SPECIFIC PROBLEM AREAS
ACROMEGALY
General aspects
Aetiopathogenesis
Clinical presentation
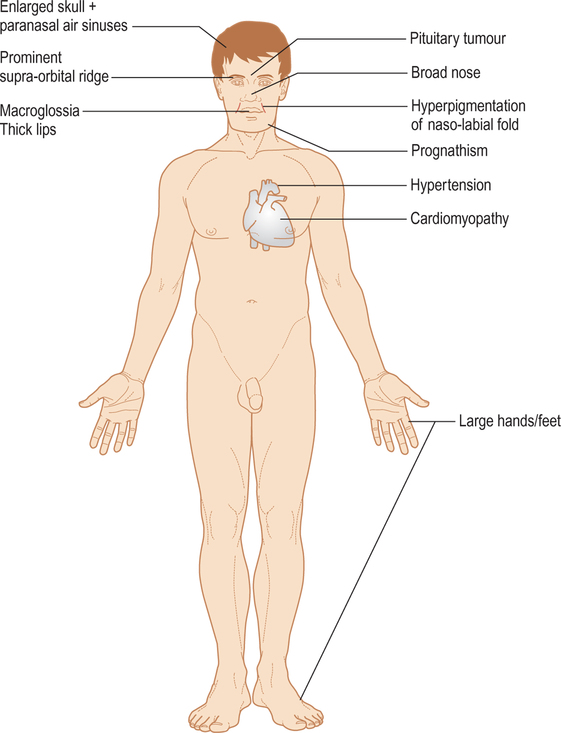
 Excess tissue growth (Fig. 3.1): • supra-orbital ridge (prominent) • nose (broadened) • skin (thickening) • macroglossia • mandible (spaced teeth, prognathism) • hands and feet (large)
Excess tissue growth (Fig. 3.1): • supra-orbital ridge (prominent) • nose (broadened) • skin (thickening) • macroglossia • mandible (spaced teeth, prognathism) • hands and feet (large)  Systemic complications due to organ enlargement: • diabetes • hypertension • cardiomyopathy
Systemic complications due to organ enlargement: • diabetes • hypertension • cardiomyopathy  Local effects of pituitary tumour (headache, visual defects).
Local effects of pituitary tumour (headache, visual defects).
Dental management
Risk assessment
Pain and anxiety control
General anaesthesia
Table 3.1
Key considerations for dental management in acromegaly (see text)
| Management modifications* | Comments/possible complications | |
| Risk assessment | 2 | Blindness, diabetes, hypertension, arrhythmias |
| Preventive dentistry and education | 1 | Carpal tunnel syndrome, enlarged tongue |
| Pain and anxiety control | ||
| – Local anaesthesia | 0 | |
| – Conscious sedation | 0 | |
| – General anaesthesia | 1/4 | Kyphosis, narrow glottis |
| Patient access and positioning | ||
| – Access to dental office | 0 | |
| – Timing of treatment | 1 | Sleep apnoea, fatigue |
| – Patient positioning | 1 | Longer dental chair |
| Treatment modification | ||
| – Oral surgery | 0 | |
| – Implantology | 0 | |
| – Conservative/Endodontics | 0 | |
| – Fixed prosthetics | 0 | |
| – Removable prosthetics | 0 | |
| – Non-surgical periodontology | 0 | |
| – Surgical periodontology | 0 | |
| Hazardous and contraindicated drugs | 0 |
*0 = No special considerations. 1 = Caution advised. 2 = Specialised medical advice recommended in some cases. 3 = Specialised medical advice mandatory. 4 = Only to be performed in hospital environment. 5 = Should be avoided.
ADDISON’S DISEASE
General aspects
Aetiopathogenesis
Clinical presentation
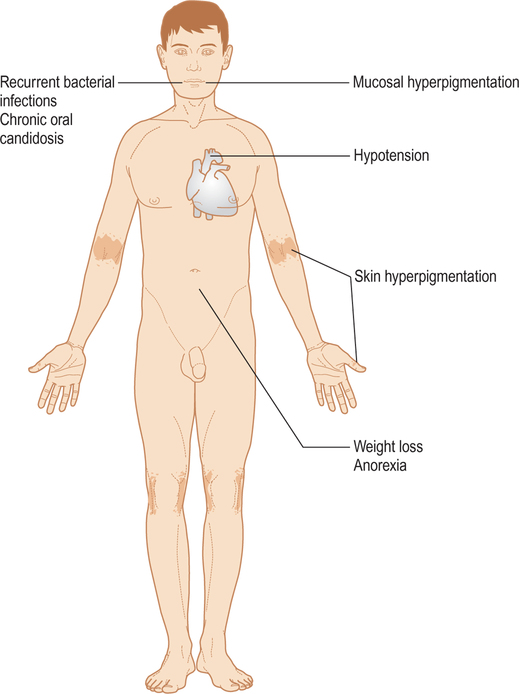
 Low cortisol leads to: • skin and mucosal hyperpigmentation (due to raised ACTH in primary disease; part of ACTH molecule is similar to melanocyte stimulating hormone) (Fig. 3.2) • hypotension (weakness, lethargy, tiredness, collapse) • weight loss
Low cortisol leads to: • skin and mucosal hyperpigmentation (due to raised ACTH in primary disease; part of ACTH molecule is similar to melanocyte stimulating hormone) (Fig. 3.2) • hypotension (weakness, lethargy, tiredness, collapse) • weight loss  Adrenocortical hypofunction may lead to shock and death if the individual is stressed as, for example, by an operation, infection or trauma.
Adrenocortical hypofunction may lead to shock and death if the individual is stressed as, for example, by an operation, infection or trauma.
Dental management
Risk assessment
Treatment modification
Surgery
Table 3.2
Key considerations for dental management in Addison’s disease (see text)
| Management modifications* | Comments/possible complications | |
| Risk assessment | 2 | Acute adrenal insufficiency |
| Appropriate oral health care | 2 | Consider steroid cover |
| Preventive dentistry | 1 | Increased susceptibility to infection |
| Pain and anxiety control | ||
| – Local anaesthesia | 0 | |
| – Conscious sedation | 0 | |
| – General anaesthesia | 2/4 | ACTH and cortisol secretion |
| Patient access and positioning | ||
| – Access to dental office | 0 | |
| – Timing of treatment | 1 | Early morning |
| – Patient positioning | 0 | |
| Treatment modification | ||
| – Oral surgery | 1 | Delayed healing |
| – Implantology | 1 | Delayed healing |
| – Conservative/Endodontics | 0 | |
| – Fixed prosthetics | 0 | |
| – Removable prosthetics | 0 | |
| – Non-surgical periodontology | 0 | |
| – Surgical periodontology | 1 | Delayed healing |
| Hazardous and contraindicated drugs | 0 |
*0 = No special considerations. 1 = Caution advised. 2 = Specialised medical advice recommended in some cases. 3 = Specialised medical advice mandatory. 4 = Only to be performed in hospital environment. 5 = Should be avoided.
ALCOHOLISM
General aspects
Aetiopathogenesis
Clinical presentation
 Alcohol at blood levels above 35 mg/dL (35 mg/100 mL) impairs judgment, while signs of intoxication are clinically obvious at a blood alcohol level above 100 mg/dL, with slurred speech, loss of restraint and ataxia. At a blood alcohol level above 200 mg/dL some people become aggressive.
Alcohol at blood levels above 35 mg/dL (35 mg/100 mL) impairs judgment, while signs of intoxication are clinically obvious at a blood alcohol level above 100 mg/dL, with slurred speech, loss of restraint and ataxia. At a blood alcohol level above 200 mg/dL some people become aggressive.  Thus the acute effects of alcohol are mainly on judgment, concentration and coordination, and are dose-related as shown in Table 3.3
Thus the acute effects of alcohol are mainly on judgment, concentration and coordination, and are dose-related as shown in Table 3.3  Earlier signs or symptoms of chronic excessive alcohol drinking include an evasive, truculent, over-boisterous or facetious manner, slurred speech, smell of alcohol on the breath, signs of self-neglect, gastric discomfort (particularly heartburn), anxiety (often with insomnia), or tremor
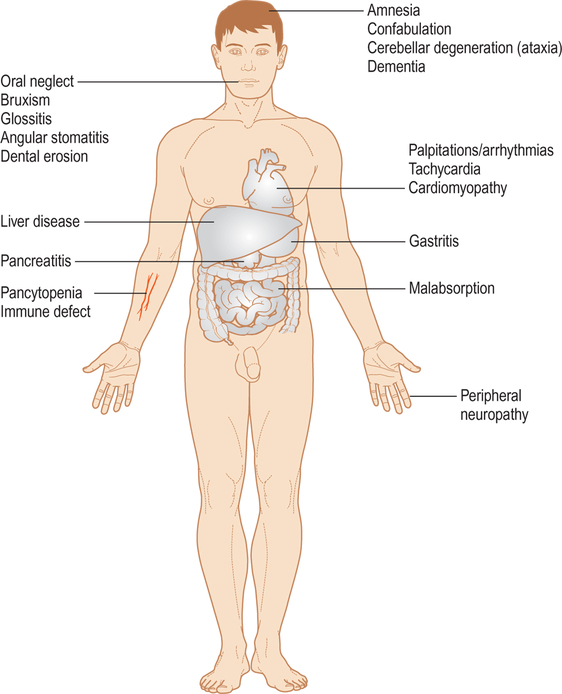
Earlier signs or symptoms of chronic excessive alcohol drinking include an evasive, truculent, over-boisterous or facetious manner, slurred speech, smell of alcohol on the breath, signs of self-neglect, gastric discomfort (particularly heartburn), anxiety (often with insomnia), or tremor  Later signs or symptoms of chronic excessive alcohol drinking include palpitations and tachycardia, cardiomyopathy, liver disease, malnutrition, peripheral neuropathy, amnesia and confabulation (in Wernicke’s and Korsakoff’s CNS syndromes), cerebellar degeneration with ataxia, or dementia (Fig. 3.3, Table 3.4)
Later signs or symptoms of chronic excessive alcohol drinking include palpitations and tachycardia, cardiomyopathy, liver disease, malnutrition, peripheral neuropathy, amnesia and confabulation (in Wernicke’s and Korsakoff’s CNS syndromes), cerebellar degeneration with ataxia, or dementia (Fig. 3.3, Table 3.4)  Alcohol can interact with other drugs such as warfarin, paracetamol/acetaminophen, and CNS-active agents such as benzodiazepines.
Alcohol can interact with other drugs such as warfarin, paracetamol/acetaminophen, and CNS-active agents such as benzodiazepines.
Table 3.3
| Blood alcohol level in mg/dL | Effect |
| <100 | Dry and decent |
| 100–200 | Delighted and devilish |
| 200–300 | Delinquent and disgusting |
| 300–400 | Dizzy and delirious |
| 400–500 | Dazed and dejected |
| >500 | Dead drunk |
Table 3.4
| Possible effects | Biochemical changes | |
| Cardiac | Cardiomyopathy, arrhythmias | |
| CNS | Intoxication | Raised blood alcohol |
| Dementia | Decreased thiamine levels | |
| Wernicke–Korsakoff syndrome | ||
| Gastric | Gastritis | |
| Haematological | Pancytopenia | Reduced haemoglobin |
| Immune defect | Reduced platelet count | |
| Leukopenia | ||
| Macrocytosis | ||
| Reduced blood clotting factors II, VII, IX, X | ||
| Hepatic | Hepatitis | Raised gamma glutamyl |
| Fatty liver (steatosis) | transpeptidase | |
| Cirrhosis | Raised other liver enzymes | |
| Raised bilirubin | ||
| Reduced albumin | ||
| Intestinal | Malabsorption of glucose and vitamins | Reduced folate, thiamine and vitamins B12, A, D, E and K |
| Oesophageal | Gastro-oesophageal reflux disease | |
| Mallory–Weiss syndrome (tears from vomiting) | ||
| Pancreatic | Pancreatitis | Raised serum amylase |
Dental management
Risk assessment
Treatment modification
Surgery
Table 3.5
Key considerations for dental management in alcoholism (see text)
| Management modifications* | Comments/possible complications | |
| Risk assessment | 2 | Liver cirrhosis, consent |
| Preventive dentistry and education | 1 | Alcoholism screening, oral cancer screening and diet counselling |
| Pain and anxiety control | ||
| – Local anaesthesia | 1 | Tolerance |
| – Conscious sedation | 1 | Additive effect |
| – General anaesthesia | 5 | Resistance, aspiration |
| Patient access and positioning | ||
| – Access to dental office | 0 | |
| – Timing of treatment | 1 | Morning |
| – Patient positioning | 0 | |
| Treatment modification | ||
| – Oral surgery | 1 | Bleeding tendency |
| – Implantology | 5 | Poor risk group |
| – Conservative/Endodontics | 1 | Maintenance compromised |
| – Fixed prosthetics | 1 | Maintenance compromised |
| – Removable prosthetics | 0 | |
| – Non-surgical periodontology | 1 | Maintenance compromised |
| – Surgical periodontology | 1 | Bleeding tendency |
| Hazardous and contraindicated drugs | 2 | Sedatives, NSAIDs, metronidazole, cephalosporins |
*0 = No special considerations. 1 = Caution advised. 2 = Specialised medical advice recommended in some cases. 3 = Specialised medical advice mandatory. 4 = Only to be performed in hospital environment. 5 = Should be avoided.
ALZHEIMER’S DISEASE
General aspects
 Dementia is a chronic organic brain disease characterised by amnesia (especially for recent events), inability to concentrate, disorientation in time, place or person and intellectual impairment (including loss of normal social awareness)
Dementia is a chronic organic brain disease characterised by amnesia (especially for recent events), inability to concentrate, disorientation in time, place or person and intellectual impairment (including loss of normal social awareness)  It has many causes (Table 3.6), the most common being: • Alzheimer’s disease • multi-infarct (vascular) dementia • Lewy body dementia
It has many causes (Table 3.6), the most common being: • Alzheimer’s disease • multi-infarct (vascular) dementia • Lewy body dementia  Dementia is usually seen in old age, and may be mimicked by acute organic brain disease, confusional states, drug-induced disorders and psychiatric disease.
Dementia is usually seen in old age, and may be mimicked by acute organic brain disease, confusional states, drug-induced disorders and psychiatric disease.
Table 3.6
| Common causes | Uncommon causes |
| Alcoholism | AIDS |
| Alzheimer’s disease (>60% of all dementia) | Brain trauma, haemorrhage or infection |
| Cortical Lewy body dementia (10%) | Creutzfeldt–Jakob disease |
| Huntington’s chorea | Metabolic causes (e.g. hypothyroidism) |
| Hydrocephalus | Pick’s disease (frontal lobar atrophy) |
| Multi-infarct dementia (25%) | |
| Tumours |
Dental management
Treatment modification
Table 3.7
Key considerations for dental management in Alzheimer’s disease (see text)
| Management modifications* | Comments/possible complications | |
| Risk assessment | 2 | Behaviour control; other systemic diseases; consent |
| Preventive dentistry | 1 | Electric toothbrushing; chlorhexidine |
| Pain and anxiety control | ||
| – Local anaesthesia | 1 | Behaviour control; |
| – Conscious sedation | 1 | other systemic diseases |
| – General anaesthesia | 3/4 | |
| Patient access and positioning | ||
| – Access to dental office | 1 | Hip fracture |
| – Timing of treatment | 1 | Morning; carer present |
| – Patient positioning | 1 | Sitting upright |
| Treatment modification | ||
| – Oral surgery | 1 | |
| – Implantology | 5 | Poor oral hygiene |
| – Conservative/Endodontics | 1 | Single procedures |
| – Fixed prosthetics | 1 | Single procedures, early stages |
| – Removable prosthetics | 1/5 | Lost, broken, poorly tolerated |
| – Non-surgical periodontology | 1 | |
| – Surgical periodontology | 1 | |
| Hazardous and contraindicated drugs | 2 | Tolerance of sedatives |
*0 = No special considerations. 1 = Caution advised. 2 = Specialised medical advice recommended in some cases. 3 = Specialised medical advice mandatory. 4 = Only to be performed in hospital environment. 5 = Should be avoided.
AMPHETAMINE, LSD AND ECSTASY ABUSE
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 plasma GH – raised
plasma GH – raised  oral glucose tolerance test – fails to suppress GH
oral glucose tolerance test – fails to suppress GH  serum insulin-like growth factor 1 – raised
serum insulin-like growth factor 1 – raised  CT and MRI.
CT and MRI. Neurosurgery and/or radiation
Neurosurgery and/or radiation  Dopamine agonists (bromocriptine) and somatostatin analogues (sandostatin).
Dopamine agonists (bromocriptine) and somatostatin analogues (sandostatin). The skull is thickened and the paranasal air sinuses are enlarged
The skull is thickened and the paranasal air sinuses are enlarged  Mandibular enlargement leads to class III malocclusion with spacing of the teeth and thickening of all soft tissues, but most conspicuously of the face
Mandibular enlargement leads to class III malocclusion with spacing of the teeth and thickening of all soft tissues, but most conspicuously of the face  Enlargement of the dental bases leads to relatively sudden ill-fitting dentures
Enlargement of the dental bases leads to relatively sudden ill-fitting dentures  Macroglossia and thick lips are due to soft tissue growth
Macroglossia and thick lips are due to soft tissue growth Apical hypercementosis
Apical hypercementosis  Sialosis
Sialosis  Hyperpigmentation of the naso-labial fold
Hyperpigmentation of the naso-labial fold  Progressive periodontal disease has been described – probably related to dental malposition and tissue enlargement.
Progressive periodontal disease has been described – probably related to dental malposition and tissue enlargement. visual impairment
visual impairment  cardiomyopathy
cardiomyopathy  cardiac arrhythmias
cardiac arrhythmias  hypertension
hypertension  diabetes mellitus
diabetes mellitus  hypopituitarism.
hypopituitarism. primary – occurs when at least 90% of the adrenal cortex has been destroyed, and leads to low levels of both cortisol and aldosterone
primary – occurs when at least 90% of the adrenal cortex has been destroyed, and leads to low levels of both cortisol and aldosterone  secondary – due to low levels of adrenocorticotrophic hormone (ACTH), which causes a drop in the adrenal glands’ production of cortisol but not aldosterone.
secondary – due to low levels of adrenocorticotrophic hormone (ACTH), which causes a drop in the adrenal glands’ production of cortisol but not aldosterone. Main cause is autoimmune (sometimes also associated with diabetes, Graves’ disease, pernicious anaemia, vitiligo or hypoparathyroidism), particularly in women
Main cause is autoimmune (sometimes also associated with diabetes, Graves’ disease, pernicious anaemia, vitiligo or hypoparathyroidism), particularly in women  Rare causes include adrenal tuberculosis, histoplasmosis or tumours
Rare causes include adrenal tuberculosis, histoplasmosis or tumours  Secondary adrenocortical hypofunction may also follow an abrupt withdrawal from systemic corticosteroid therapy.
Secondary adrenocortical hypofunction may also follow an abrupt withdrawal from systemic corticosteroid therapy. Postural hypotension
Postural hypotension  Plasma cortisol level – low
Plasma cortisol level – low  Plasma sodium – low
Plasma sodium – low  Plasma potassium – high
Plasma potassium – high  ACTH stimulation test – impaired
ACTH stimulation test – impaired  Adrenal antibodies.
Adrenal antibodies. Glucocorticoids (cortisone or cortisol) and mineralocorticoids (fludrocortisone).
Glucocorticoids (cortisone or cortisol) and mineralocorticoids (fludrocortisone). Pigmentation of the mucosae of a brown or black colour is seen in over 75% of patients with Addison’s disease. Hyperpigmentation predominantly affects areas that are normally pigmented or exposed to trauma (for example in the buccal mucosa at the occlusal line, or the tongue, and occasionally, the gingivae).
Pigmentation of the mucosae of a brown or black colour is seen in over 75% of patients with Addison’s disease. Hyperpigmentation predominantly affects areas that are normally pigmented or exposed to trauma (for example in the buccal mucosa at the occlusal line, or the tongue, and occasionally, the gingivae).  Recurrent bacterial oral infections are not uncommon
Recurrent bacterial oral infections are not uncommon  Chronic oral candidosis has also been described where there is an associated immune defect.
Chronic oral candidosis has also been described where there is an associated immune defect. call for immediate help
call for immediate help  lay patient flat with legs raised
lay patient flat with legs raised  give hydrocortisone 200 mg IM
give hydrocortisone 200 mg IM  oxygen 10L/min
oxygen 10L/min  if IV access can be obtained, give 1 litre dextrose saline
if IV access can be obtained, give 1 litre dextrose saline  check blood pressure.
check blood pressure.

 CNS – memory loss, disinhibition
CNS – memory loss, disinhibition  liver – fatty liver, alcoholic hepatitis, cirrhosis
liver – fatty liver, alcoholic hepatitis, cirrhosis  GIT – gastritis, peptic ulcer, pancreatitis
GIT – gastritis, peptic ulcer, pancreatitis  heart – cardiomyopathy, hypertension.
heart – cardiomyopathy, hypertension. Gamma glutamyl transpeptidase increased
Gamma glutamyl transpeptidase increased  Complete blood count (macrocytosis often without anaemia)
Complete blood count (macrocytosis often without anaemia)  Blood alcohol levels raised.
Blood alcohol levels raised. Cognitive therapy
Cognitive therapy  Naltrexone
Naltrexone  Acamprosate
Acamprosate  High-protein, high-calorie and low-sodium diet (± vitamin supplementation).
High-protein, high-calorie and low-sodium diet (± vitamin supplementation). Mortality related to alcoholic hepatitis diagnosis is 10-25%, and life quality and expectancy can be affected by diseases including: • liver disease, especially alcohol-induced hepatitis and cirrhosis • nutritional defects • pancreatitis • gastritis and peptic ulcer • immune defects leading to infections, especially pneumonia and tuberculosis, and impaired wound
Mortality related to alcoholic hepatitis diagnosis is 10-25%, and life quality and expectancy can be affected by diseases including: • liver disease, especially alcohol-induced hepatitis and cirrhosis • nutritional defects • pancreatitis • gastritis and peptic ulcer • immune defects leading to infections, especially pneumonia and tuberculosis, and impaired wound Social difficulties from alcohol misuse can affect the six “Ls”: • law – breach of the criminal, civil and/or professional codes • learning – intellectual difficulties • livelihood – job problems • living – housing problems • lover – interpersonal difficulties of all kinds, husband/wife, partner, employer/employee etc. • lucre (Latin – lucrum = wealth) – money problems.
Social difficulties from alcohol misuse can affect the six “Ls”: • law – breach of the criminal, civil and/or professional codes • learning – intellectual difficulties • livelihood – job problems • living – housing problems • lover – interpersonal difficulties of all kinds, husband/wife, partner, employer/employee etc. • lucre (Latin – lucrum = wealth) – money problems. The most common oral effect of alcoholism is neglect, leading to advanced caries and periodontal disease
The most common oral effect of alcoholism is neglect, leading to advanced caries and periodontal disease  Dental erosion may result from regurgitation
Dental erosion may result from regurgitation  Nocturnal bruxism by reticular system stimulation is common, and may predispose to temporomandibular joint disorders
Nocturnal bruxism by reticular system stimulation is common, and may predispose to temporomandibular joint disorders  If there is deficiency of folate or other B complex vitamins (niacin, piridoxine, riboflavine or thiamine), sore mouth, recurrent aphthae, glossitis, dysgeusia, tongue depapillation, dysaesthesia and angular stomatitis may result
If there is deficiency of folate or other B complex vitamins (niacin, piridoxine, riboflavine or thiamine), sore mouth, recurrent aphthae, glossitis, dysgeusia, tongue depapillation, dysaesthesia and angular stomatitis may result  Painless, bilateral, parotid gland enlargement due to fat infiltration (sialosis) is frequent in patients with alcoholic cirrhosis
Painless, bilateral, parotid gland enlargement due to fat infiltration (sialosis) is frequent in patients with alcoholic cirrhosis  Other orofacial features include a smell of alcohol on the breath, telangiectases and possibly rhinophyma (enlargement of the nose with dilation of follicles and redness and prominent vascularity of the skin, also known as “grog blossom”).
Other orofacial features include a smell of alcohol on the breath, telangiectases and possibly rhinophyma (enlargement of the nose with dilation of follicles and redness and prominent vascularity of the skin, also known as “grog blossom”). Dentists should screen for alcohol abuse by recognising characteristic clinical and laboratory findings and behavioural disturbances
Dentists should screen for alcohol abuse by recognising characteristic clinical and laboratory findings and behavioural disturbances  Alcohol is a known risk factor for oral cancer development, thus a periodical examination for detection of suspicious soft-tissue lesions is mandatory
Alcohol is a known risk factor for oral cancer development, thus a periodical examination for detection of suspicious soft-tissue lesions is mandatory  Dentists should provide specific preventive information to patients with alcoholism and refer them to health care providers for assessment or treatment
Dentists should provide specific preventive information to patients with alcoholism and refer them to health care providers for assessment or treatment  Oral health care advice should be given
Oral health care advice should be given  Diet counselling should be provided.
Diet counselling should be provided. Diazepam, lorazepam and other sedatives increase CNS depression
Diazepam, lorazepam and other sedatives increase CNS depression  Aspirin should be avoided since it is more likely in the alcoholic patient to cause gastric erosions and bleeding, and to precipitate bleeding. The hepatotoxic effects of acetaminophen/paracetamol are enhanced, although it is still probably the safest analgesic in this group, and may be used in reduced dosage.
Aspirin should be avoided since it is more likely in the alcoholic patient to cause gastric erosions and bleeding, and to precipitate bleeding. The hepatotoxic effects of acetaminophen/paracetamol are enhanced, although it is still probably the safest analgesic in this group, and may be used in reduced dosage.  Metronidazole and cephalosporins can interact with alcohol to cause widespread vasodilatation, nausea, vomiting, sweating, headache and palpitations similar to the antabuse reaction (disulfiram effect). The effects are unpleasant or alarming but rarely dangerous.
Metronidazole and cephalosporins can interact with alcohol to cause widespread vasodilatation, nausea, vomiting, sweating, headache and palpitations similar to the antabuse reaction (disulfiram effect). The effects are unpleasant or alarming but rarely dangerous. gene defects (20% of cases)
gene defects (20% of cases)  apolipoprotein-Epsilon 4 (apoE4)
apolipoprotein-Epsilon 4 (apoE4)  insulin resistance
insulin resistance  herpes virus infection
herpes virus infection  others (cerebral ischaemia, immunological disturbances, etc).
others (cerebral ischaemia, immunological disturbances, etc). First stage: • memory loss • disorientation in time and place • judgment impaired • lack of spontaneity • poor appearance
First stage: • memory loss • disorientation in time and place • judgment impaired • lack of spontaneity • poor appearance  Second stage: • loss of intellect • aphasia • inability to feed or clothe self • acquired defects of visual–spatial skill
Second stage: • loss of intellect • aphasia • inability to feed or clothe self • acquired defects of visual–spatial skill  Third stage: • apathy and mutism • inability to communicate • anxiety, depression, irritability • hyperorality • hyper-reflexia • absolute dependence • disruptive behaviour may be present.
Third stage: • apathy and mutism • inability to communicate • anxiety, depression, irritability • hyperorality • hyper-reflexia • absolute dependence • disruptive behaviour may be present. History and clinical findings: • development of multiple cognitive disturbances • memory impairment • problems with language (aphasia), motor activities (apraxia), recognition (agnosia), planning, organisation
History and clinical findings: • development of multiple cognitive disturbances • memory impairment • problems with language (aphasia), motor activities (apraxia), recognition (agnosia), planning, organisation  Neuropsychiatric tests
Neuropsychiatric tests  Neuroimaging (cortical atrophy and ventricular enlargement).
Neuroimaging (cortical atrophy and ventricular enlargement). Rivastigmine
Rivastigmine  Donepezil
Donepezil  Galantamine
Galantamine  Aspirin and gingko biloba may delay onset.
Aspirin and gingko biloba may delay onset. Oral hygiene neglect typically increases with Alzheimer’s disease progression
Oral hygiene neglect typically increases with Alzheimer’s disease progression  Xerostomia, due to poor saliva production and drugs (phenothiazines), gives rise to candidosis, cervical caries and prosthesis intolerance
Xerostomia, due to poor saliva production and drugs (phenothiazines), gives rise to candidosis, cervical caries and prosthesis intolerance  Periodontal disease is common, as is halitosis
Periodontal disease is common, as is halitosis  Loss of taste
Loss of taste  Depapillated, red, dry, fissured tongue
Depapillated, red, dry, fissured tongue  Trauma due to apraxia is not unusual, and may present with: • maxillofacial injuries • traumatic oral ulcers • missing and broken teeth • attrition • severe alveolar ridge atrophy secondary to ill-fitting dentures
Trauma due to apraxia is not unusual, and may present with: • maxillofacial injuries • traumatic oral ulcers • missing and broken teeth • attrition • severe alveolar ridge atrophy secondary to ill-fitting dentures  Oral dyskinesia due to antipsychotic medication.
Oral dyskinesia due to antipsychotic medication. Dextroamphetamine (amphetamine) and methylphenidate are the most representative drugs. Stimulants are prescribed for treating only a few health conditions, including narcolepsy, attention-deficit hyperactivity disorder, and deep depression. Amphetamines are misused or abused for their euphoriant effect, to stave off fatigue in order to continue working and for slimming.
Dextroamphetamine (amphetamine) and methylphenidate are the most representative drugs. Stimulants are prescribed for treating only a few health conditions, including narcolepsy, attention-deficit hyperactivity disorder, and deep depression. Amphetamines are misused or abused for their euphoriant effect, to stave off fatigue in order to continue working and for slimming.  LSD (lysergic acid diethylamide), manufactured from lysergic acid (found in ergot, a fungus that grows on rye and other grains), is a major hallucinogen, considered one of the most potent mood-changing chemicals
LSD (lysergic acid diethylamide), manufactured from lysergic acid (found in ergot, a fungus that grows on rye and other grains), is a major hallucinogen, considered one of the most potent mood-changing chemicals  MDMA (3,4-methylenedioxymethamphetamine), popularly known as “ecstasy”, is a synthetic, psychoactive drug with sympathomimetic properties, and both stimulant (amphetamine-like) and hallucinogenic (LSD-like) properties.
MDMA (3,4-methylenedioxymethamphetamine), popularly known as “ecstasy”, is a synthetic, psychoactive drug with sympathomimetic properties, and both stimulant (amphetamine-like) and hallucinogenic (LSD-like) properties. These are the main drugs in a group of central stimulants which also includes phenmetrazine, methylphenidate and, to a lesser extent, diethylpropion. They produce a range of effects by stimulating alpha- and beta-adrenergic receptors, increasing the levels of monoamines (which include norepinephrine and dopamine) and thus stimulating the CNS and peripheral nervous system.
These are the main drugs in a group of central stimulants which also includes phenmetrazine, methylphenidate and, to a lesser extent, diethylpropion. They produce a range of effects by stimulating alpha- and beta-adrenergic receptors, increasing the levels of monoamines (which include norepinephrine and dopamine) and thus stimulating the CNS and peripheral nervous system.  Acute amphetamine toxicity causes dry mouth, dilated pupils, tachycardia, aggression, talkativeness, tachypnoea and hallucinations, leading to seizures, hypertension, hyperpyrexia, arrhythmias and collapse
Acute amphetamine toxicity causes dry mouth, dilated pupils, tachycardia, aggression, talkativeness, tachypnoea and hallucinations, leading to seizures, hypertension, hyperpyrexia, arrhythmias and collapse  Chronic amphetamine toxicity causes restlessness, hyperactivity, loss of appetite and weight, tremor, repetitive movements, bruxism and picking at the face and extremities
Chronic amphetamine toxicity causes restlessness, hyperactivity, loss of appetite and weight, tremor, repetitive movements, bruxism and picking at the face and extremities  High doses of amphetamines can cause mood swings and psychoses (including hallucinations and paranoia), and can cause respiratory failure and death
High doses of amphetamines can cause mood swings and psychoses (including hallucinations and paranoia), and can cause respiratory failure and death  Combining use with other drugs such as alcohol can result in nausea, difficulty breathing and unconsciousness.
Combining use with other drugs such as alcohol can result in nausea, difficulty breathing and unconsciousness. The effects of LSD are unpredictable but prolonged (∼12h), depending on the amount taken, the user’s personality, mood, and expectations, and the surroundings in which the drug is used
The effects of LSD are unpredictable but prolonged (∼12h), depending on the amount taken, the user’s personality, mood, and expectations, and the surroundings in which the drug is used  Typically, LSD produces several different emotions at once or users swing rapidly from one emotion to another within 30-90 minutes. Synaesthesia, the overflow from one sense to another when, for example, colours are heard, is common. There is often lability of mood, panic (“bad trip”) and delusions of magical powers, such as being able to fly. If taken in a large enough dose, the drug produces delusions and visual hallucinations. The user’s sense of time and self changes.
Typically, LSD produces several different emotions at once or users swing rapidly from one emotion to another within 30-90 minutes. Synaesthesia, the overflow from one sense to another when, for example, colours are heard, is common. There is often lability of mood, panic (“bad trip”) and delusions of magical powers, such as being able to fly. If taken in a large enough dose, the drug produces delusions and visual hallucinations. The user’s sense of time and self changes.  Many LSD users experience flashbacks, recurrence of certain aspects of a person’s experience, without having taken the drug again. A flashback comes suddenly, often without warning, and may be within a few days or more than a year after LSD use.
Many LSD users experience flashbacks, recurrence of certain aspects of a person’s experience, without having taken the drug again. A flashback comes suddenly, often without warning, and may be within a few days or more than a year after LSD use.  The physical effects from LSD
The physical effects from LSD Severe adverse effects include terrifying thoughts and feelings and despair, occasionally leading to fatal accidents.
Severe adverse effects include terrifying thoughts and feelings and despair, occasionally leading to fatal accidents. MDMA (ecstasy) affects dopamine-containing neurones that use the chemical serotonin to communicate with other neurones; a decrease in serotonin transporters has been recently demonstrated in the brain of MDMA users by positron emission tomography (PET)
MDMA (ecstasy) affects dopamine-containing neurones that use the chemical serotonin to communicate with other neurones; a decrease in serotonin transporters has been recently demonstrated in the brain of MDMA users by positron emission tomography (PET)  Ecstasy, like amphetamines, produces euphoria and appetite suppression, but is more potently hallucinogenic, possibly because of chemical affinities with mescalin.
Ecstasy, like amphetamines, produces euphoria and appetite suppression, but is more potently hallucinogenic, possibly because of chemical affinities with mescalin.  It is usually taken by mouth, producing effects after 20-60 minutes
It is usually taken by mouth, producing effects after 20-60 minutes  Adverse effects of MDMA are not dose-related, and include: • psychiatric sequelae such as agitation or paranoia • neurological effects such as ataxia and seizures • cardiovascular such as tachycardia, arrhythmias or infarction • renal or hepatic failure • other effects
Adverse effects of MDMA are not dose-related, and include: • psychiatric sequelae such as agitation or paranoia • neurological effects such as ataxia and seizures • cardiovascular such as tachycardia, arrhythmias or infarction • renal or hepatic failure • other effects  MDMA users face risks similar to those found with the use of cocaine and amphetamines: • psychological difficulties, including confusion, depression, sleep problems, drug craving, severe anxiety, and paranoia – during and sometimes weeks after taking MDMA • physical symptoms such as muscle tension, involuntary teeth clenching, nausea, blurred vision, rapid eye movement, faintness, and chills or sweating • raised heart rate and blood pressure, a special risk for people with circulatory or heart disease
MDMA users face risks similar to those found with the use of cocaine and amphetamines: • psychological difficulties, including confusion, depression, sleep problems, drug craving, severe anxiety, and paranoia – during and sometimes weeks after taking MDMA • physical symptoms such as muscle tension, involuntary teeth clenching, nausea, blurred vision, rapid eye movement, faintness, and chills or sweating • raised heart rate and blood pressure, a special risk for people with circulatory or heart disease  There is evidence that people who develop a rash that looks like acne after using MDMA may be risking severe side effects, including liver damage, if they continue to use the drug.
There is evidence that people who develop a rash that looks like acne after using MDMA may be risking severe side effects, including liver damage, if they continue to use the drug. Work absenteeism, frequent disappearances from the workplace, making improbable excuses and taking frequent or long trips to the toilet or to the stockroom where drugs are kept
Work absenteeism, frequent disappearances from the workplace, making improbable excuses and taking frequent or long trips to the toilet or to the stockroom where drugs are kept  Personality change – mood swings, anxiety, depression, lack of impulse control, suicidal thoughts or gestures, and deteriorating interpersonal relations with colleagues and staff; the user rarely admits errors or accepts blame for errors or oversights
Personality change – mood swings, anxiety, depression, lack of impulse control, suicidal thoughts or gestures, and deteriorating interpersonal relations with colleagues and staff; the user rarely admits errors or accepts blame for errors or oversights  Unreliability in keeping appointments, meeting deadlines, and work performance – which alternates between periods of high and low productivity. Many suffer from mistakes made due to inattention, poor judgment, bad decisions, confusion, memory loss, and difficulty concentrating or recalling details and instructions. Ordinary tasks require greater effort and consume more time.
Unreliability in keeping appointments, meeting deadlines, and work performance – which alternates between periods of high and low productivity. Many suffer from mistakes made due to inattention, poor judgment, bad decisions, confusion, memory loss, and difficulty concentrating or recalling details and instructions. Ordinary tasks require greater effort and consume more time.  Progressive deterioration in personal appearance and hygiene, and uncharacteristic deterioration of handwriting and charting
Progressive deterioration in personal appearance and hygiene, and uncharacteristic deterioration of handwriting and charting  Other common signs are: • tachycardia (amphetamines) • hyperpyrexia (ecstasy) • bruxism – amphetamines or ecstasy • drug-associated diseases • psychosis.
Other common signs are: • tachycardia (amphetamines) • hyperpyrexia (ecstasy) • bruxism – amphetamines or ecstasy • drug-associated diseases • psychosis. Amphetamines have no true withdrawal syndrome and, in this respect, amphetamine addiction is quite different from opioid or barbiturate dependence
Amphetamines have no true withdrawal syndrome and, in this respect, amphetamine addiction is quite different from opioid or barbiturate dependence  LSD is not considered an addictive drug since it does not produce compulsive drug-seeking behaviour as do cocaine, amphetamine, heroin, alcohol, and nicotine; most users of LSD voluntarily limit or stop its use over time
LSD is not considered an addictive drug since it does not produce compulsive drug-seeking behaviour as do cocaine, amphetamine, heroin, alcohol, and nicotine; most users of LSD voluntarily limit or stop its use over time  After long-term use of ecstasy, tolerance develops but there is neither physical dependence nor withdrawal symptoms.
After long-term use of ecstasy, tolerance develops but there is neither physical dependence nor withdrawal symptoms. Bruxism may result from chronic amphetamine use
Bruxism may result from chronic amphetamine use  There can be xerostomia and greater caries incidence.
There can be xerostomia and greater caries incidence. Jaw clenching appears to be common
Jaw clenching appears to be common  Bruxism, TMJ dysfunction, dry mouth, attrition, erosion, mucosal burns or ulceration and periodontitis have been reported.
Bruxism, TMJ dysfunction, dry mouth, attrition, erosion, mucosal burns or ulceration and periodontitis have been reported. has subjective symptoms of dental pain, with no objective evidence of the disorder
has subjective symptoms of dental pain, with no objective evidence of the disorder  makes a self-diagnosis and requests a specific drug, especially a psychoactive agent
makes a self-diagnosis and requests a specific drug, especially a psychoactive agent  appears to have a dramatic but unexpected complaint such as trigeminal neuralgia
appears to have a dramatic but unexpected complaint such as trigeminal neuralgia  firmly rejects treatments that exclude psychoactive />
firmly rejects treatments that exclude psychoactive />