number of systemic diseases impact on the oral health of older adults. These can affect the intraoral environment or cause extraoral changes (e.g. arthritis of the hands) that make oral hygiene procedures difficult. Patients with arthritic conditions (Fig 3-6) affecting the hands often require specially modified toothbrushes to facilitate plaque removal. Some medications cause xerostomia (dry mouth) and thus the buffering capacity of saliva is dramatically altered. Examples of medications commonly prescribed for the elderly that may cause dry mouth are shown in Table 3-1. Whilst this table is not exhaustive, it can be seen that dry mouth is a common side-effect of these medications, and the reader is referred to the British National Formulary for a more comprehensive listing of drugs with oral side-effects.

Fig 3-6 Patient with rheumatoid arthritis affecting her fingers. This patien/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


