Immunity and Immunologic Oral Lesions
Margaret J. Fehrenbach, Joan Andersen Phelan and Olga A.C. Ibsen
After studying this chapter, the student will be able to:
1. Define and pronounce each of the words in the vocabulary list for this chapter.
2. Describe the differences between an immune response and an inflammatory response.
3. List and describe the two main types of lymphocytes, including their origins and activities.
4. List and describe the different types of T-cell lymphocytes and their functions.
5. Describe the origin of macrophages and list their activities in the immune response.
6. Describe the differences between humoral immunity and cell-mediated immunity and include the cells involved in each.
7. Describe the differences between passive and active immunity and give an example for each type of immunity.
8. List and describe four types of hypersensitivity reactions and give an example for each type of hypersensitivity.
9. Describe the process of autoimmunity and how it results in disease.
10. Describe the process of immunodeficiency and how it results in disease.
11. Describe and contrast the clinical features of each of the three types of aphthous ulcers.
12. List systemic diseases associated with aphthous ulcers.
13. Describe and compare the clinical features of urticaria, angioedema, contact mucositis, and fixed drug eruption.
14. Describe the clinical features of erythema multiforme and Stevens-Johnson syndrome.
15. Describe the clinical and microscopic features of lichen planus.
16. List the triad of systemic signs that comprise reactive arthritis (Reiter syndrome) and describe the oral lesions that occur in this condition.
17. Name the two cells that characterize Langerhans cell disease microscopically. Describe the acute disseminated form, chronic disseminated form, and chronic localized form and state the names that traditionally have been used for each of these conditions.
18. Describe the oral manifestations of each of the following autoimmune diseases: lupus erythematosus, pemphigus vulgaris, mucous membrane pemphigoid, and Behçet syndrome.
19. Define desquamative gingivitis, describe the clinical features, and list three diseases in which desquamative gingivitis may occur.
The inflammatory response, as described in Chapter 2, is a rapid first line of defense against injury. The immune response, described in this chapter, follows the inflammatory response and is necessary for complete recovery. This chapter begins with a description of the acquired immune response and then includes a discussion of the most commonly encountered oral diseases that may result from harmful effects of such a response. Surveillance against neoplastic cells also involves the immune response and is described, along with the neoplastic process and neoplastic oral lesions, in Chapter 7.
Acquired Immune Response
Like the inflammatory response, the acquired immune response defends the body against injury, particularly from foreign substances such as microorganisms. The immune response differs from the inflammatory response in that it has the capacity for memory and responds more quickly to a foreign substance if encountered again. It works amid the background of an already activated inflammatory response and innate immune response, as well as a working repair process. The innate immune response does not involve memory and is described, along with inflammation, in Chapter 2. In contrast, the acquired immune response involves a complex network of white blood cells. Similar to the inflammatory response, the immune response may also result in an increased level of tissue damage and disease as it fights against what it considers foreign.
Cellular Involvement in the Immune Response
B-Cell Lymphocyte
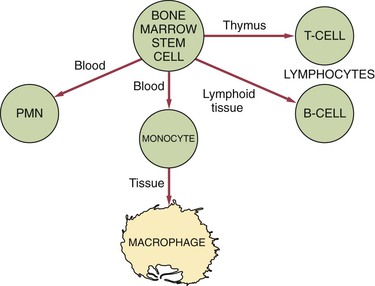
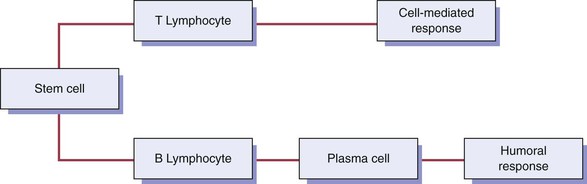
The B-cell lymphocyte (B cell) develops from a stem cell in the bone marrow and then resides and matures in lymphoid tissue (Figure 3-1). When antigen stimulates a B cell, the B cell travels to the site of the injury. Two main types of B cells develop when stimulated by an antigen: (1) the B-memory cell and (2) the plasma cell.
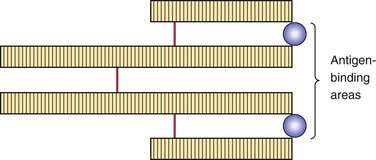
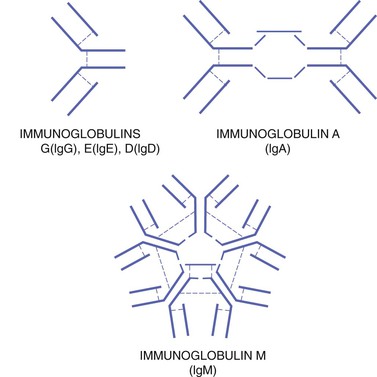
The plasma cell has a round, pinwheel-shaped nucleus and visible cytoplasm. The plasma cell produces and releases many copies of a particular protein (antibody) in response to the presence of antigen. Antibodies circulating within the blood serum are considered immunoglobulins. Five different general types of immunoglobulins exist: (1) IgA, (2) IgD, (3) IgE, (4) IgG, and (5) IgM (Table 3-1). They all are variations of the same basic structure (Figures 3-2 and 3-3). Each immune response involves specific antibodies produced in response to a specific antigen by a specific plasma cell. This specificity is a characteristic function of the immune response. The level of a specific antibody in the blood is called the antibody titer. This can be measured by diagnostic laboratory tests and is useful in the diagnosis and evaluation of infectious disease.
TABLE 3-1
| IMMUNOGLOBULIN (IG) | DESCRIPTION |
| IgA | Has two subgroups: serous in the blood and secretory in the saliva and other secretions such as tears and breast milk; aids in defense against proliferation of microorganisms in body fluids as well as protecting mucosal sites (e.g., gastrointestinal and genitourinary tracts) |
| IgD | Functions in the activation of B-cell lymphocytes, because it is found on their surface, but full role is unclear |
| IgE | Involved in hypersensitivity or allergic reactions because it can bind to mast cells and basophils to bring about the release of biochemical mediators such as histamine; and also attacks parasites |
| IgG | Major antibody in blood serum (about 75%); can pass the placental barrier, produced in secondary immune response, and serves as the first passive immunity for the newborn |
| IgM | Involved in early immune responses because of its involvement with IgD in the activation of B-cell lymphocytes, activates complement, and reacts to blood group antigens |
T-Cell Lymphocyte
After it develops from a bone marrow stem cell, the T-cell lymphocyte (T cell) travels to the thymus and is processed into a mature cell (see Figure 3-1). The thymus is a primary lymphoid organ located high in the chest. It is quite large in infants and shrinks as an individual matures.
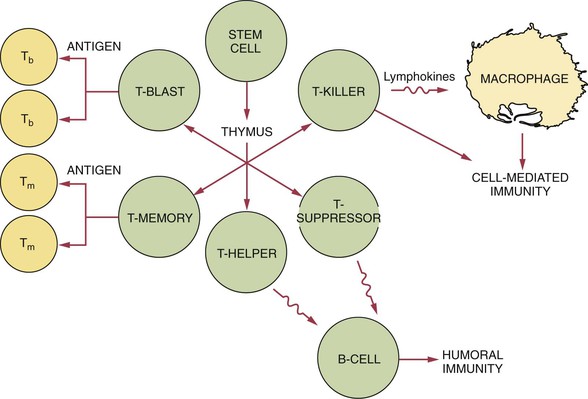
The T-helper cell increases the functioning of the B-cell, enhancing the antibody response. It is easily identifiable by the CD4 cell receptor on its surface (Figure 3-4). The T-suppressor cell (or T-regulator cell) carries the CD8 marker as well as other markers on its surface and suppresses the functioning of the B cell.
Macrophage
Not only is the white blood cell macrophage present in the connective tissue during inflammation, it is also involved in the evolving immune response to an antigen as an accessory cell (see Figure 3-1). The macrophage is active in phagocytosis of foreign substances and also assists both the B-cell and T-cell during the immune response.
The macrophage carries receptors for lymphokines produced by the lymphocytes, which allow it to be activated into a single-minded pursuit of specific foreign material such as microorganisms or neoplastic cells (Table 3-2). When activated, the macrophage can function in many other different ways, always amplifying the immune response. Unlike lymphocytes, the macrophage does not retain memory of an encountered antigen and needs to be reactivated during each encounter.
TABLE 3-2
| CYTOKINE | FUNCTION |
| Interferons | Various functions involving leukocytes, fibroblasts, and endothelial cells |
| Interleukins | Stimulate leukocyte proliferation and other functions |
| Lymphotoxin | Destroys fibroblasts |
| Macrophage-activating factor | Activates macrophages to produce and secrete lysosomal enzymes |
| Macrophage chemotactic factor | Stimulates macrophage emigration |
| Migration inhibitory factor | Inhibits macrophage activity |
| Tumor necrosis factor | Various functions involving leukocytes and fibroblasts |
Cytokines
Cytokines are proteins that are made by cells and are able to affect the behavior of other cells; thus they are considered immunomodulating agents. Immunomodulating agents, or immunomodulators, alter the immune response by augmenting or reducing the functions of the response. Cytokines are produced by the cells of the immune system and play a prominent role in the activation of the immune response. They are one way that lymphocytes communicate with each other and with other immune system cells. B cells and T cells produce their own cytokines, called lymphokines, in varying levels (see Figure 3-4).
Different cytokines have differing functions within the immune response (see Table 3-2). They can activate macrophages and enhance the ability of macrophages to destroy foreign cells. These types of cytokines may also be involved in various other functions concerning leukocytes, fibroblasts, and endothelial cells. They are also responsible for the systemic effects of inflammation such as loss of appetite and increased heart rate. Monocytes/macrophages produce their own cytokines, called monokines. Dendritic cells, such as the Langerhans cells, also produce and react to cytokines.
Major Divisions of the Immune Response
There are two major divisions of the immune response: (1) humoral immunity and (2) cell-mediated immunity (Figure 3-5). These two divisions differ in their reaction to an antigen. However, these divisions are interrelated, and present understanding of the immune response recognizes that these divisions do not function as distinctly separate mechanisms.
Immunopathology
Hypersensitivity
Hypersensitivity or allergy comprises the same basic types of reactions that occur when the immune response is fighting microorganisms and protecting the body against disease. However, these hypersensitivity or allergenic reactions are exaggerated immune responses causing an immunopathologic condition, along with tissue destruction. Four main types of hypersensitivity reactions occur; they are classified by the nature of the immune response that causes the disease (Table 3-3).
TABLE 3-3
| TYPE OF REACTION | EXAMPLE(S) |
| Type I or anaphylactic type | Hay fever, asthma, anaphylaxis |
| Type II or cytotoxic type | Autoimmune hemolytic anemia |
| Type III or immune complex type | Autoimmune diseases such as systemic lupus erythematosus |
| Type IV or cell-mediated type | Granulomatous diseases such as tuberculosis as well as graft and organ transplant rejection |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
) )
)